A 64-year-old man with a 40-pack-year smoking history (he had stopped smoking 5 years earlier), hypertension, diabetes mellitus type II, hyperlipidemia, obesity, and pulmonary embolism was referred to our clinic for the evaluation of persistent medial left knee pain and an apparent periprosthetic fracture. He had undergone revision total knee arthroplasty (TKA) for aseptic loosening at another institution 4 months previously. Before referral, he underwent a workup for infection that included serum markers and fluoroscopically guided aspiration, reportedly within normal limits. However, the fluoroscopy reportedly highlighted a medial femoral condyle fracture, which, together with the persistent pain, prompted the referral to this center. On presentation at our clinic, there was notable focal tenderness over the left medial femoral condyle on the initial physical examination. Radiographs demonstrated a well-positioned, well-fixed prosthesis without obvious fractures (Fig. 1). The patient was prescribed nonsteroidal anti-inflammatory drugs and was instructed to return for follow-up.
At a follow-up appointment 3 months after the initial evaluation at our clinic, the patient reported no changes in symptoms. Repeat physical examination and radiographs were similarly unremarkable. The patient requested conservative management and was referred to interventional pain management. Diagnosed initially with complex regional pain syndrome, he underwent spinal cord stimulation at the left L3-4 dorsal root ganglion. The patient reported an immediate reduction in left knee pain after the spinal cord stimulation trial and later underwent final implantation of the spinal cord stimulation device.
At 7 months after his initial visit, the patient experienced a pop in the left knee while walking. It was followed by an acute increase in knee pain and repeated falls due to an inability to bear weight on the left extremity. When he presented to clinic, the radiograph of the left knee revealed substantial lysis along the medial aspect of the proximal left tibia (Fig. 2). Laboratory studies revealed an elevated C-reactive protein level (35.70 mg/L), an elevated erythrocyte sedimentation rate (55 mm/hour), and normal levels of gamma-globulin in protein electrophoresis. Whole-body positron emission tomography (PET) showed increased radiotracer uptake in the left proximal medial tibia and elsewhere (Fig. 3). Computed tomographic (CT) scans of the left knee revealed a 4-cm destructive lesion in the medial tibial condyle underlying the tibial tray (Fig. 4). Based on the imaging findings and due to concern for a periprosthetic infection, the patient underwent an intraoperative percutaneous biopsy of the tibial lesion with frozen section. This procedure was later followed by curettage.
The histology of the lesion from the biopsy is shown in Figure 5, and the histology of the lesion from curettage is shown in Figure 6.
The PET scan demonstrated a large lesion in the base of the right lung. The biopsies of the knee were interpreted as showing squamous carcinoma, consistent with metastatic carcinoma from the lung.
A subsequent lung biopsy was consistent with squamous cell carcinoma, confirming the origin of the tibial lesion. Because of the advanced staging of the malignancy, the patient was offered palliative care for both the primary and metastatic tumors with local radiotherapy to the tibia and palliative chemotherapy.
At a follow-up visit 3 months after excision and curettage with cementplasty (11 months after the initial visit), the patient reported that he was able to tolerate cancer treatments. Nonetheless, he required a wheelchair because of the limited mobility of the left knee and an inability to bear weight. Repeat radiographs of the left knee revealed a well-fixed total knee replacement with tibial cementation that did not require further surgical intervention (Fig. 7). The patient continued receiving palliative treatment at another institution until he died from complications of the malignancy at 7 months after the surgical intervention and a total of 15 months after the initial evaluation at this institution.
Proceed to Discussion >>Reference: Baez C, Nusbickel AJ, Knapik JA, Deen JT. Periprosthetic metastatic lung carcinoma about a total knee arthroplasty: a case report. JBJS Case Connector. 2022 Oct-Dec;12(4):e22.00350.
This case highlights metastasis as a source of unrelenting pain after revision TKA in a patient who had a previously unknown primary lung malignancy. The prevalence of individuals who undergo a TKA is an estimated 4.55% of the U.S. population older than 50 years of age. Furthermore, TKA volume is expected to grow by 143% by 2050. The most common failure modes associated with modern TKA include infection, instability, and stiffness. Metastasis and malignancy have not appeared among their more prevalent counterparts in systematic reviews of arthroplasty failure. Although bone is the third most common location for metastatic disease, the neoplastic etiology for arthroplasty failure and pain is exceedingly rare.
Similar to the current case, reported patients with periprosthetic metastasis have typically presented with unrelenting pain in the setting of revision arthroplasty believed to be due to aseptic loosening. It is of particular interest that this patient presented with constant pain and continuous falls due to difficulty bearing weight for 11 months before there was radiographic evidence of a permeative lytic lesion. Only a handful of cases have presented at pain onset with normal radiographic findings, followed by a rapid progression of osteolysis. Interestingly, the only other case that presented a similar period between pain onset and radiographic evidence of destruction was a squamous cell carcinoma of the lung with metastasis associated with a total hip arthroplasty. Nonetheless, osteolysis due to periprosthetic metastasis often presents at a relatively late stage of the disease, limiting options for intervention. The diagnosis of periprosthetic metastasis seems to be met by a grim prognosis, with a 7-month survival in this case and very similar survivals in other published cases ranging from 2 weeks to 10 months. This correlates with population-based reports that estimate median survivorship to range from 2 to 12 months after the diagnosis of bone metastasis.
Advances in materials and processing continue to reduce wear and osteolysis as a common form of intermediate-term and late failure after TKA, elevating the comparative importance of more unusual causes. Simultaneously, the near-universal annual reduction in cancer mortality rates is also relevant to the future incidence of periprosthetic metastases. By prolonging the life expectancy for these patients, it is plausible that orthopaedic surgeons may encounter greater numbers of patients with periprosthetic metastases from established and managed primary lesions in the near future.
Nonetheless, the clinical intricacy in detecting these findings increases in cases like the one presented here, without previous or current knowledge of a cancer diagnosis. Including metastasis and malignancy among differential diagnoses when evaluating patients with pain after arthroplasty offers a major opportunity to improve clinical outcomes. The earlier detection and treatment of periprosthetic neoplasms carry the potential to mitigate pain and improve extremity function throughout the remainder of the patient’s life. Identifying unknown primary lesions is a conjugate benefit of prompt evaluation because it will direct oncological treatment and prognosis according to the neoplasm.
Despite the benefits of early detection, the routine screening of every patient with pain after TKA for potential malignancy is unlikely to be cost-effective, and it should not replace evaluation for more common causes, including infection, loosening, or instability. However, it is imperative to actively consider patient risk factors for malignancies in the breast, prostate, and lung that commonly metastasize to bone. Therefore, extensive smoking history, as seen in this case, cancer history, and genetic predisposition should raise concern for metastasis as a differential diagnosis in these patients. Particular interest should be taken in the characteristics of the pain that a patient is experiencing for red flags of metastatic disease, such as pain that is described as being dull, increasing in intensity, and worsening at night. Moreover, unrelenting pain that persists, despite ruling out common causes, should also elevate the index of suspicion and may warrant further workup through inflammatory markers, local and solid organ CT scans, PET scans, and bone biopsy, because these form part of the baseline investigation into metastatic bone disease.
This case report highlights periprosthetic metastasis as a rare cause of pain in the context of a TKA. As the causes of failure evolve, wear-related osteolysis becomes less common, and life expectancy among patients with cancer continues to grow, practitioners should consider metastasis among their differential diagnoses when treating unremitting pain after TKA, particularly in the setting of aseptic loosening, focal lysis, or predisposing risk factors.
Reference: Baez C, Nusbickel AJ, Knapik JA, Deen JT. Periprosthetic metastatic lung carcinoma about a total knee arthroplasty: a case report. JBJS Case Connector. 2022 Oct-Dec;12(4):e22.00350.
What is the diagnosis?
Adverse local tissue reaction with foreign-body giant cells and debris
Metastatic squamous carcinoma consistent with lung origin
Epithelioid hemangioendothelioma
Granulomatous inflammation
Sarcoma associated with Paget disease




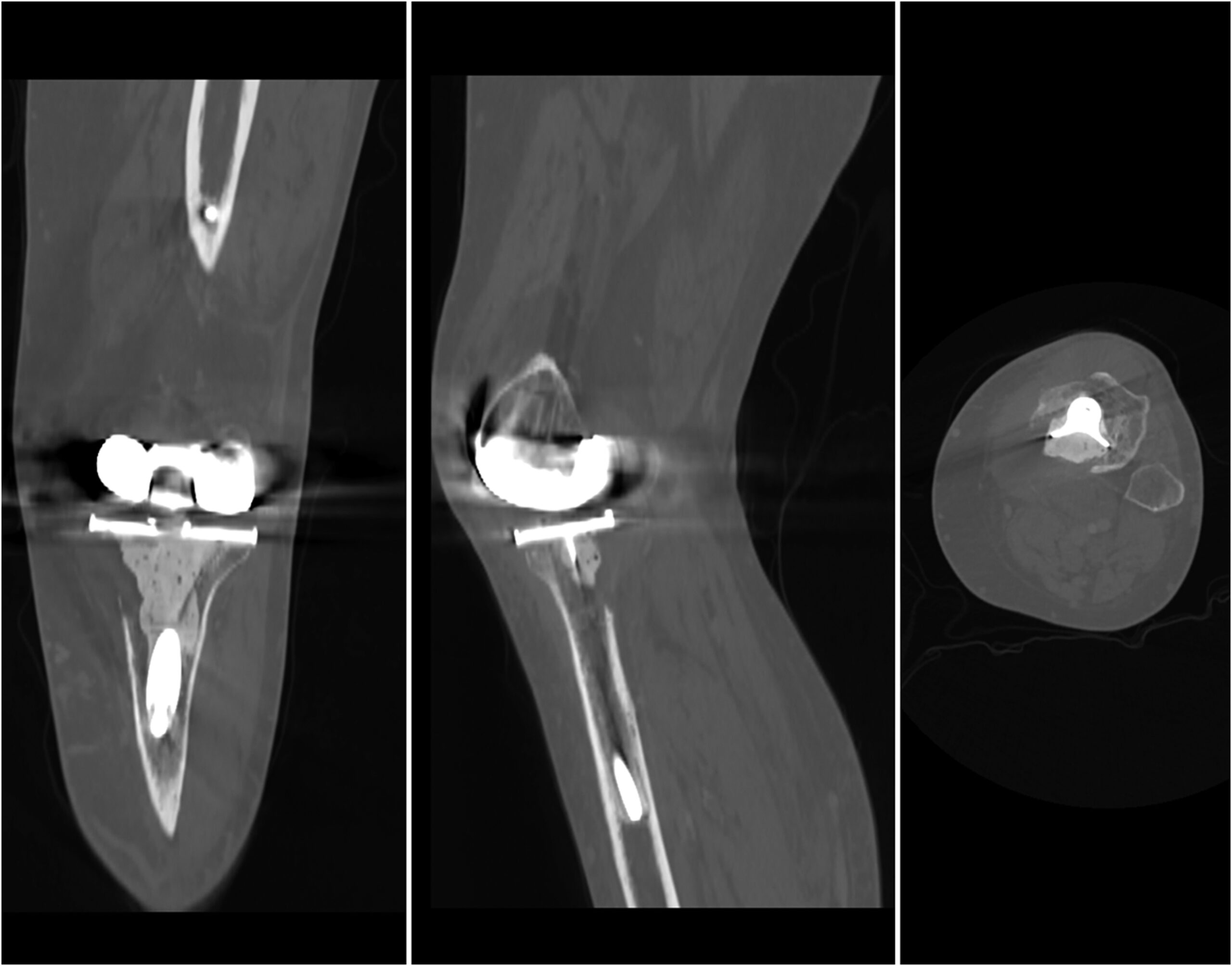
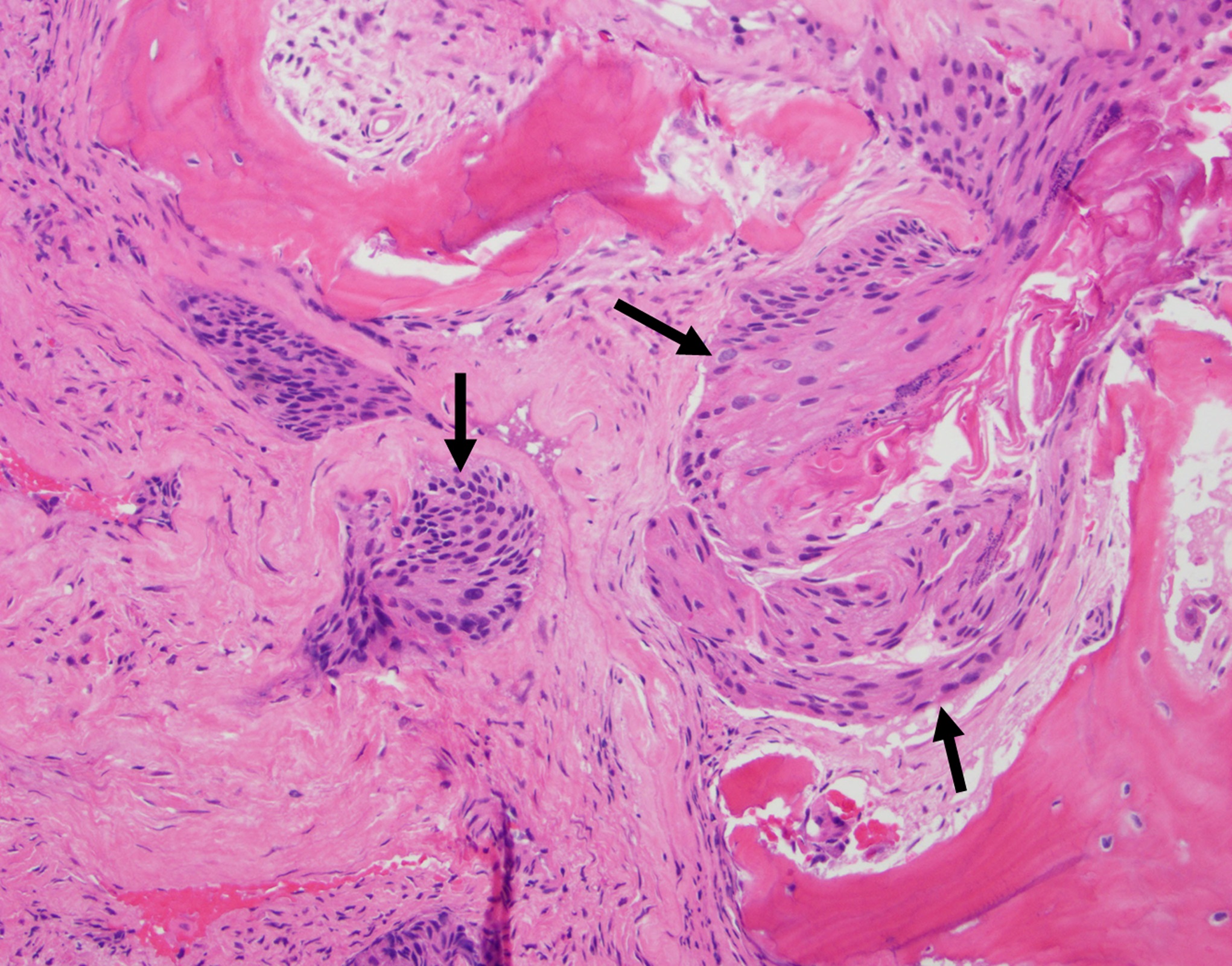
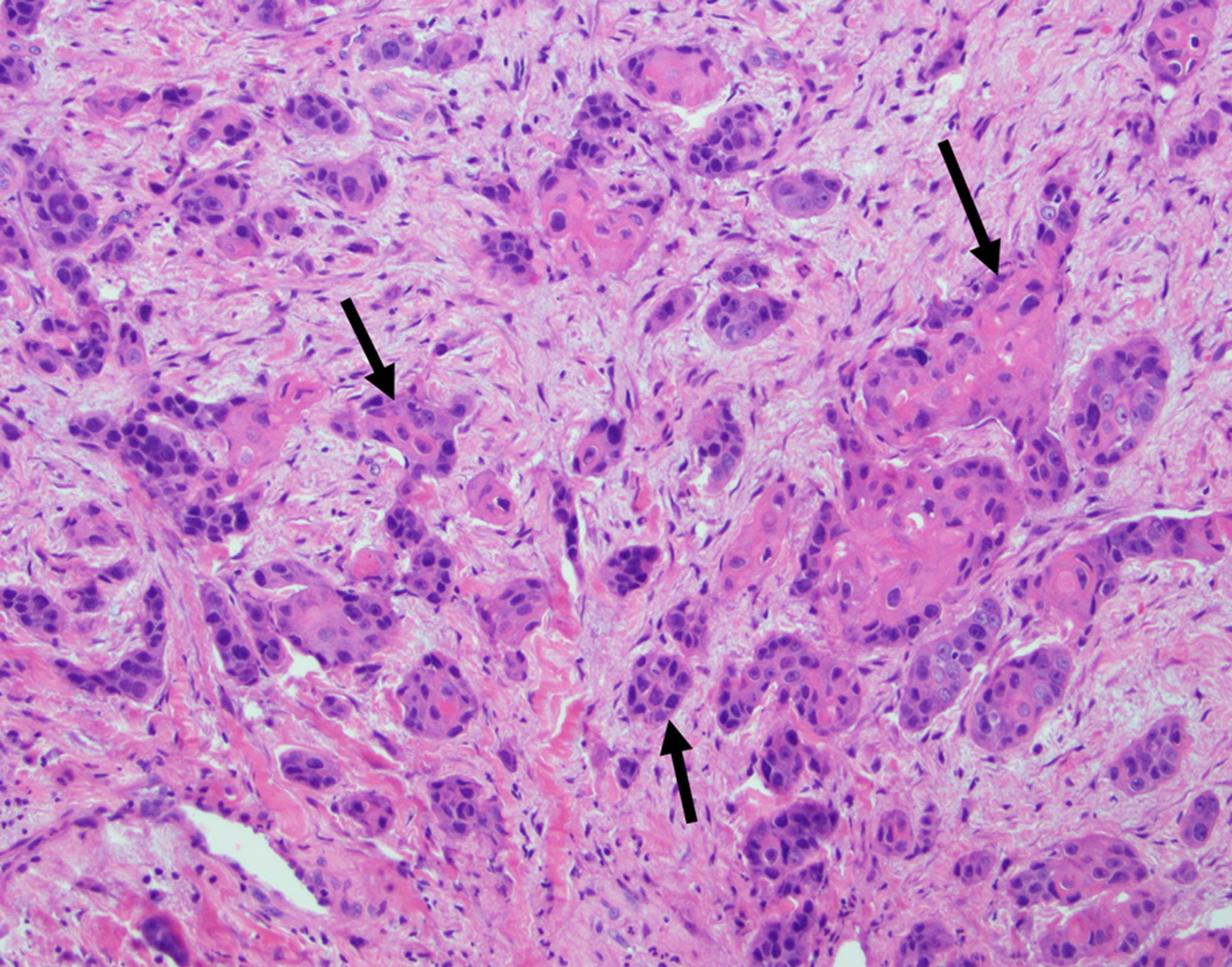
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3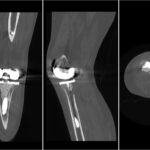 Fig. 4
Fig. 4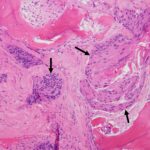 Fig. 5
Fig. 5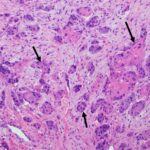 Fig. 6
Fig. 6 Fig. 7
Fig. 7