A Fifteen-Year-Old Girl with Abnormal Appearance of the Patella
August 7, 2013
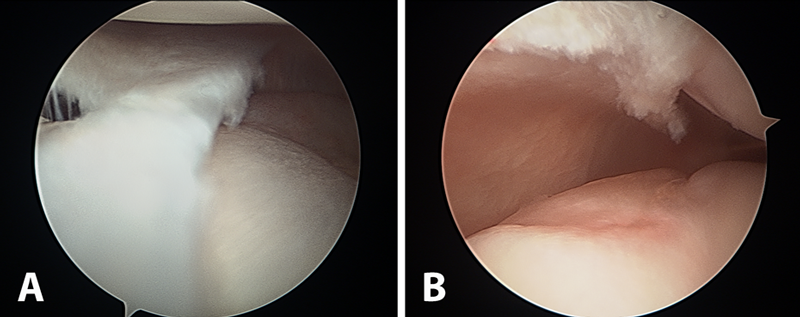
A fifteen-year-old girl presented with a two-year history of worsening bilateral anterior knee pain and a recurrent painful catching sensation without any known history of trauma or patellar dislocation. She had previously been evaluated orthopaedically and had been diagnosed with recurrent knee sprains. The pain had not improved with activity modification, a period of protected weight-bearing with crutches, or extended use of nonsteroidal anti-inflammatory medications. The clinical examination was notable for bilateral patellar apprehension and a clunking sensation of the patella around 30° of active flexion, with a normal range of motion of 0° to 140°. The pain and clunking were improved when the patella was stabilized inferiorly through active range of motion. The remaining knee examination was unremarkable. No evidence of joint contracture, clubfoot deformity, or brachydactyly was noted. Diagnostic imaging studies consisted of magnetic resonance imaging (MRI) (Fig. 1) in addition to computed tomography (CT) (Fig. 2) and bilateral knee radiographs. These studies demonstrated two distinct anterior and posterior ossified patellar layers on both knees. The tibial tubercle-trochlear groove distance on the axial image overlay was 5.6 mm, indicating grossly normal osseous alignment. MRI showed that the extensor mechanism and retinacular complex insertions were limited to the anterior fragment only (Fig. 1).
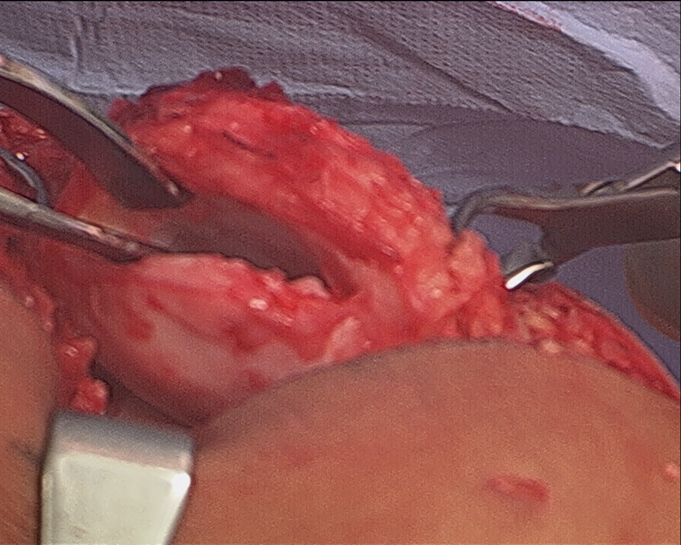
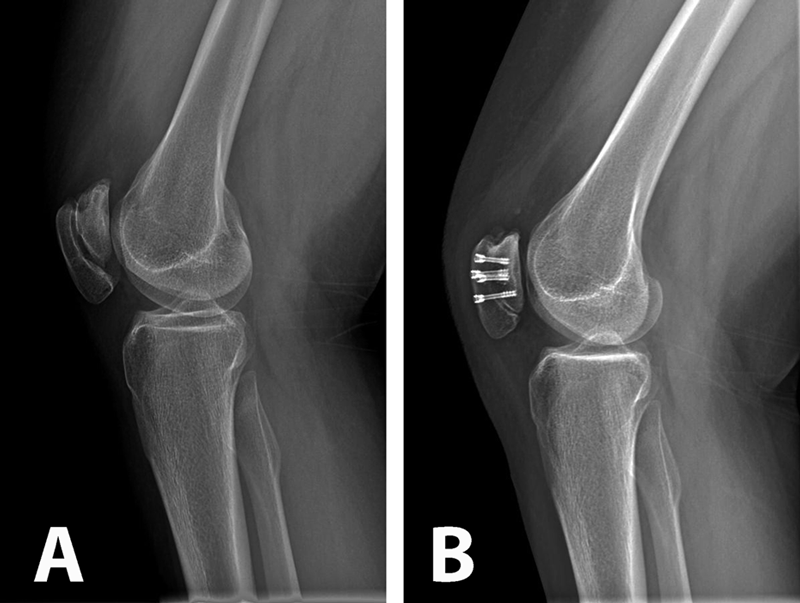
The patient was referred to a genetic counselor for additional evaluation. Molecular testing revealed a homozygous diastrophic dysplasia sulfate transporter (DTDST) gene mutation and confirmed a diagnosis of autosomal recessive multiple epiphyseal dysplasia (MED). The condition of double-layered patella (DLP) is strongly associated with MED. A radiographic survey revealed mild bilateral hip dysplasia but no additional skeletal abnormalities. The patient and her family elected to proceed with surgery on the right knee since the symptoms were more frequent and severe than in the left knee. In the operating room, the knee was initially manipulated under anesthesia to assess the degree of instability between the osseous patellar layers. The anterior and posterior parts moved independently starting at full extension to approximately 40° of flexion, at which point the posterior part clunked from a superior location and located inferiorly, directly posterior to the larger anterior piece, which was anchored by the patellar tendon. Tracking in the coronal plane appeared to be in appropriate alignment. Next, diagnostic arthroscopy was performed; it revealed a substantial medial plica with clefting of the medial femoral condyle (Fig. 3-A) as well as a grade-2 lesion of the midportion of the tibial plateau with loose bodies. The plica was debrided, a limited chondroplasty was performed, and the loose bodies were removed. The trochlea appeared mildly dysplastic with grossly normal cartilage (Fig. 3-B). Intra-articular visualization of the patella while the knee was manipulated from extension to flexion demonstrated sudden relocation of the posterior osseous layer with a palpable clunk at 40° of flexion. We then performed a medial parapatellar open approach to the knee. Once the retinaculum was reduced, the intervening soft tissue between the ossified patellar layers was grossly similar to synovial tissue and hyaline cartilage; this was confirmed on pathologic analysis. The cartilage interface was then debrided and burred down to cancellous bone on both the anterior and posterior surfaces between the two aspects of the patella (Fig. 4). Demineralized bone graft mixed with autologous platelet-rich plasma (GPS II Gravitational Platelet Separation System; Biomet, Warsaw, Indiana) was applied in the interface to assist with fusion. Finally, the osseous layers were fixed in compression with four headless screws (Darco-Wright Medical, Arlington, Tennessee) directed from anterior to posterior in a diamond-shaped configuration. Immediately following the procedure, the knee was manipulated through a full range of motion and revealed smooth patellar tracking. The patient was allowed to bear weight as tolerated postoperatively and progressively increased range of motion with a continuous passive motion machine. At the first postoperative visit, she had no mechanical symptoms; at the sixteen-month follow-up, the patient remained symptom-free and was quite happy with the outcome. The same procedure was later performed on the left knee, with similar resolution of symptoms; at the eight-month follow-up, the left knee remained symptom-free as well. The gait had normalized and she had begun participating in sports activities (Fig. 5).
Proceed to Discussion >>Reference: Nguyen MD, Everhart JS, May MM, Flanigan DC. Bilateral double-layered patella: MRI findings and fusion with multiple headless screws: a case report. JBJS Case Connector. 2013 May 22;3(2):e50.
There is very limited information on the evaluation and treatment of DLP. Our experience with MRI to evaluate the extensor tendon insertion site and use of soft-tissue debridement and osseous fusion with headless screws was favorable and provides additional insight into the successful treatment of patients with DLP with unstable osseous layers. This imaging modality provides useful information for preoperative planning, particularly for visualization of the patellofemoral articular cartilage and extensor tendon insertion sites. In our patient, the extensor tendon and the retinaculum and medial patellofemoral ligament insertions were limited to the anterior layer, necessitating fusion of both layers and repair of the medial retinacular complex to restore normal extensor function and medial stability to the posterior (articular) osseous layer. MRI also allows for evaluation of the status of the patellofemoral articular cartilage in addition to the alignment of the tibial tubercle relative to the trochlear groove. In our case, the cartilage surface was grossly normal and the patient had normal tibial tubercle-trochlear groove alignment. Therefore, we were able to determine preoperatively that lack of stabilizing soft-tissue attachments to the posterior osseous layer rather than osseous malalignment was the cause of instability, and that a tibial tubercle osteotomy would be unlikely to improve the treatment outcome.
Reference: Nguyen MD, Everhart JS, May MM, Flanigan DC. Bilateral double-layered patella: MRI findings and fusion with multiple headless screws: a case report. JBJS Case Connector. 2013 May 22;3(2):e50.
Nonunion of a patellar fracture
Acute patellar fracture
Aberrant quadriceps tendon insertion
Congenital double-layered patella
Morquio disease

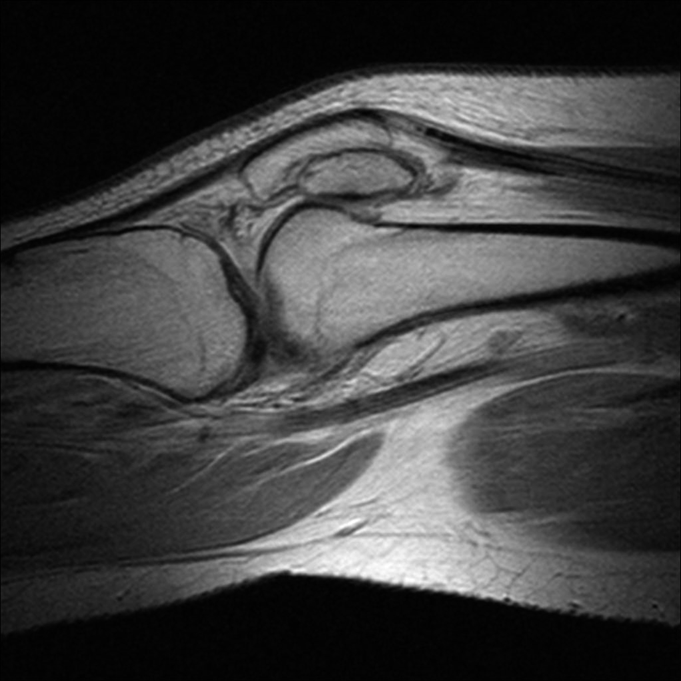
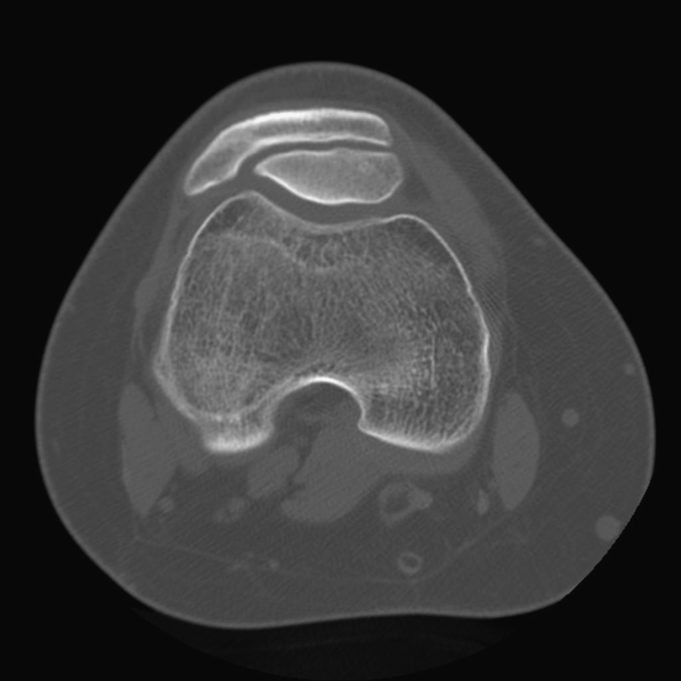
 Fig. 1
Fig. 1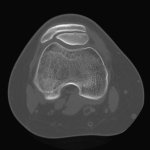 Fig. 2
Fig. 2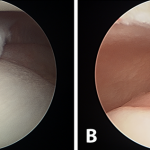 Fig. 3
Fig. 3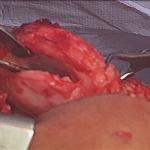 Fig. 4
Fig. 4 Fig. 5
Fig. 5