A five-year and two-month-old boy presented with a three-day history of pain in the right shoulder and fever of 103°F (39.4°C) without antecedent trauma. The white blood-cell count was 18,400 cells/mL, and the C-reactive protein level was 22 mg/dL. Radiographs and magnetic resonance images (Figs. 1 and 2) demonstrated findings consistent with osteomyelitis of the proximal part of the humerus. Because there was a concern of sepsis, the patient was transferred to our tertiary pediatric medical center. Following transfer, he was febrile, with a temperature of 40°C, and he had tachycardia (pulse rate, 160/min) and tachypnea (respiratory rate, 60/min). He was intubated in the emergency room, started on intravenous vancomycin and ceftriaxone, and admitted to the pediatric intensive-care unit. The C-reactive protein level and the erythrocyte sedimentation rate were 40.2 mg/dL and 42mm/hr, respectively. Ultrasonography was performed to evaluate for abscess formation (Fig. 3). No fluid collection was seen, but two thrombi were identified. One large thrombus involved the midportion of the subclavian vein, and the other filled the right brachial, cephalic, and basilic veins. Administration of enoxaparin was initiated to treat the deep venous thrombosis. There was no family history of coagulopathy, and no laboratory evidence of a hypercoagulable state. Respiratory insufficiency caused by septic pulmonary emboli required prolonged intubation and ventilatory support; bilateral chest tubes were placed to drain parapneumonic effusions, and vasopressors were used to maintain systemic perfusion. The patient was treated with antibiotics after a blood culture was positive. On hospital day 11, a repeat magnetic resonance imaging scan of the right humerus (Fig. 4) and the chest was acquired. It demonstrated osteomyelitis with adjacent pyomyositis and a small abscess posterior to the proximal part of the humerus. There were cavitary pulmonary lesions in multiple areas of both lungs.
On the basis of the magnetic resonance imaging findings and given the lack of clinical and laboratory evidence of improvement, surgical debridement of the proximal part of the humerus was performed. The child was extubated on postoperative day 3, and he improved clinically until he was transferred out of the intensive-care unit on postoperative day 7. By then, the laboratory indices had improved substantially (white blood-cell count, 11,500 cells/mL; erythrocyte sedimentation rate, 57 mm/hr, and C-reactive protein level, 2.4 mg/dL). He was discharged home on postoperative day 21. At the time of discharge, he had a full range of motion of the right shoulder with some soreness. The incision was healing well. Ultrasound examination of the right upper extremity at ten days after discharge showed that no thrombus was present. At fifteen days after discharge, administration of the vancomycin and enoxaparin was discontinued, and oral clindamycin therapy was begun. Three weeks later, the erythrocyte sedimentation rate was 7 mm/hr and the C-reactive protein level was <0.1 mg/dL. At the most recent follow-up visit, sixteen months after hospital discharge, the child had no symptoms in the right arm or shoulder. He had a full painless range of motion, excellent strength in the right upper extremity, and no evidence of a limb-length discrepancy. Radiographs revealed an open physis and healing osteomyelitis (Fig. 5). We recommended continued follow-up to evaluate for later physeal dysfunction and humeral deformity.
Proceed to Discussion >>Reference: McDonald JE, Copley LAB. Upper-extremity deep venous thrombosis associated with proximal humeral osteomyelitis in a child. A case report. J Bone Joint Surg Am. 2010;92:2121-4.
Deep venous thrombosis is rare in children and is usually associated with the use of intravenous catheters or with inherited hypercoagulable conditions. Deep venous thrombosis and septic pulmonary embolism have been increasingly reported in association with musculoskeletal infections in children. This phenomenon is thought to be due, in part, to the rising incidence of community-acquired methicillin-resistant Staphylococcus aureus as the causative organism. In our previous report of deep venous thrombosis associated with osteomyelitis in children, we noted that methicillin-resistant Staphylococcus aureus was the causative organism in eight of eleven children who had deep venous thrombosis but in only 24.4% of 201 children who did not have deep venous thrombosis. In that report of 212 children with osteomyelitis, thirty-one cases involved the upper extremity. However, all eleven of the deep venous thromboses were identified in association with lower-extremity infections, leading us to believe that upper-extremity infections are unlikely to be associated with deep venous thrombosis. Our review of the literature identified only one previous case report of an upper-extremity infection associated with deep venous thrombosis; this was in a twelve-year-old boy who developed osteomyelitis of the humerus, deep venous thrombosis of the basilic vein, and septic pulmonary embolism. The causative organism was Staphylococcus aureus. Stahlman et al. reported another entity, Lemierre syndrome, in which anaerobic bacteria (Fusobacterium) are associated with osteomyelitis and septic thrombophlebitis. However, with that entity, the thrombus forms in the internal jugular vein and is preceded by a pharyngeal infection, resulting in metastatic septic arthritis and osteomyelitis. We present this case report of a five-year-old boy with upper-extremity osteomyelitis and deep venous thrombosis to highlight the fact that the upper extremity can be so affected. We also want to emphasize the severity of the clinical illness that children with deep venous thrombosis demonstrate. In our previous report, seven of the eleven children with deep venous thrombosis and osteomyelitis were admitted to the intensive-care unit. The majority had marked elevation of laboratory infection indices, and all required surgical intervention, with an average of 2.6 surgical procedures per patient. The average length of the hospital stay was 30.6 days. The clinical course of the child in this report was quite similar. The treatment with appropriate antibiotics, aggressive surgical debridement, and anticoagulation probably prevented a worse outcome for this child. Awareness of this condition should lead physicians to evaluate children with musculoskeletal infection for deep venous thrombosis, regardless of the location of the infection, especially when the laboratory indices are markedly elevated in a child who presents with sepsis and requires intensive care. The initially selected antibiotic should adequately cover community-acquired methicillin-resistant Staphylococcus aureus, and every effort should be made to identify the foci of infection, with the physician anticipating that thorough surgical debridement will be performed when the child has been medically stabilized. Finally, the lungs should also be studied to evaluate for septic pulmonary embolism. When deep venous thrombosis and septic pulmonary embolism are identified, appropriate anticoagulation therapy should be initiated.
Reference: McDonald JE, Copley LAB. Upper-extremity deep venous thrombosis associated with proximal humeral osteomyelitis in a child. A case report. J Bone Joint Surg Am. 2010;92:2121-4.
Methicillin-sensitive Staphylococcus aureus
Streptococcus faecalis
Methicillin-resistant Staphylococcus aureus
Mycobacterium tuberculosis


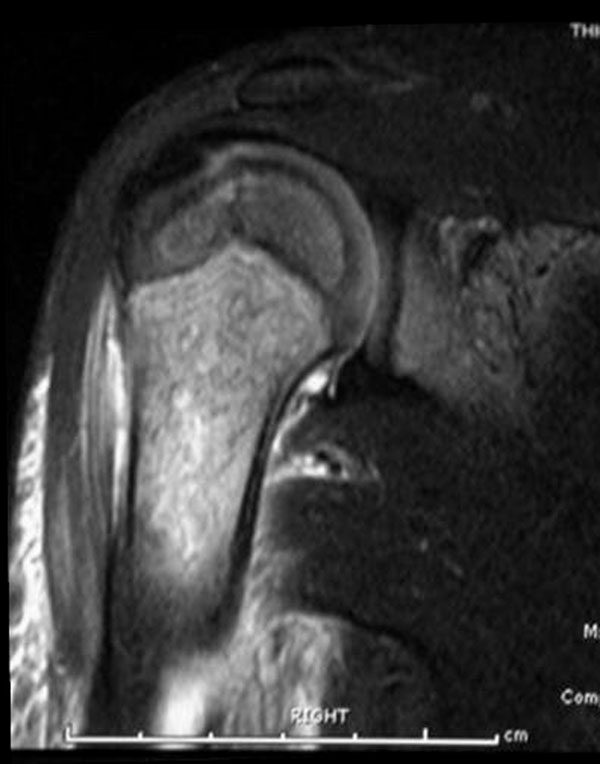
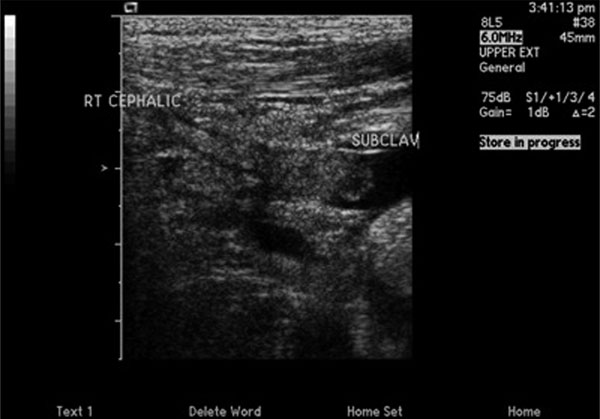
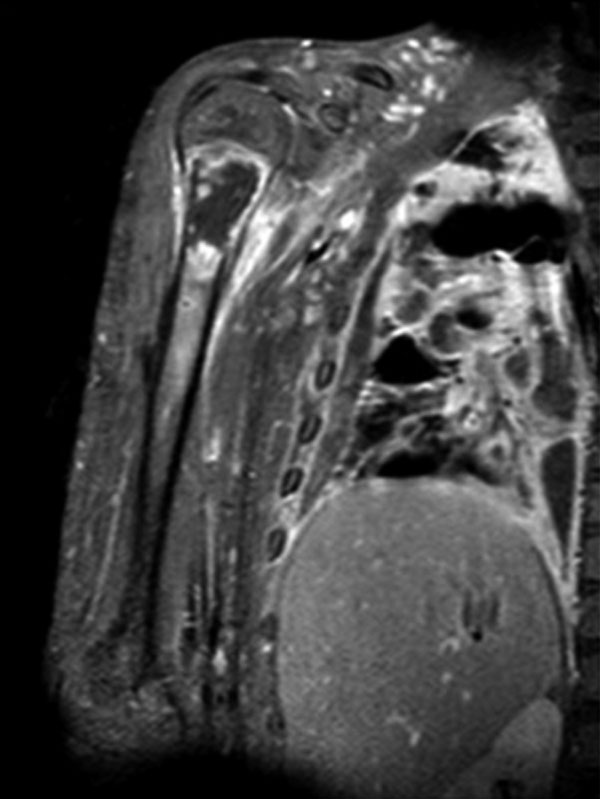
 Fig. 1
Fig. 1 Fig. 2
Fig. 2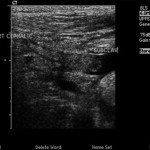 Fig. 3
Fig. 3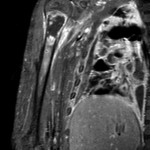 Fig. 4
Fig. 4 Fig. 5
Fig. 5