A 77-year-old man was referred for right groin and buttock pain that he had experienced for 12 months. The pain was associated with reduced range of motion and difficulty weight-bearing on the involved side. The patient had undergone bilateral total hip arthroplasties (THAs) 10 years previously without any problems (Fig. 1). The THAs were undertaken using the PINNACLE Cup (DePuy Synthes), Marathon highly cross-linked polyethylene liner (DePuy Synthes), titanium alloy Summit tapered stem (DePuy Synthes), and cobalt-chrome ARTICUL/EZE 12/14 taper femoral head (DePuy Synthes). The patient had no other notable medical history.
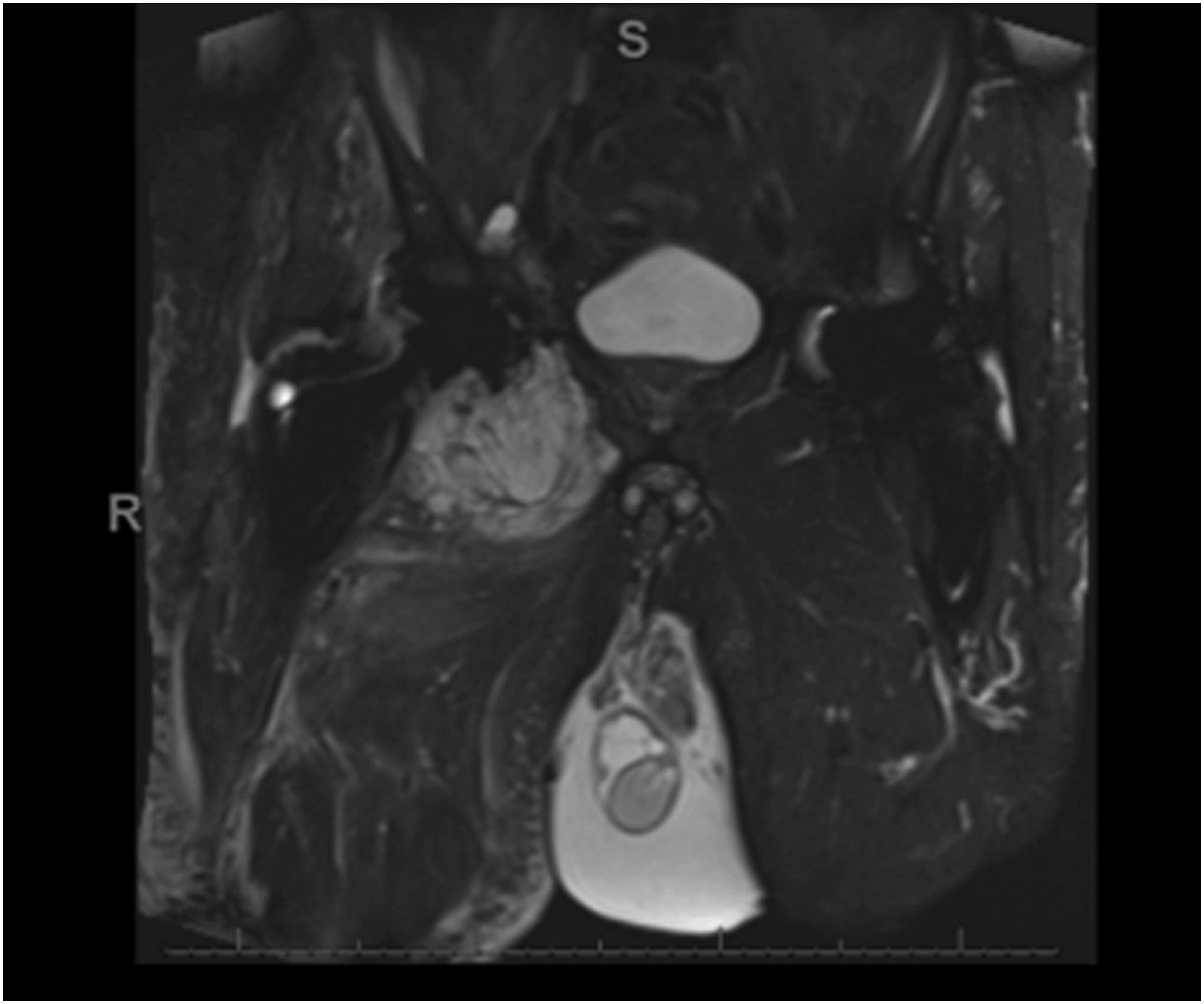
Serum metal ion levels showed cobalt 4.9 nmol/L (reference range, 2.4 to 8.3 nmol/L) with chromium 6.0 nmol/L (reference range, 2.5 to 6.0 nmol/L), and metal artifact reduction sequence magnetic resonance imaging (MARS MRI) demonstrated a 6.5 × 8.7 × 4.6-cm right hip periarticular hyperintense lesion with a thickened pseudocapsule and surrounding fluid with metallic debris. A soft-tissue core needle biopsy of the lesion revealed extensive inflammatory cells.
The patient underwent revision THA with exchange of modular components and debulking. Biopsies obtained for frozen section were not representative, but separate biopsies were obtained for permanent sections only. The histology of the subsequently excised tissue is shown in Figures 2 and 3.
During the same admission, an orthopaedic oncologist attempted a surgical resection of the residual neoplasm with wide resection margins, although true-negative margins were impossible because of the surgical contamination at the time of the revision hip replacement. The excised tissue was interpreted as a low-grade chondrosarcoma, possibly arising from synovial chondromatosis.
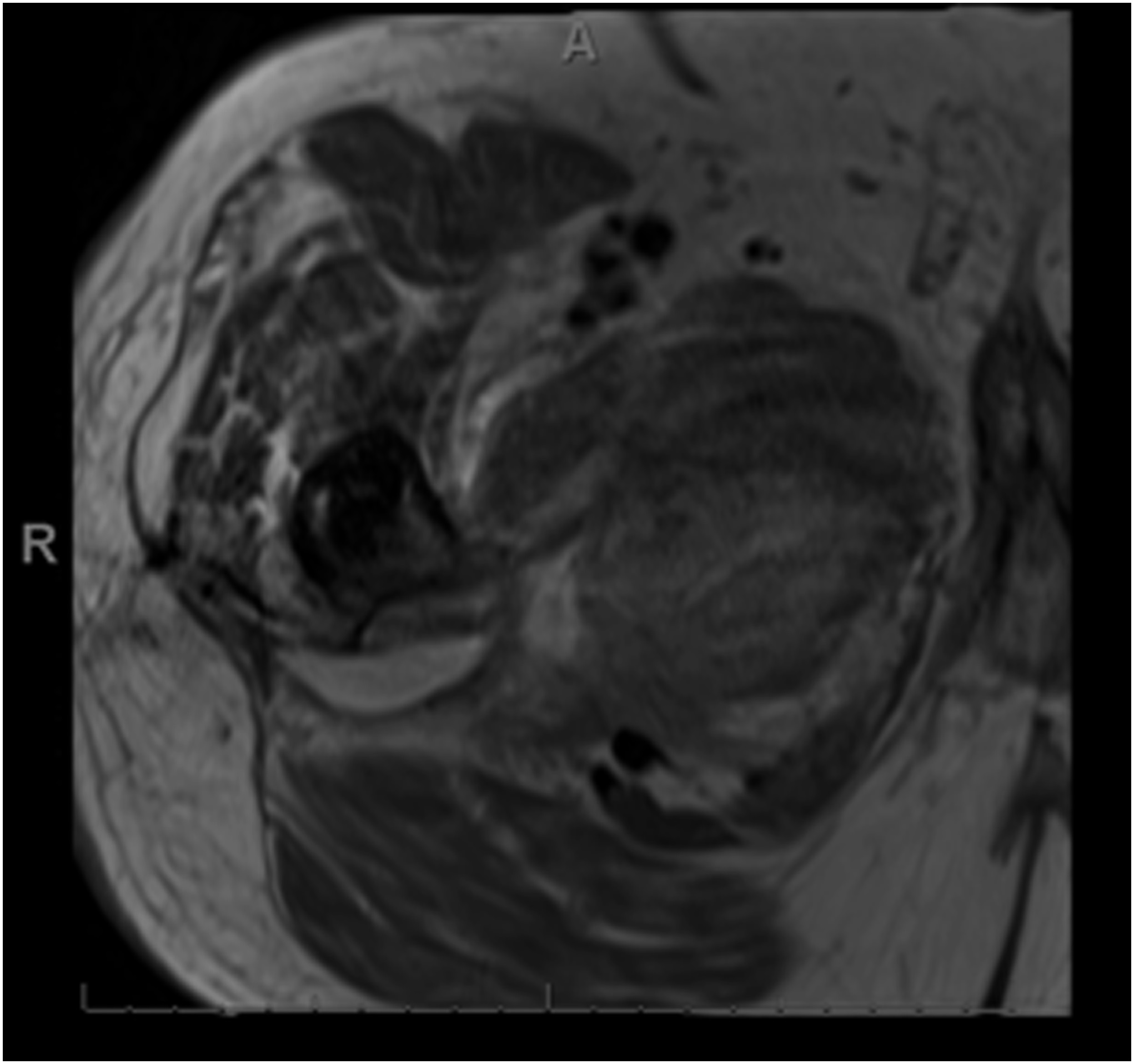
Nine months later, the patient presented with increasing right groin pain and reduced range of motion in the right hip. A repeat MARS MRI scan showed an extensive aggressive recurrence of the tumor around the external surface of the pelvis along with involvement of the major neurovascular structures (Figs. 4 and 5).
The disease was behaving in a much more clinically aggressive manner than the histologic grade would have suggested. The patient underwent chest, abdominal, and pelvic computed tomographic (CT) scans, which showed no evidence of metastases or systemic disease dissemination. The sarcoma multidisciplinary team reviewed the case and reached a consensus for hemipelvectomy with no role for chemotherapy or radiotherapy. The patient underwent right external hemipelvectomy with wide resection margins (Fig. 6). He made an excellent recovery after the procedures. At 16 months after the surgical procedure, the patient remained cancer-free, mobilized with 2 crutches, and remained independent with all activities of daily living. At the latest follow-up, he was undergoing surveillance with CT scans of the chest, abdomen, and pelvis biannually, as per the British Columbia Cancer Agency protocol.
Proceed to Discussion >>Reference: Kayani B, Clarkson P, Ng T, Masri BA. A sarcoma masquerading as a pseudotumor after total hip arthroplasty: a case report. JBJS Case Connect. 2023 Dec 14;13(4).e23.00275.
This report provides important clinical lessons in the management of soft-tissue lesions around prosthetic joints. The course of this rare case highlights the importance of considering sarcomas in the differential diagnosis of soft-tissue lesions around hip articulations, especially when a definitive histological diagnosis on biopsy has not been established, and when the metal ion levels are <1 part per billion, which is the threshold recommended for the suspicion of pseudotumor.
Soft-tissue sarcomas comprise a group of >70 distinct histological entities of malignant neoplasms that are grouped together because of their common mesenchymal origin. These lesions are rare and account for <1% of all malignancies, with approximately 13,000 new cases per year in the United States. Although soft-tissue sarcomas may be present in proximity to prosthetic joints, no causative relationship has been established to help to explain the presence of these lesions in our patient who had undergone a previous metal-on-polyethylene THA. In this report, the extraskeletal chondrosarcoma seems to have occurred sporadically without any clear, identifiable etiology or history of exposure to known risk factors including radiation treatment, viral infections, immunosuppression, herbicide exposure, or genetic syndromes.
Synovial chondromatosis is characterized by the proliferation of cartilage within the synovial membrane due to subsynovial connective tissue metaplasia. The diagnosis of synovial chondromatosis should be considered in any patient presenting with an intra-articular soft-tissue mass, particularly if there are radiographic features of superficial bony erosion and mineralization. The transformation of synovial chondromatosis into secondary chondrosarcoma is a rare event that occurs at a mean time of 11 years after diagnosis and most commonly affects the knee joint (47.7%), followed by the hip joint (34.3%) and the ankle joint (5.9%). Importantly, distinguishing between synovial chondromatosis and secondary chondrosarcoma may be challenging because the histological features may overlap, particularly with inadequate tissue sampling in patients with multifocal secondary chondrosarcoma. Accurate diagnosis, therefore, requires a comprehensive evaluation of clinical, radiological, and histological findings.
It has been previously shown that deep-seated intra-abdominal or pelvic sarcomas often present later in the disease process with larger and more advanced tumors compared with those in the extremities. The deep-seated tumors may compress neurovascular structures and intrapelvic organs leading to a wide spectrum of neurological, vascular, gastrointestinal, and genitourinary symptoms. In this case report, the intrapelvic tumor was able to reach considerable size before becoming symptomatic, which may have contributed to the poor outcome. Tumor invasion into the surrounding soft tissues may have led to microextensions into the pseudocapsule, with further seeding of the tumor during revision THA for the suspected pseudotumor. These may have increased the risk of disease recurrence that required subsequent treatment with hemipelvectomy.
The judicious use of advanced localized imaging with MARS MRI and tissue biopsy with pathological examination is important for establishing the correct diagnosis and planning treatment. In this report, the chondrosarcoma displayed radiological features on MARS MRI that are also commonly present with pseudotumors, including a poorly defined solid mass, thickened pseudocapsule, synovial thickening, surrounding edema, and dispersed metallic debris. Furthermore, the metal ion levels were not elevated, and the initial histology was negative for sarcoma. The normal metal ion levels should have been a hint that a pseudotumor was not a likely diagnosis. Chondrosarcomas are notoriously difficult to diagnose on core needle biopsy, and, in the presence of normal metal ion levels and a negative core needle biopsy, an open biopsy should be considered to rule out a sarcoma.
In summary, we have reported the case of a malignant sarcoma clinically and radiologically appearing as a benign pseudotumor around a prosthetic hip articulation. The patient had inconclusive initial biopsy findings with normal serum metal ion levels. The report highlights the importance of considering sarcomas in the differential diagnosis of masses around hip implants, especially when a definitive histological diagnosis has not been established and metal ion levels are not elevated.
Reference: Kayani B, Clarkson P, Ng T, Masri BA. A sarcoma masquerading as a pseudotumor after total hip arthroplasty: a case report. JBJS Case Connect. 2023 Dec 14;13(4).e23.00275.
What is the diagnosis?
Adverse local tissue reaction to debris
Periprosthetic pseudotumor
Chondrosarcoma in cap of osteochondroma
Low-grade chondrosarcoma
Chondroblastic osteosarcoma


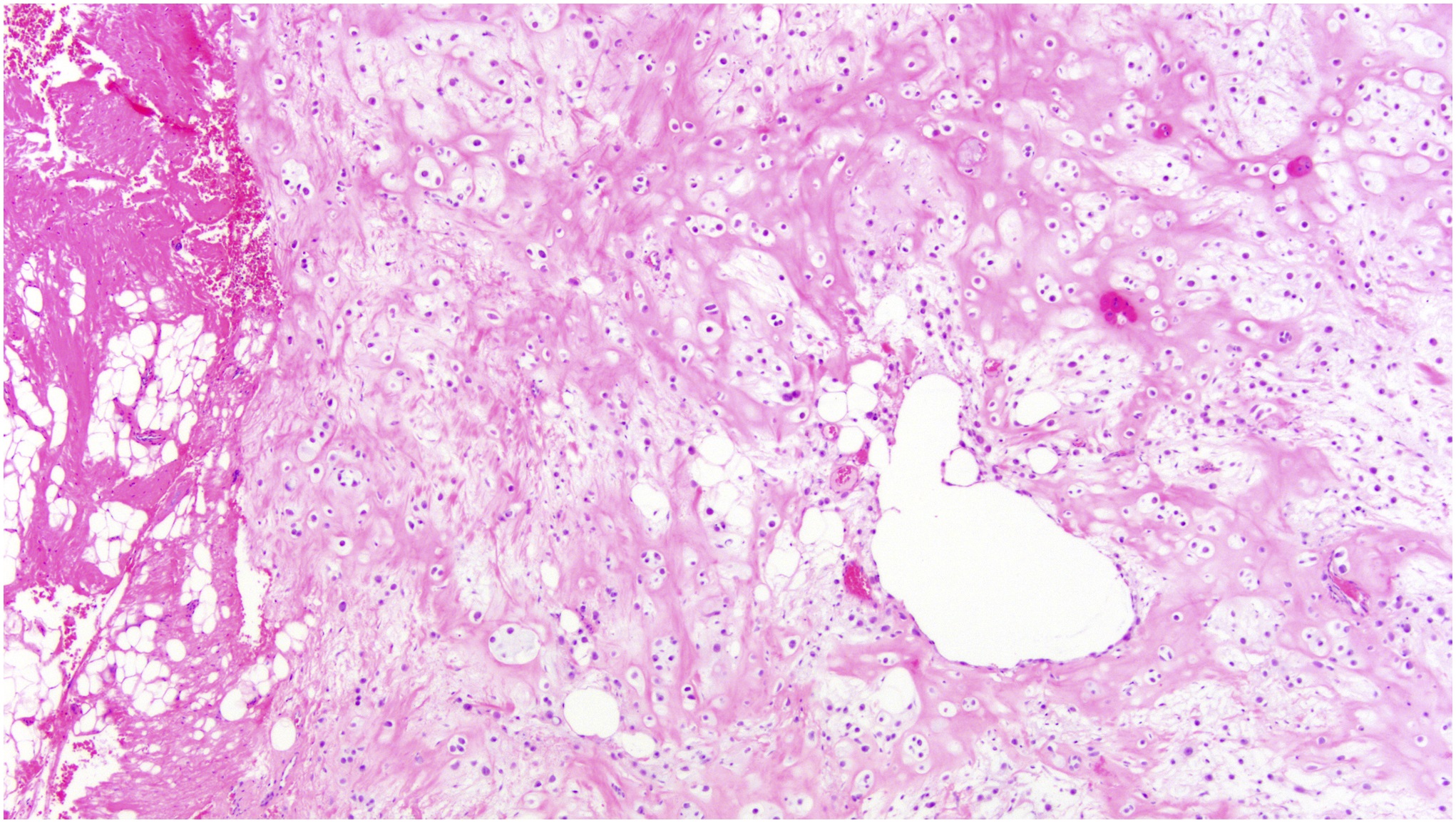
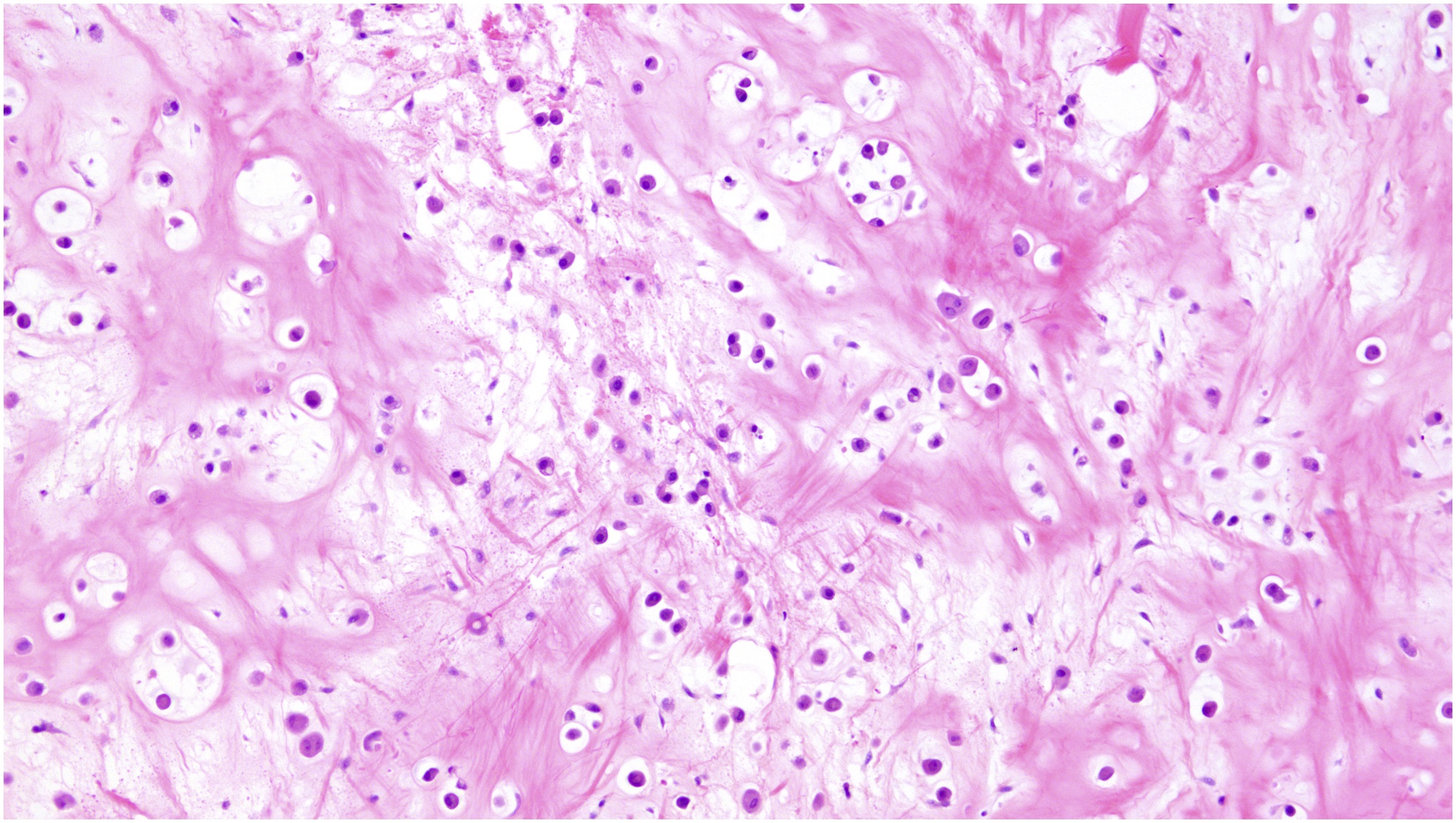
 Fig. 1
Fig. 1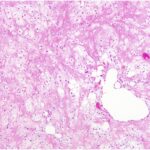 Fig. 2
Fig. 2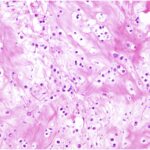 Fig. 3
Fig. 3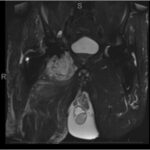 Fig. 4
Fig. 4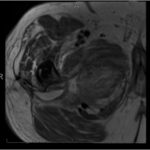 Fig. 5
Fig. 5 Fig. 6
Fig. 6