A 70-Year-Old Man with Shoulder and Elbow Pain
September 1, 2021
A 70-year-old man with no history of trauma visited our hospital because he was experiencing shoulder and elbow pain. He had been treated for multiple sclerosis with pulse steroid therapy using 1,000 mg of methylprednisolone sodium succinate. At the time of the initial visit, his body temperature was 37.4°C and tenderness and local heat were positive around the lateral side of the elbow. The shoulder forward elevation was restricted to 20° due to pain. The elbow range of motion was −10° for extension and 90° for flexion.
Blood tests showed the C-reactive protein (CRP) concentration to be 5.28 mg/dL (reference range, 0 to 0.14 mg/dL), and the radiographs showed osteolysis in the proximal part of the humerus and the lateral epicondyle (Fig. 1). Fat-suppression techniques in magnetic resonance imaging (MRI) scans revealed diffuse high-signal change in the medullary cavity in both the proximal and the distal epiphyses of the humerus (Fig. 2). The serum beta-d-glucan test was negative.
To obtain tissue for diagnosis, surgical debridement of the elbow was performed as ambulatory surgery. A 3-cm skin incision was made on the lateral epicondyle, and serous yellow fluid was found under the subcutaneous tissue. Two samples of the tissue were obtained from the medullary cavity of the humerus through the vulnerable portion of the lateral epicondyle. Afterward, the wound and the elbow joint were lavaged with saline. The wound healed well, and the sutures were removed 10 days after the surgical procedure. There were no complications observed. The pathologic examination revealed lymphocytes and neutrophils congregating in granulation tissue, along with multinucleated giant cells (Fig. 3). The fluid and the tissue sample culture test results were negative.
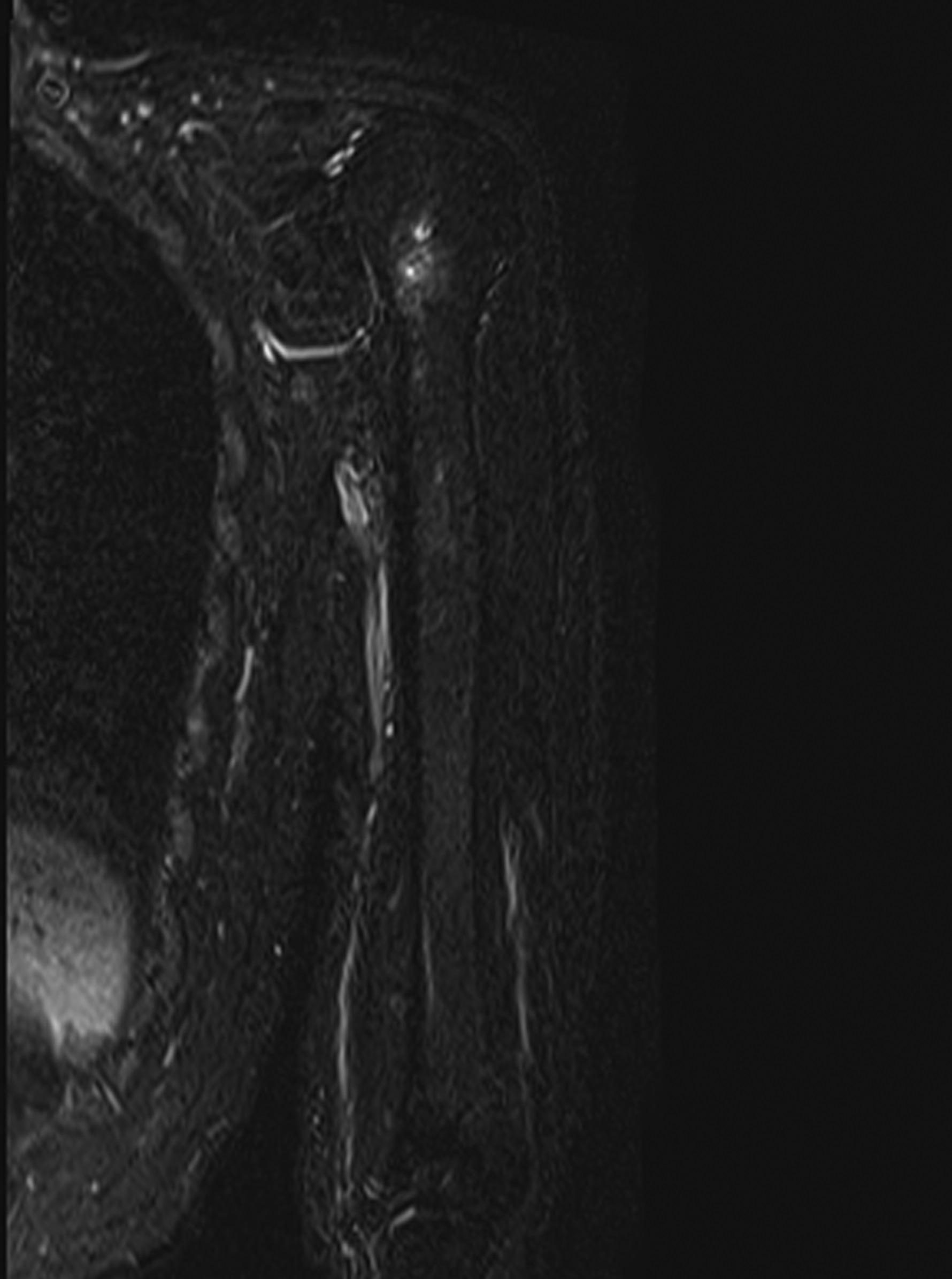
Based on a presumptive diagnosis of septic osteomyelitis, 3-g cefazolin sodium per day was administered intravenously. Subsequently, cephalexin at a dose of 1,500 mg was administered orally for 3 months until the CRP concentration decreased to 0.05 mg/dL. The elbow and shoulder pain subsided, but the shoulder pain recurred 10 days after the antibiotics treatment was completed. Although no signs of inflammation were found in the left elbow, redness, swelling, and tenderness were observed in the left shoulder. Thereafter, the CRP concentration increased to 1.12 mg/dL. Ultrasonography of the shoulder joint depicted discontinuity of the cortical bone of the humeral head (Fig. 4). Furthermore, MRI revealed multiple diffused lesions in the entire humerus (Fig. 5). The cortical bone of the humeral head had a partial defect.
The patient underwent open shoulder debridement, and a 7-cm deltoid-splitting approach was used. Granulation tissue was noted in the subacromial space. After removal of the granulation tissue with electrocautery, the cortical defect (5 mm in diameter) was observed in the humeral head. The granulation tissue and necrotic bone and marrow were curetted. The wound and the shoulder joint were lavaged with saline. The wound healed well, and the skin staples were removed 8 days after the surgical procedure. No complications were observed.
Multinucleated giant cells were observed on microscopic examination of the hematoxylin eosin-stained bone marrow slides in all the samples obtained from the surgical site (Fig. 6). Further pathological examinations were performed with Grocott, periodic acid-Schiff, and Ziehl-Neelsen staining (Fig. 7).
A Cryptococcus neoformans antigen with an antibody titer of 64 was detected in the blood test, and pulmonary nodular lesions were detected on the chest computed tomography (CT) scan (Fig. 8). These features, as well as the interpretation of the biopsy, led to the diagnosis of cryptococcal osteomyelitis of the humerus.
The patient later revealed that pigeons were dwelling on his balcony, and he had to clean pigeon stools daily. Fluconazole at a dose of 400 mg/day was administered to the patient for 5 months before it was reduced to 200 mg/day for the following 17 months. The patient was discharged 24 days after the surgical procedure. The shoulder pain subsided 1 year after the surgical procedure. Neither recurrence of the pain nor increase in the CRP concentration were observed at the latest follow-up.
The patient felt no pain in the shoulder and elbow joint at 30 months postoperatively. The shoulder forward elevation improved to 155°. The elbow range of motion was 0° for extension and 140° for flexion. The high-signal areas almost disappeared on the MRI scan (Fig. 9). The antibody titers of C. neoformans antigen gradually decreased and finally turned negative at 30 months postoperatively.
Proceed to Discussion >>Reference: Onishi O, Kida Y, Kiba T, Kabuto Y, Minami M, Nishimura A, Konishi E, Takahashi K. Cryptococcal osteomyelitis of the entire humerus: a case report. JBJS Case Connect. 2020 Oct-Dec;10(4):e20.00279.
Cryptococcus is an encapsulated fungus existing in high concentrations in the stools of birds. Once inhaled as aerosol droplets, Cryptococcus causes opportunistic infections in immunocompromised people. The lungs and the central nerve system become infected most commonly, and isolated osteomyelitis in an extrapulmonary lesion is rare.
In this case, the patient was immunocompromised because of steroid treatment for multiple sclerosis. Pigeons frequently came to the balcony of his house; subsequently, the patient was highly exposed to aerial fungal pathogen from pigeon excreta, and, finally, the pathogen affected the lung by inhalation, whereas most people encountering the cryptococcal pathogen are asymptomatic, and cryptococcal lung masses may form in immunocompromised patients. In our patient, Cryptococcus affected the humeral bone hematogenously, penetrating the cortical bone of the epicondyle and humeral head, which is similar to the pathogenesis described in a previous study. In the case presented herein, we did not initially diagnose the condition as cryptococcal osteomyelitis. Instead, we assumed the diagnosis to be bacterial osteomyelitis of the humerus because of the high CRP level, the signal change in the bone marrow of humerus on the MRI, and the negative result of the serum beta-d-glucan test. Therefore, we did not send the sample for the Grocott staining at the first surgical biopsy from the elbow. However, antibiotic administration after debridement of the elbow resulted in incomplete healing.
No pathogens were found in the initial pathological samples from the shoulder, although we realized that multinucleated giant cell formation suggested the possibility of a fungal infection. Therefore, Grocott, periodic acid-Schiff, and Ziehl-Neelsen stainings were added to detect the pathogen other than bacteria for the samples from the shoulder. Grocott staining revealed the presence of a fungal infection, and the cryptococcal antigen test result was positive. Debridement and antifungal agent administration improved the patient’s condition.
Bacteria, such as Staphylococcus aureus, are commonly the cause of osteomyelitis. In our case, the bacterial culture was negative, but because false-negative cultures are not rare, we continued the administration of cephem antibiotics. It was difficult to suspect a fungal infection because the patient’s symptoms and CRP level improved and cultures were negative. At first, we only investigated a beta-d-glucan test to rule out a fungal infection. Although a beta-d-glucan test will be positive for fungal infections such as candidiasis and aspergillosis, it should be negative for cryptococcosis. Hence, this was an important pitfall. Furthermore, the cryptococcal yeast is very difficult to visualize using hematoxylin-eosin staining alone, although multinucleated giant cells made us suspect a fungal infection.
To our knowledge, cryptococcal osteomyelitis of the humerus has been reported by only 6 authors (7 patients in total) since 1988. All 7 reported cases had focal lesions (distal, medial, or proximal) in the humerus, whereas diffuse lesions of the entire humerus have not been reported. In this case, the entire humerus was affected by Cryptococcus; hence, a surgical procedure of the elbow and the shoulder was necessary for infection control.
Orthopaedic surgeons should consider not only bacteria but also Cryptococcus as the pathogen of osteomyelitis around the elbow and shoulder when the beta-d-glucan test is negative.
Reference: Onishi O, Kida Y, Kiba T, Kabuto Y, Minami M, Nishimura A, Konishi E, Takahashi K. Cryptococcal osteomyelitis of the entire humerus: a case report. JBJS Case Connect. 2020 Oct-Dec;10(4):e20.00279.
What is the diagnosis?
Cryptococcal osteomyelitis
Langerhans cell histiocytosis
Collagenous spherulosis
Valley fever (coccidioidomycosis)
Candida osteomyelitis

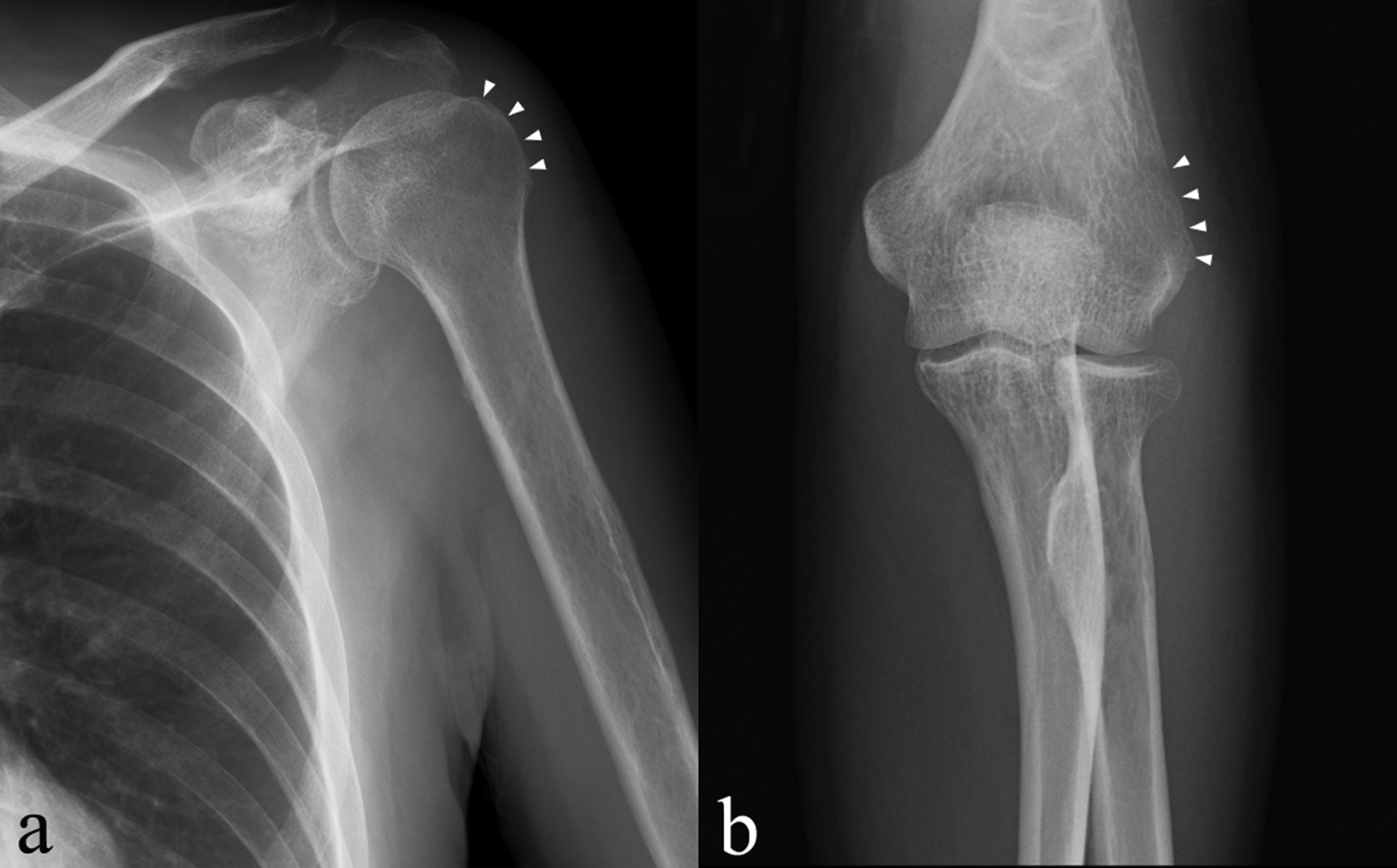
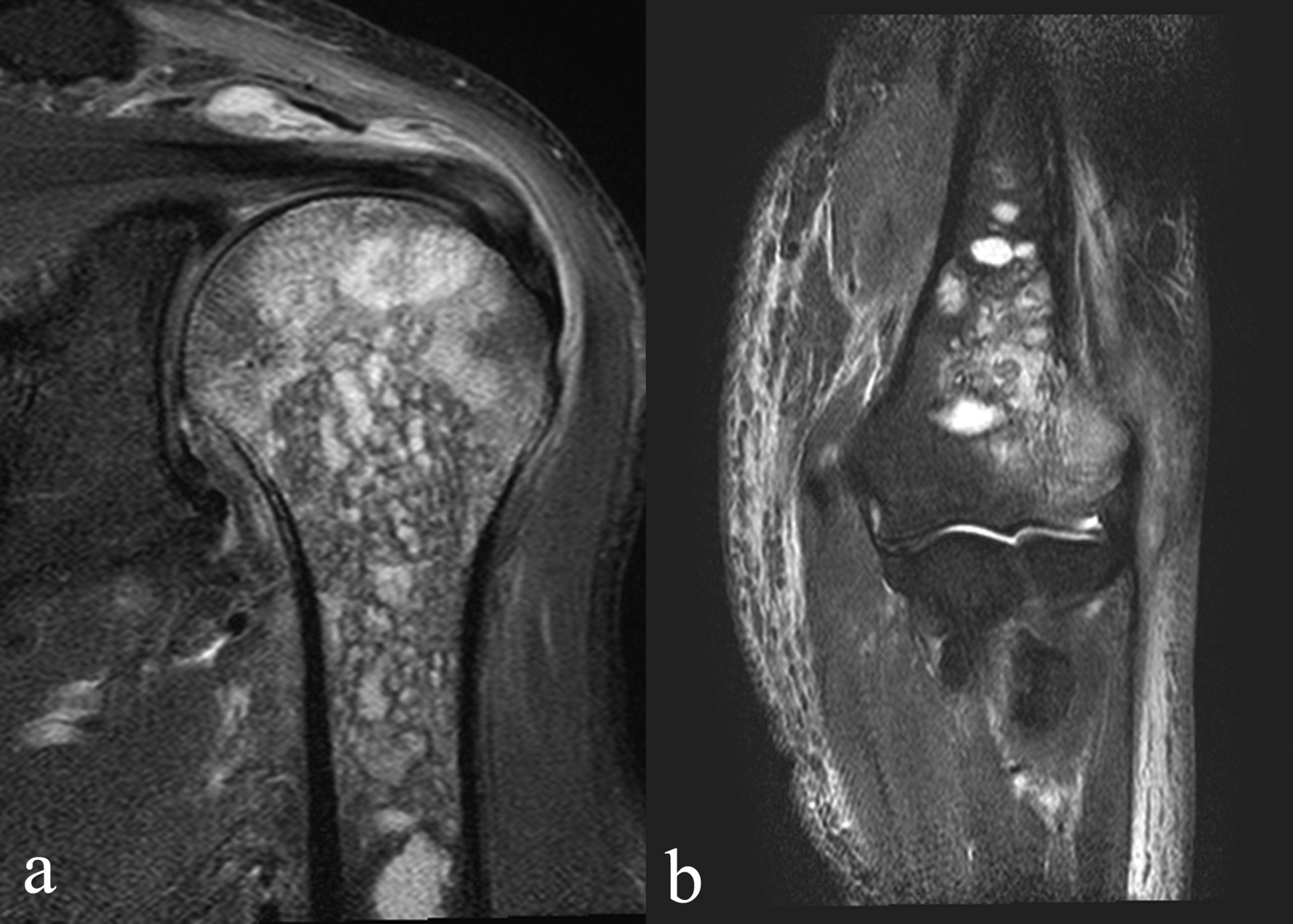
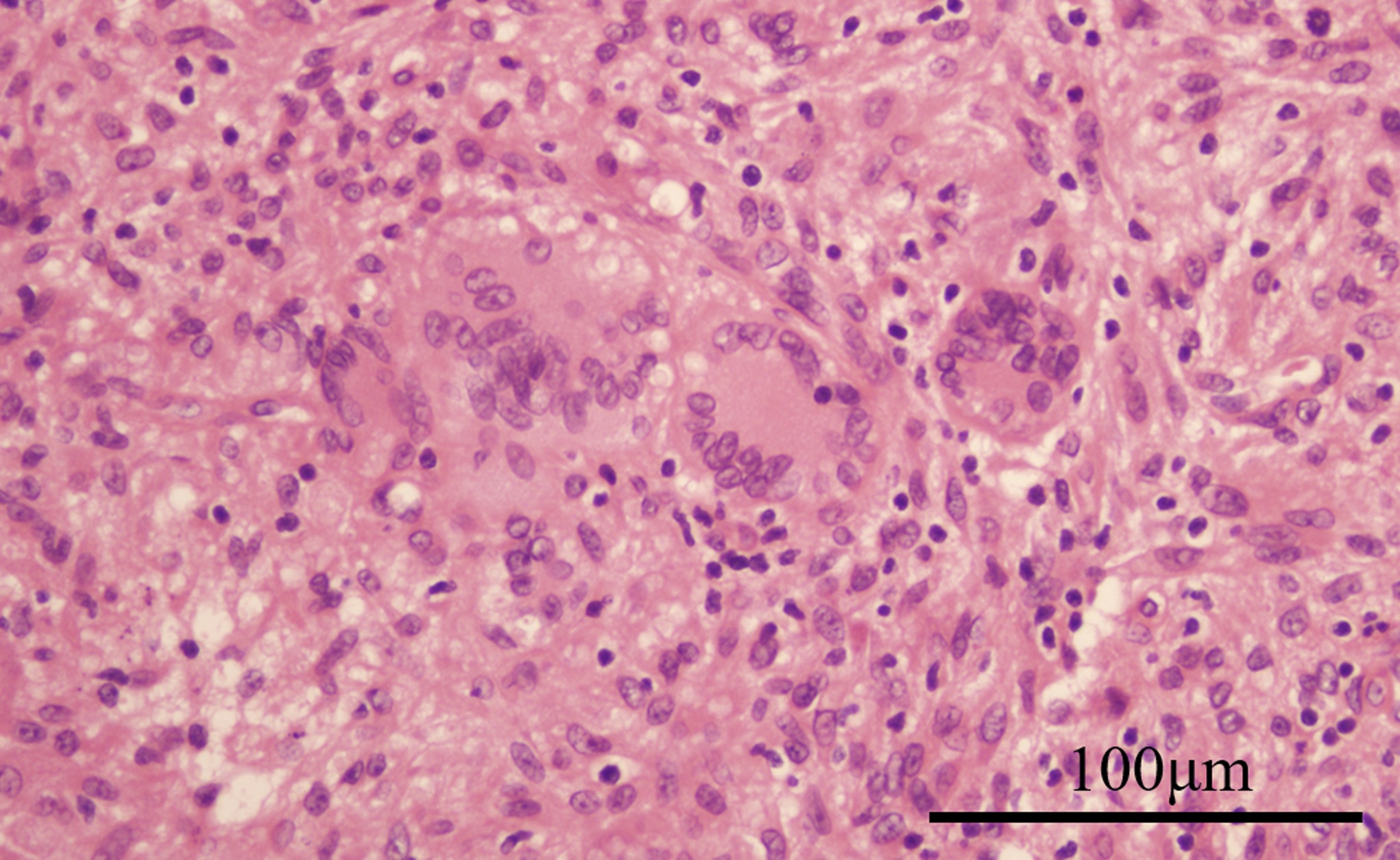
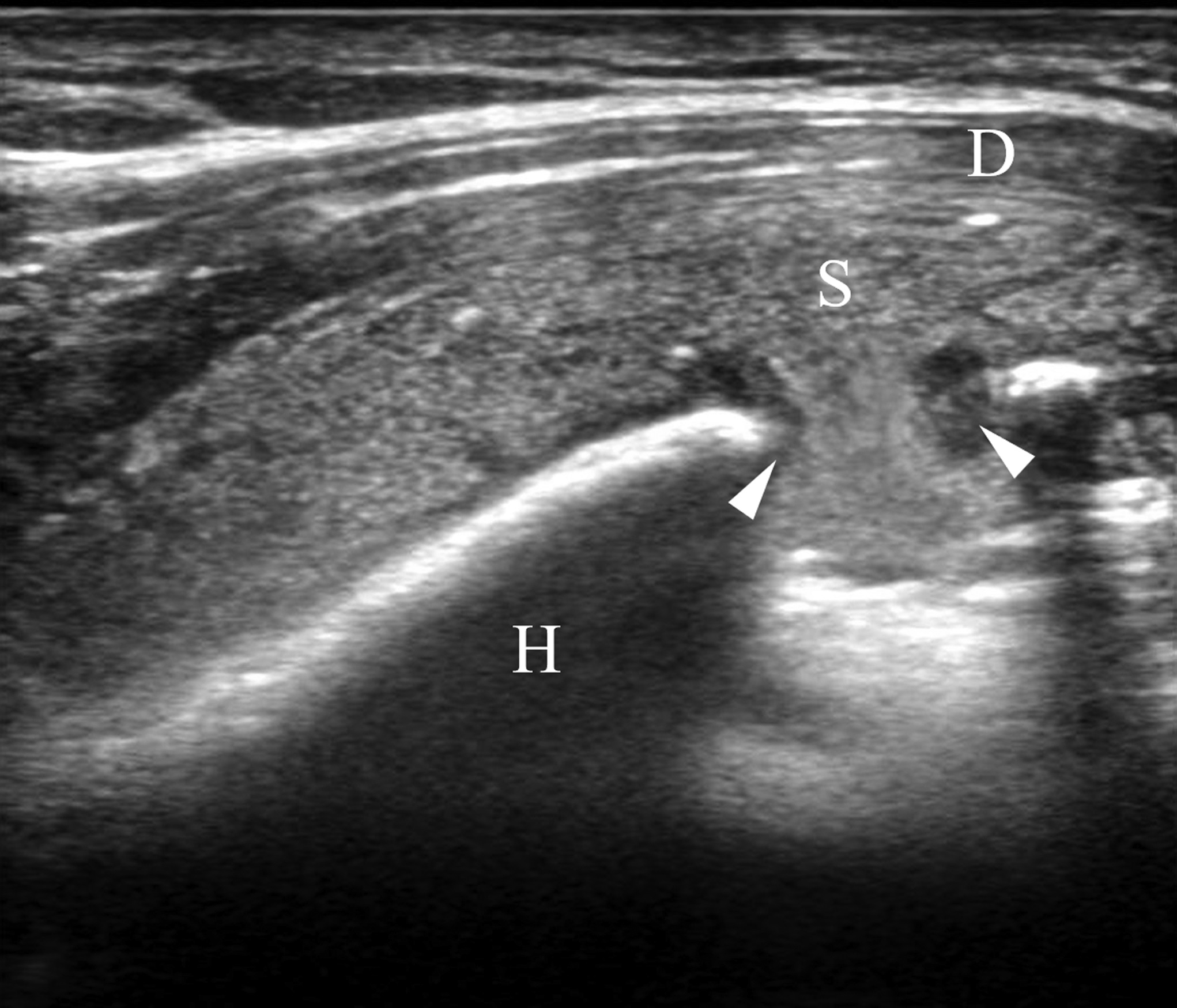


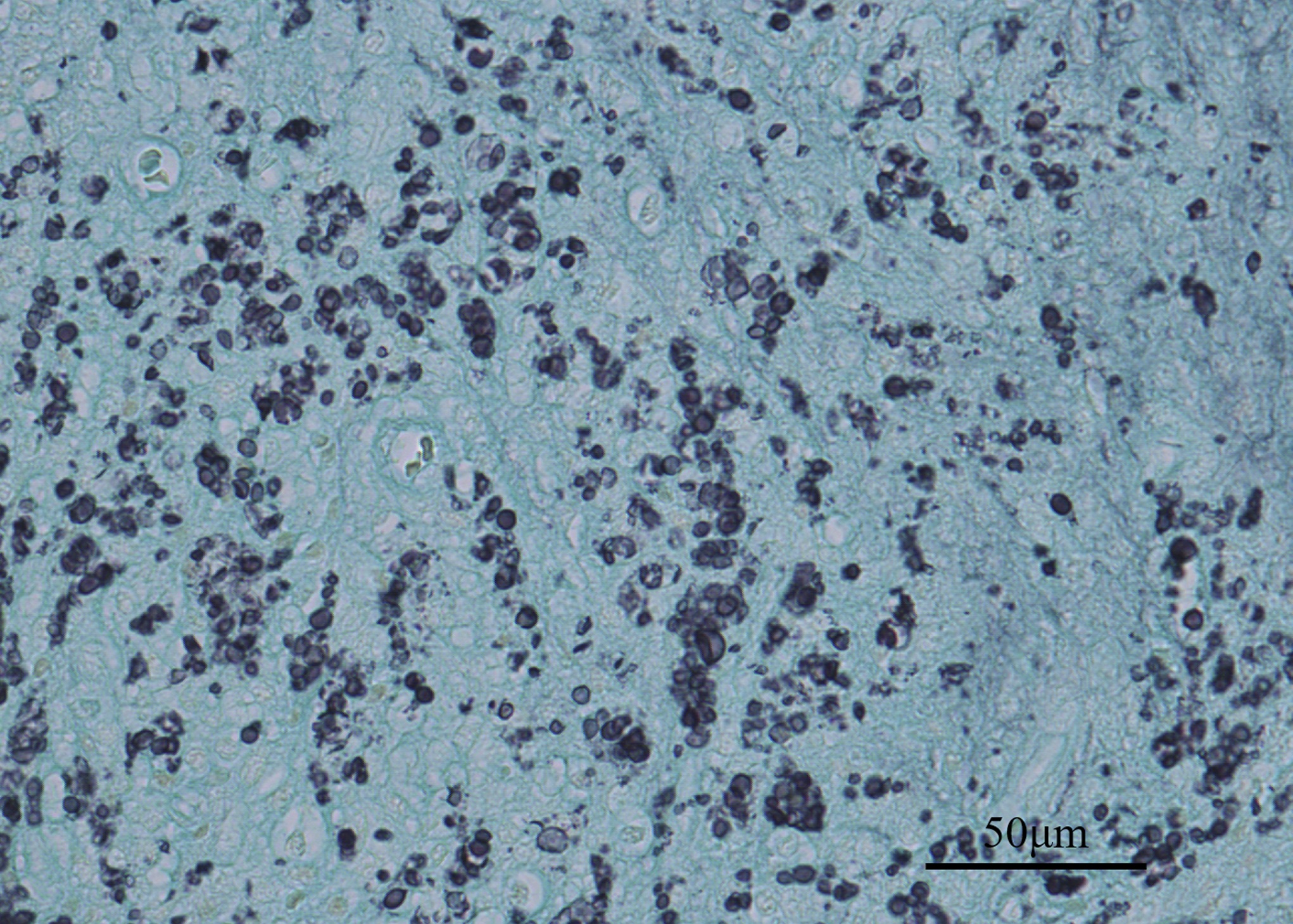
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5
Fig. 5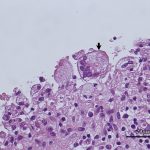 Fig. 6
Fig. 6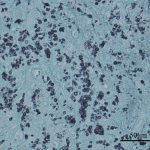 Fig. 7
Fig. 7 Fig. 8
Fig. 8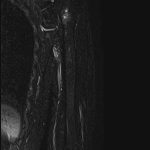 Fig. 9
Fig. 9