A 14-Year-Old Girl with Adolescent Idiopathic Scoliosis
October 6, 2021
A 14-year-old girl previously diagnosed with adolescent idiopathic scoliosis presented to our institution for consultation with regard to operative treatment of scoliosis. Her spinal curvature was first noticed by her mother 5 years before presentation and had been managed with a thoracolumbosacral orthosis. However, her curve progressed to the point that it required a surgical procedure. Her preoperative physical examination showed uneven shoulder levels (right higher than the left), right rib prominence on Adam’s forward bend test, and a 25° thoracic trunk rotation measured by a scoliometer.
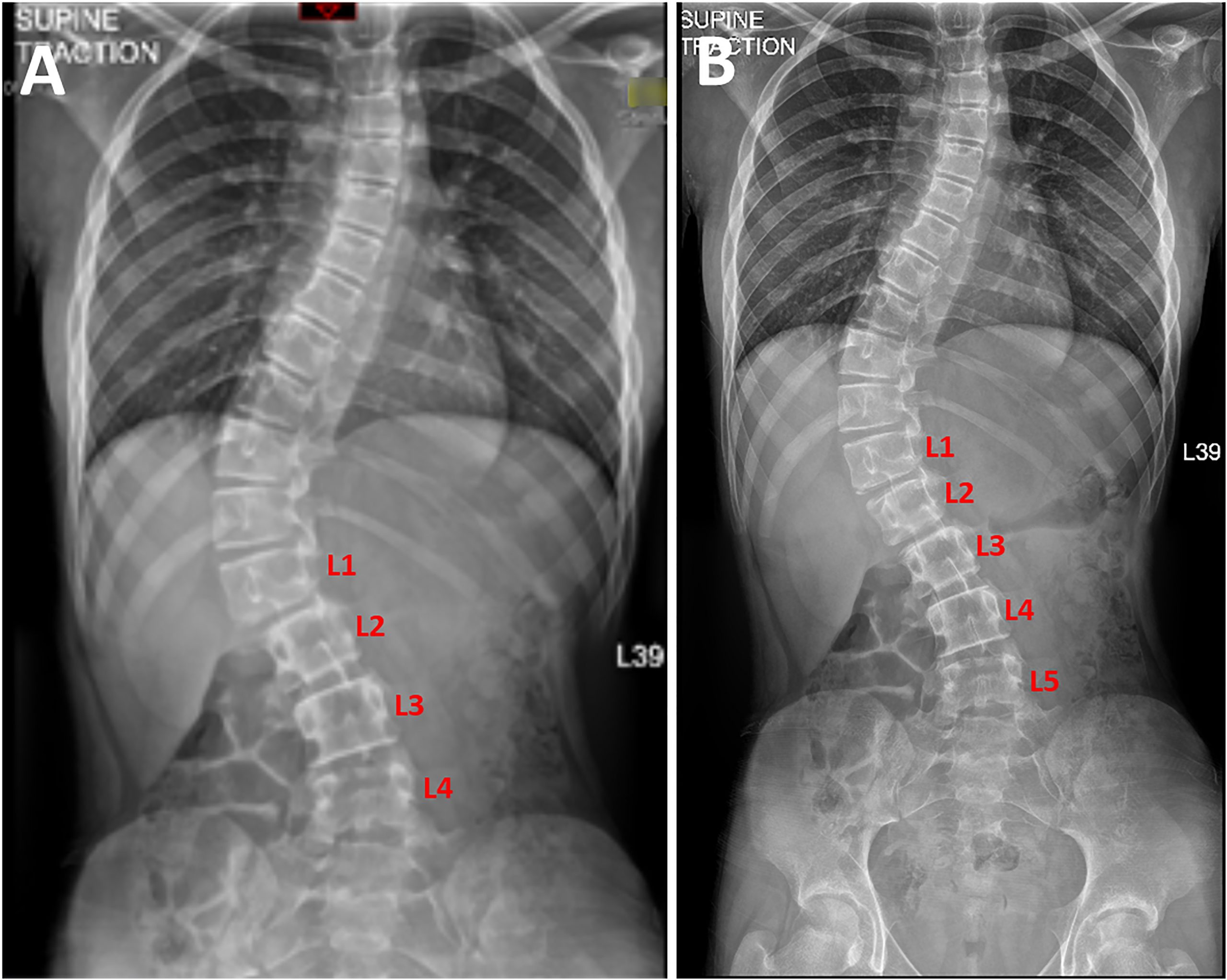
Per routine practice, standard posteroanterior and lateral standing and traction spine radiographs were obtained to guide preoperative planning. The standing views demonstrated an 82° thoracolumbar curve with an apex at T12, 5 lumbar vertebrae, and a grade-0 Risser sign (Fig. 1). However, the patient’s traction radiograph showed only 4 lumbar vertebrae.
The AccE GC85A digital radiography system (Samsung Electronics) had been used to stitch the source images captured by the radiology technician. The images are stitched automatically. It was noticed that there was a missing vertebra in the traction radiograph (Fig. 2-A); the missing vertebra was determined to be the result of a technical stitching error that was later corrected (Fig. 2-B).
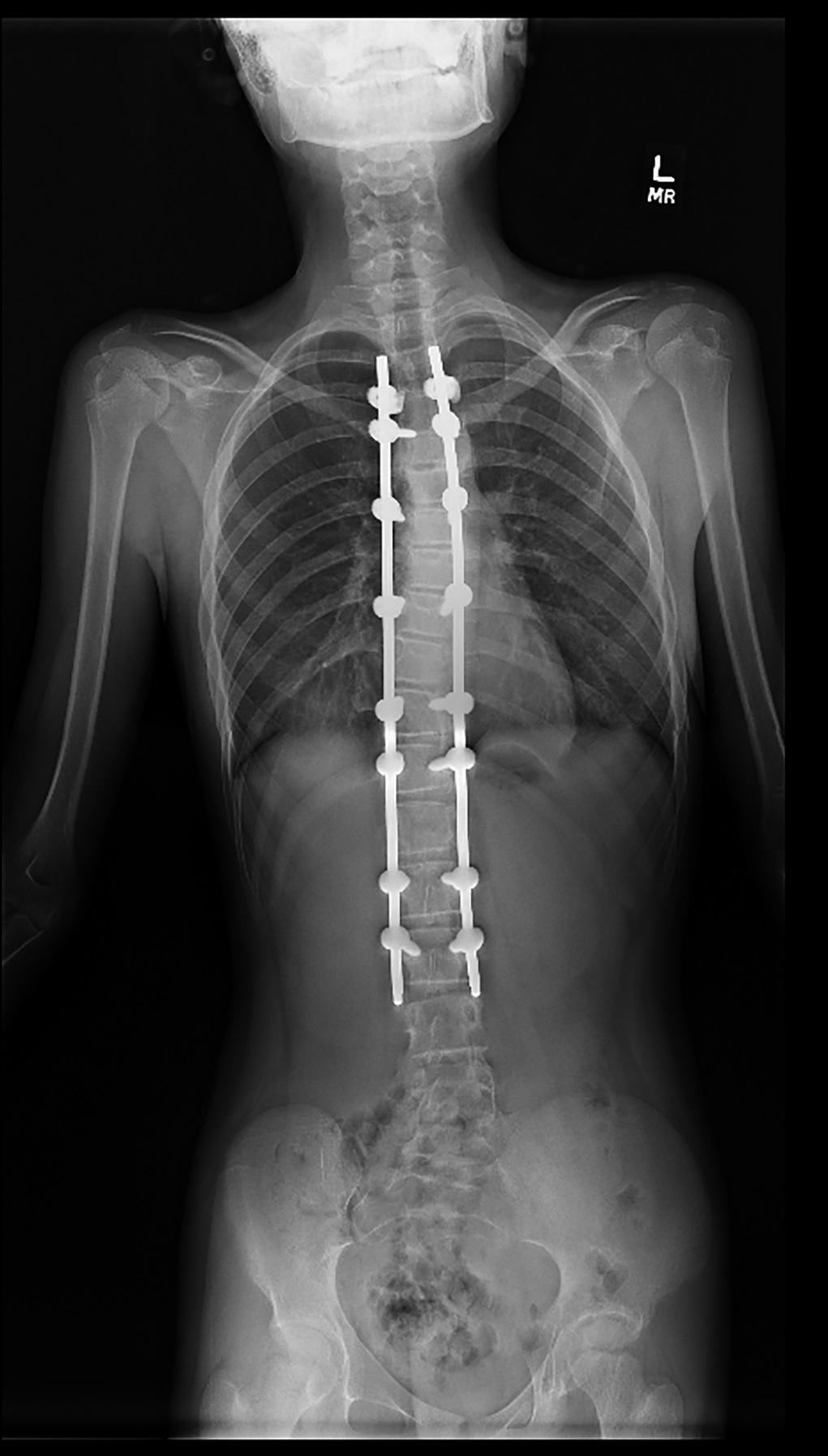
The patient underwent uneventful posterior spinal arthrodesis from T4 to L3 (Fig. 3). She was discharged from the hospital on postoperative day 3 and, by 4 months after the surgical procedure, had had an uncomplicated recovery course.
An example of image stitching is shown in Figures 4-A and 4-B.
Proceed to Discussion >>Reference: Ikwuezunma I, Fayad LM, Sponseller PD. Case of the missing vertebra: a report of a radiographic stitching error in a scoliosis patient. JBJS Case Connect. 2021 Jul 6;11(3):e21.00295.
Contemporary scoliosis studies use digital radiography, which involves image processing and analytic algorithms to render a single panoramic image for clinical application. Notably, current digital imaging systems cannot capture the entire spine in a single scan because of the limited field of the imaging detector. Hence, multiple exposures with spatial overlap are required to generate a composite image. In the case of scoliosis radiographs, the thoracic spine and the lumbar spine are scanned in a series as 2 separate images of the upper torso and the lower torso with an overlapping region between the 2 images, which are then stitched together.
Image stitching consists of 2 fundamental steps: image registration and blending. Image registration describes the transformation of ≥2 sets of image data into 1 coordinate system (i.e., the alignment of multiple images of the same scene). This process uses the overlapping regions of the image sets to find the merge position and transformation that provide the optimal configuration (Fig. 4-A). After successful registration, the intensity of the images in the overlapping region is smoothly adjusted, or blended, to remove seams and discontinuities. The composite image is then exported to the picture archiving and communication system as a single-view image displaying the entire thoracic spine and lumbar spine (Fig. 4-B). Several strategies have been described to facilitate this process, including the placement of a radiodense ruler parallel to the long axis in the backdrop or the attachment of a grid of attenuating lines to the imaging detector.
Despite ongoing technological advances, no method is 100% accurate. Digital stitching poses several challenges and is susceptible to technical errors, including image noise, motion artifact, intensity variation, and image disorientation. Consequently, stitching errors may lead to a false diagnosis of spinal abnormalities or may potentially hide real structural abnormalities. As a result, such errors may lead to increased patient morbidity, misallocated resources, and unnecessary health-care costs. Here, we describe a near-miss event demonstrating the seamless mechanical elimination of a lumbar vertebra in the traction view.
Radiographic parameters form the basis of evaluation and treatment of scoliosis by providing the most reliable means of assessing disease and risk and helping to guide clinical decision-making. Modern digital radiography of scoliosis studies has substantially enhanced the clinic workflow through rapid image acquisition, reduced patient-motion artifact, ease of digital measurement, and efficient distribution. However, current automated systems are not free from error.
This report describes a patient with adolescent idiopathic scoliosis who presented for preoperative evaluation and nearly underwent incorrect-level selection because of a mistaken impression of the actual number of lumbar vertebrae after a digital radiograph stitching error. In her case, the timely identification of this error led to the correct-level selection for spinal arthrodesis, which had important clinical implications. Erroneous radiographic imaging can result in a wrong-level surgical procedure.
The research with regard to technical errors of digital radiograph stitching is scarce. One case series from Australia described 4 instances of digital stitching errors in limb-length and scoliosis radiographs. One incident nearly prompted an unnecessary surgical procedure after imaging in a patient with chronic back pain erroneously displayed broken rods. To date, we are aware of only 1 other study that reported the incidence of anatomical errors produced by digitally stitched scoliosis studies. Supakul et al. retrospectively reviewed 86 consecutive adolescent idiopathic scoliosis studies performed during a 2-month period. They detected an overall radiograph stitching error rate of 16% (14 of 86 patients). They similarly detected a 14% (2 of 14 patients) stitching error rate in children with spinal implants for adolescent idiopathic scoliosis. After analysis, they reported no significant difference in error rate in the presence or absence of spinal implants or between erect and supine patient positioning.
Various algorithms have been designed to enhance the digital stitching of radiographs, most of which can be categorized into 1 of 2 approaches: direct-based and feature-based. Direct-based registration represents the classic method involving the pixel-to-pixel comparison of ≥2 images with specific error criteria to find the parametric transformation that provides optimal alignment. Direct-based methods facilitate accurate registration by using all available imaging data within the images’ overlapping regions, albeit at the expense of increased computational time. Alternatively, more recent algorithms commonly use feature-based alignment methods that extract the distinctive features from each image (e.g., corner detectors invariant to image rotation, scaling, or intensity discrepancies) to match those features to establish global correspondence and approximate the motion transformation between the images. As a result, feature-based methods are more robust against scene movement and provide faster stitching results compared with direct methods.
Although seldom reported, digital stitching errors are potentially consequential. Despite ongoing technological advancements, clinicians must remain vigilant when reviewing digitally stitched images. Technicians, radiologists, and orthopaedic surgeons should be trained to detect radiograph stitching errors to minimize complications. Given that most imaging systems that incorporate these stitching techniques provide the end user with the 2 source images in addition to the final stitched image, it is imperative that the reviewing clinician take time to scan the individual source images for discrepancies that may result from stitching errors. We propose that radiographers should clearly label that an image has been stitched and indicate the overlapping region of each exposure on the stitched radiograph. We advise correlating composite images with source images and screening for soft-tissue mismatch or misaligned margins.
Reference: Ikwuezunma I, Fayad LM, Sponseller PD. Case of the missing vertebra: a report of a radiographic stitching error in a scoliosis patient. JBJS Case Connect. 2021 Jul 6;11(3):e21.00295.
What is the interpretation?
The standing scoliosis radiograph being from a different patient than the traction radiograph
An apparently missing vertebra in the traction radiograph due to a technical stitching error by the imaging software
The T11 vertebra on the standing radiograph being misinterpreted as T12
The T12 vertebra on the traction radiograph being misinterpreted as L1
Idiopathic vertebral hypoplasia at L5


 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4