A 67-year-old man presented to the emergency department reporting fever, malaise, and left lower-extremity pain. He stated that, at 6 weeks before presentation, he started having nonspecific atraumatic leg pain and was subsequently found to have an occlusive deep venous thrombosis in the left femoral, popliteal, posterior tibial, and peroneal veins and was ultimately discharged with instructions to take oral anticoagulation. The patient continued to have an increase in pain and was unable to ambulate, so he presented to the emergency department. A computed tomographic (CT) pulmonary embolism torso study was ordered to rule out pulmonary embolus (Fig. 1).
On examination, the patient was found to have diffuse swelling of the left lower extremity extending to the ankle. He also was found to have an area of fluctuance over the medial left knee and severe pain with both active and passive motion. Joint aspiration of the knee produced 40 mL of fluid. A CT scan of the left lower extremity demonstrated peripherally enhancing multilocular complex fluid collections throughout the deep spaces of the thigh (Fig. 2) and heterogenous intramedullary findings with extensive micronodular erosion of the cortex about the left femoral diaphysis (Fig. 3).
The radiographic studies were interpreted as showing soft-tissue fluid collections and intraosseous air, most consistent with osteomyelitis caused by a gas-forming organism (emphysematous osteomyelitis).
A standard knee arthrotomy, along with exploration of the lateral and posterior compartments of the thigh, was performed the following day. Compartments were irrigated with sterile saline using pulse lavage. The femoral canal was accessed with multiple lateral drill holes using a 4.5-mm drill-bit to allow drainage. The final lavage was performed with 3 L of saline with vancomycin and gentamicin for coverage of gram-positive, gram-negative, and anaerobic bacteria. Over 3 L of atypical gray, dishwater-colored purulence was evacuated.
The patient initially improved but required an additional debridement with evacuation of another 2 L of purulent fluid from the compartments of the thigh. Retrograde debridement of the femoral canal was performed using a Reamer/Irrigator/Aspirator (DePuy Synthes).
After the second operation, the patient’s condition improved substantially. The initial cultures were negative after 5 days. Due to the atypical appearance of the fluid, culture specimens were kept in the laboratory for 15 days. On postoperative day 9, Parvimonas micra grew on the intramedullary cultures. Given that this was likely from hematogenous seeding of the bone, upon further evaluation, the patient was found to have a chronic dental abscess of the 27th tooth (the offending organism was unknown), for which he had been taking amoxicillin. He continued to improve and was ultimately discharged home with a 6-week course of intravenous metronidazole (500 mg every 8 hours) and ceftriaxone (2 g daily), with future procedures dependent on his clinical course. Antibiotic susceptibility reports were not provided, so antibiotic choice was based on infectious disease recommendations. Their decision was based on local antibiogram information showing particular susceptibility to beta-lactam antibiotics and metronidazole and the infectious disease literature.
The patient improved initially with new bone formation noted through the diaphysis on femoral radiographs at 8 weeks. His inflammatory markers (white blood cell count, erythrocyte sedimentation rate, and C-reactive protein) eventually plateaued, and repeat imaging with magnetic resonance imaging (MRI) showed a distal metaphysis abscess and ongoing active osteomyelitis (Fig. 4). Approximately 5 months after his initial presentation, the patient underwent repeat debridement with a Reamer/Irrigator/Aspirator and underwent placement of an antibiotic rod within the femoral canal using tobramycin cement and 2 g of ceftriaxone. Again, the antibiotic choice was empiric and was chosen to cover a broad spectrum of organisms, including P. micra, in the absence of updated culture results. After debridement of the femoral metaphysis, the resulting defects were packed with antibiotic beads and the bone window was sealed with antibiotic cement (Fig. 5). The patient’s inflammatory markers subsequently improved, and his treatment eventually transitioned from intravenous antibiotics to suppressive oral therapy with doxycycline 100 mg twice per day indefinitely. The antibiotic choice was based on broad spectrum of coverage in the absence of updated culture results, favorable side effect profile, and patient convenience.
Three months later, the patient fell and sustained a mildly displaced midshaft femoral fracture without disrupting the antibiotic rod (Fig. 6). At that time, the antibiotic rod was removed and replaced with a retrograde intramedullary femoral nail (Fig. 7). At the 14-month follow-up, the patient showed no signs of recurrent infection and had made a full functional recovery. He was to be followed on an as-needed basis.
Proceed to Discussion >>Reference: Ghosen J, Lucasti C, Daoust S. Parvimonas micra causing emphysematous osteomyelitis: a case report. JBJS Case Connect. 2022 Oct 14;12(4):e22.00247.
The first case of emphysematous osteomyelitis was described in the literature in 1981 when intraosseous gas was noticed on CT scans. In the appropriate clinical setting and in patients with no other viable cause, intraosseous gas is highly indicative of emphysematous osteomyelitis. The presence of gas is likely explained by the metabolic activity of anaerobic bacteria in the medullary cavity. This is a serious and often fatal condition with mortality rates between 32% and 34% and as high as 50% for spinal column infections.
Emphysematous osteomyelitis is a rare condition, with fewer than 60 cases described in the literature. Diabetes mellitus has been found to be the most common predisposing condition, followed by neoplasia and hematologic disorders, although there have been several cases described in previously healthy individuals. Emphysematous osteomyelitis has been known to affect foci throughout the axial skeleton; however, it most commonly affects the vertebral bodies, followed by the pelvis and femur. In addition, emphysematous osteomyelitis has recently been found to occur concurrently with emphysematous pyelonephritis. The route of infection is usually hematogenous but can be a postoperative complication or from an abdominal fistula. Although typical osteomyelitis has been shown to have a male predominance at a rate of nearly 2:1, emphysematous osteomyelitis does not share the same distribution, with no correlation shown between sexes.
The diagnosis of emphysematous osteomyelitis is generally reliant on CT scans. The role of ultrasonography is limited, and, although MRI scans can detect intraosseous gas, CT scans are generally believed to be more sensitive. An intraosseous gas pattern called the “pumice stone” sign on CT imaging has been seen in 96% of cases, making for a sensitive indicator on imaging studies.
Treatment management should be prompt and generally will involve surgical intervention and antibiotic therapy. The general approach entails a 4 to 6-week course of broad-spectrum antibiotics with tailored therapy once the microbes have been isolated.
Therapy for emphysematous osteomyelitis with an intramedullary antibiotic spacer has previously been described and was similar to the one used in this case. Given the favorable outcome in this case, we recommend aggressive treatment with an antibiotic spacer using the same technique.
Although there has not been a case of P. micra emphysematous osteomyelitis described in the literature, there are several instances of musculoskeletal infection including spondylodiskitis, septic arthritis, and typical osteomyelitis. This patient developed a massive deep vein thrombosis in the involved extremity. This may be secondary to a period of bed rest after the onset of pain, but there has been a correlation reported between P. micra and deep vein thrombosis.
In summary, emphysematous osteomyelitis is a rare and dangerous condition that should be managed aggressively with a surgical procedure. Using a Reamer/Irrigator/Aspirator in a retrograde fashion is a viable option for the debridement of the canal. Surgeons should recognize that irrigation and debridement alone may not be sufficient to achieve complete resolution of this condition and should not hesitate to proceed with more definitive management such as the placement of an antibiotic spacer, as was done in this case.
Reference: Ghosen J, Lucasti C, Daoust S. Parvimonas micra causing emphysematous osteomyelitis: a case report. JBJS Case Connect. 2022 Oct 14;12(4):e22.00247.
What is the diagnosis?
Compartment syndrome related to occlusive deep venous thrombosis
Rhabdomyolysis
Emphysematous osteomyelitis
Echinococcosis
Probable mycobacterial infection

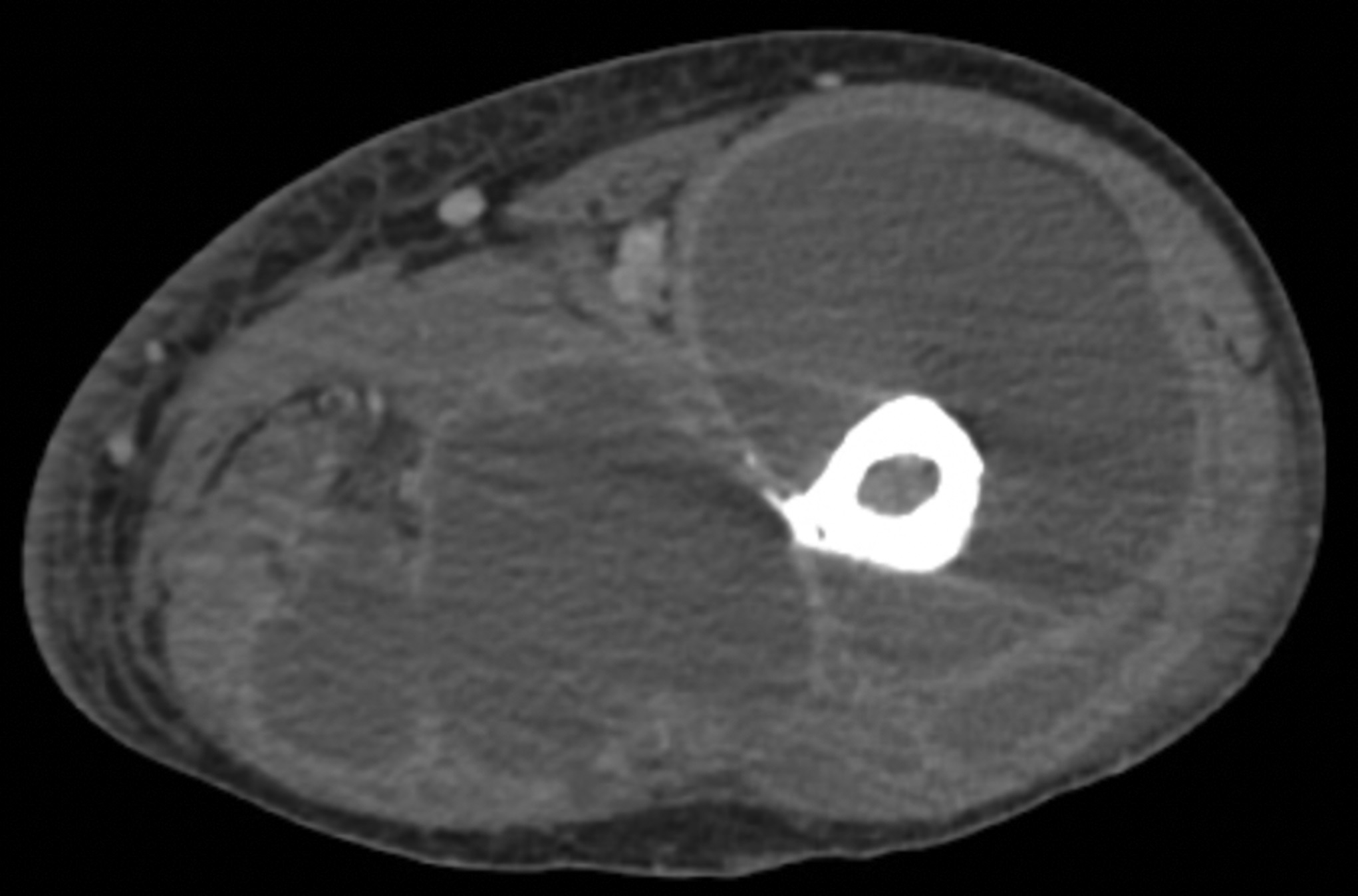
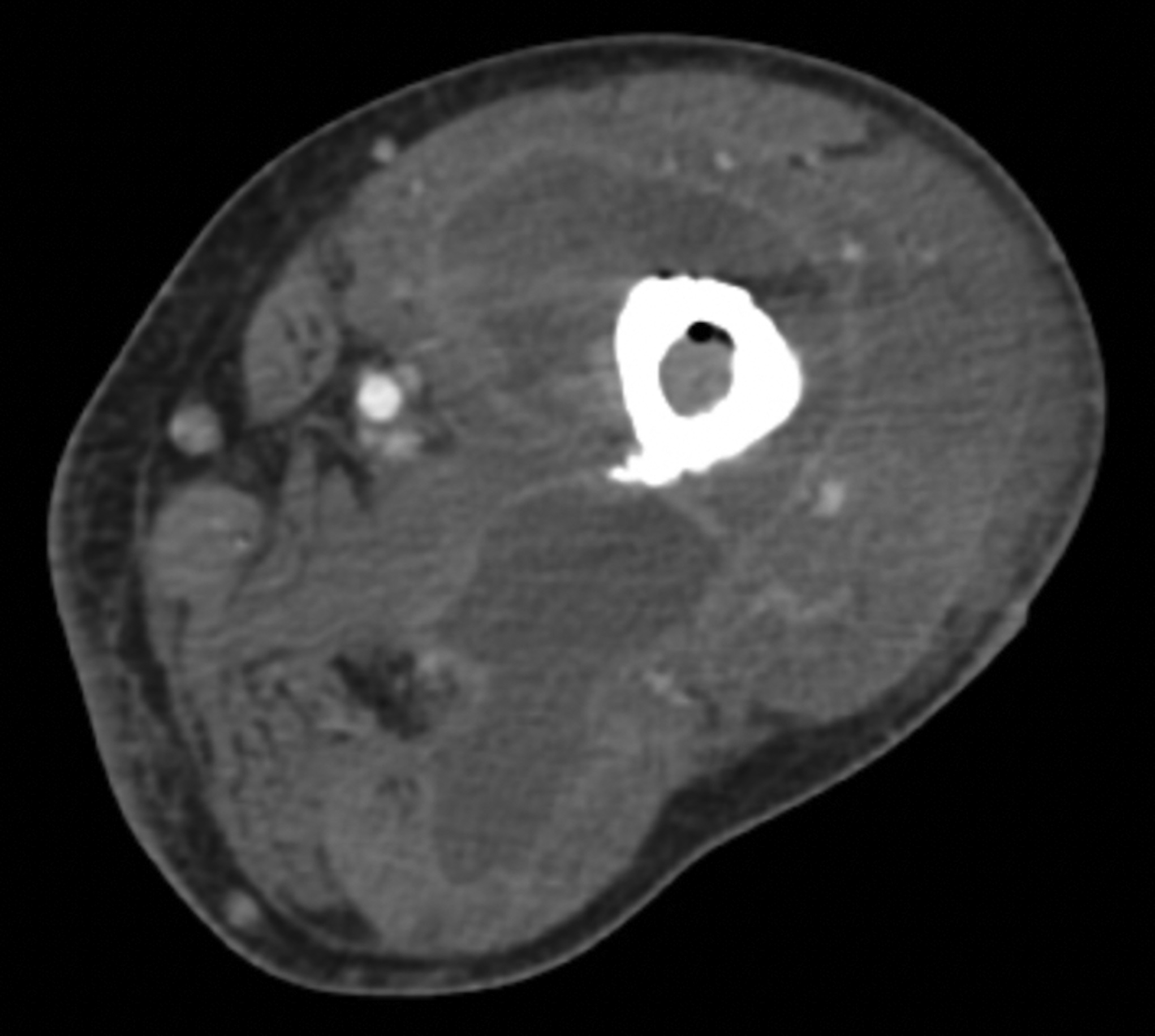

 Fig. 1
Fig. 1 Fig. 2
Fig. 2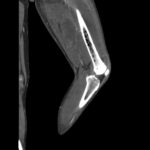 Fig. 3
Fig. 3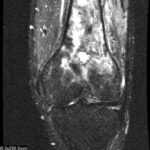 Fig. 4
Fig. 4 Fig. 5
Fig. 5 Fig. 6
Fig. 6 Fig. 7
Fig. 7


