A thirty-eight-year-old woman presented with a two-year history of a traumatic pain in the left shoulder. The pain was insidious in onset, diffuse and dull, nonradiating, and nonprogressive. The patient reported that she did not have pain at rest but experienced pain with any activity and at night, particularly when lying on her left side. She otherwise felt well. Constitutional symptoms were absent, as were proximal pain or neurological symptoms. She had anteromedial elbow pain but no symptoms in any other joint. The patient was diagnosed with neurofibromatosis-1 at eight months of age. This patient initially presented as a child with a congenital pseudarthrosis of the tibia, which ultimately required surgery. She took no medications, had no allergies, was a nonsmoker, and worked as a cashier at a grocery store. The patient's mother and maternal aunt, a male sibling, and two of the patient's four children had neurofibromatosis-1. Clinical examination revealed a healthy-appearing woman. Her height and weight were within the normal range. Examination of the integument revealed multiple cutaneous neurofibromas and axillary freckling. Atrophy of the left supraspinatus and infraspinatus was noted, while the deltoid contour was well preserved bilaterally. No palpable mass or tenderness was noted around the proximal part of the humerus, with the exception of a neurofibroma lying just lateral to the acromion. No other masses were palpable around the shoulder or neck region. The range of motion of the shoulder consisted of active forward elevation of 100° and passive forward elevation of 110°, with active external and internal rotation that was 50% of that on the contralateral side. Passive motion was limited by pain at the extremes of motion. Strength testing was limited secondary to pain; however, subscapularis testing did demonstrate a positive lift-off test. There was no evidence of shoulder instability. A detailed examination of the axillary nerve demonstrated a persistent sensory deficit with no motor impairment of the deltoid or teres minor muscles. The remainder of the findings of the neurovascular examination of the upper extremity were normal. Examination of the neck revealed unremarkable findings; however, the patient had pain in the ipsilateral elbow. The results of blood tests, including a complete blood-cell count and measurements of the erythrocyte sedimentation rate, C-reactive protein level, and rheumatoid factor, were within normal limits. Radiographs revealed a varus deformity of the proximal part of the humerus and multiple well-circumscribed lateral scapular and proximal humeral lytic erosions. These lesions did not appear to extend into the glenohumeral joint (Fig. 1). Magnetic resonance imaging of the elbow revealed normal findings. However, magnetic resonance imaging of the shoulder (Figs. 2 and 3) demonstrated distension of the glenohumeral joint with a low signal on T1-weighted images, a high signal on T2-weighted images, and uniformly bright enhancement on post-gadolinium-injection images. The enhancing material encased the scapular neck as well as the proximal part of the humerus and the humeral diaphysis, entering well-defined osseous erosions, some of which had overhanging margins. The enhancing material was in contact with the axillary nerve within the quadrilateral space and appeared to erode all of the rotator cuff tendons, which were thin, heterogeneous, and irregular in contour (Fig. 3). A 1.5-cm superficial subcutaneous mass was also seen over the superolateral aspect of the shoulder (Fig. 2). There was no evidence of involvement of the teres minor on T2-weighted images (Fig. 4). The results of electrophysiologic studies of the axillary nerve were entirely normal. On the basis of the presentation and laboratory findings, an open biopsy of the lesion was performed, with use of a direct muscle-splitting approach, to exclude the possibility of an infection or a malignant lesion. The anterior head of the deltoid was found to be directly penetrated, and the mass was located immediately under the biceps tendon. It had eroded the lesser tuberosity, resulting in partial detachment of the subscapularis tendon. The mass extended anteriorly across the shoulder joint and into the glenoid neck, eroding the bone. A biopsy sample was obtained, and tissue was sent for histological and microbiological analyses. The mass had penetrated extensively into all of the periarticular soft tissue visible through the biopsy site. The results of the analysis of the frozen intraoperative sections were conclusive for the absence of infection, but because of the unknown nature of the lesion, an excisional biopsy was not performed. Following biopsy, a single suture anchor was inserted into the anterior aspect of the humerus to repair the torn subscapularis tendon. Tissue-culture results were negative, and histological analysis confirmed that the lesion was not an infection. Tissue sections revealed a moderately cellular spindle-cell proliferation set in a fine fibrillary collagen background. The spindle-cell nuclei ranged from oval-round to elongated and undulating with tapered ends. Occasional Wagner-Meissner bodies were present. The lesional cells demonstrated strong, diffuse positive immunostaining with antibodies against S-100 protein (Fig. 5).
The symptoms and neurovascular findings were unchanged following surgery. The case was reviewed by the orthopaedic team as well as an experienced peripheral nerve surgeon. An attempt at surgical resection of the mass was contemplated and discussed with the patient. This would have required excision of a segment of the axillary nerve as well as all of the periarticular soft tissues—i.e., the rotator cuff and capsule—and was associated with a substantial risk of additional joint dysfunction. In addition, neurofibromas are frequently highly vascular and pose a risk of substantial intraoperative blood loss. Furthermore, given the potential multiple etiologies of the patient's pain, a less invasive palliative procedure was not considered. Because of the substantial morbidity associated with the above options, and the patient's desire for nonoperative intervention, no additional surgery was planned. We chose to follow this patient closely at six-month intervals with serial magnetic resonance imaging and multidisciplinary clinical assessment to rule out local extension or malignant transformation. Malignant degeneration and/or severe pain with nerve dysfunction would require intervention. Although malignant transformation may not be entirely appreciated on magnetic resonance imaging, a history of worsening symptoms may be suggestive. At five years after the initial presentation, no substantial change was noted.
Proceed to Discussion >>Reference: Goel DP, Drosdowech DS, Turner RG, Lawendy A-H, Garvin G. Periarticular neurofibroma of the shoulder. A case report. J Bone Joint Surg Am. 2010;92:715-20.
Neurofibromatosis was first described by Dr. Friedrich von Recklinghausen in 1882. It is an autosomal dominant disorder, but up to half the cases may be the result of a spontaneous mutation. Neurofibromatosis encompasses a set of genetic disorders that cause tumors to arise within or attached to nerve trunks. Histologically, neurofibromas comprise all of the components of the peripheral nerves including fibroblasts and Schwann cells. The lesions can affect the development of non-nervous tissues such as bones and skin. The condition is classified into two distinct types: neurofibromatosis-1 and neurofibromatosis-2. Neurofibromatosis-1, also known as von Recklinghausen neurofibromatosis or peripheral neurofibromatosis, occurs in one in 4000 births and is characterized by multiple café au lait spots, Lisch nodules, optic gliomas, verrucous hyperplasia, and plexiform neurofibromas. Skeletal anomalies such as scoliosis and congenital pseudarthrosis of the tibia are associated with this disease. Occasionally, tumors may develop in the brain, within cranial nerves, or within the spinal cord. About half of the people with neurofibromatosis also have learning disabilities. In a retrospective review of forty-seven patients with neurofibromatosis, café au lait markings were noted in 87%; a positive family history, in 49%; scoliosis, in 53%; neurofibromas, in 19%; and pseudarthrosis of the tibia, in 19%. In 1988, the National Institutes of Health consensus panel defined criteria for the diagnosis of neurofibromatosis-1. For this diagnosis to be made, the patient must have two or more of the following: (1) six or more café au lait patches of >5 mm in diameter (or of >15 mm in diameter in adults), (2) two neurofibromas or one plexiform neurofibroma, (3) optic glioma, (4) two or more Lisch nodules (iris hamartoma), (5) axillary or inguinal freckling, (6) distinctive osseous lesions (sphenoid dysplasia, thinning of the cortex of long bones, dystrophic scoliosis, and/or vertebral scalloping), and (7) a first-degree relative with neurofibromatosis-1 as diagnosed according to the above criteria. Neurofibromatosis-2, also known as bilateral acoustic neurofibromatosis, is much more uncommon, occurring in one in 40,000 births. Neurofibromatosis-2 is characterized by multiple tumors within the cranial and spinal nerves and by other lesions of the brain and spinal cord. Schwannomas affecting both of the auditory nerves are characteristic of this subtype. Hearing loss beginning in the teens or early twenties is generally the first symptom. There are three types of neurofibromas: solitary, diffuse, and plexiform. While all three can be seen in neurofibromatosis-1, a plexiform neurofibroma is pathognomonic of that disease. These lesions produce extensive enlargement and nodularity of the affected nerve, creating a "bag of worms" appearance. On magnetic resonance imaging, the branching, reticulated, or serpiginous morphology of these tumors is more characteristic than the signal profile (decreased on T1-weighted images, increased on T2-weighted images, and enhanced with gadolinium). Our case demonstrated both clinical and imaging features suggestive of an arthropathy, including shoulder pain, a decreased range of motion, and periarticular erosions seen on the radiographs and magnetic resonance images. The clinical and imaging findings raised the possibility of an inflammatory arthritis, atypical infectious arthritis, gout, an intra-articular hemangioma, and an intra-articular neoplasm. Extension of the erosions beyond the normal confines of the joint was seen, but this feature may also be noted in other disease entities. While intra-articular involvement is rare with neurofibromatosis, bone dysplasia is common, as are osseous erosions secondary to neurofibromas. The presence of a nearby subcutaneous mass, peripheral nerve involvement, and a history of neurofibromatosis further increased the likelihood of this diagnosis. Histological findings compatible with a neurofibroma combined with the extensive ramifying morphology on magnetic resonance imaging indicated that this was an intra-articular plexiform neurofibroma. Approximately 5% to 10% of all plexiform neurofibromas undergo malignant degeneration. The follow-up evaluation of this patient with a focus on pain progression and changes on magnetic resonance imaging may subsequently demonstrate malignant degeneration. In a review of the literature, we found only three previously reported cases of intra-articular neurofibromatosis. Two cases affected the knee, and one involved the wrist. Till and Amos reported a case of a plexiform neurofibroma in the knee of a three-year-old boy. The diagnosis was confirmed with arthroscopic biopsy, but the lesion was deemed impossible to resect. The patient's symptoms resolved with nonoperative treatment. A few years later, pain developed in the same lower limb. This was attributed to limb-length inequality, and surgical periosteal stripping was performed in the normal limb in an attempt to stimulate growth. Lokiec et al. reported a case of neurofibroma affecting the knee of a five-year-old girl. The diagnosis was confirmed by arthroscopic biopsy. The lesion resulted in a Charcot joint and was treated with a knee brace. Grasland et al. reported on a forty-five-year-old woman with a ten-year history of wrist pain. Physical examination revealed only dorsal synovitis. Radiographs demonstrated a destructive arthropathy involving the carpometacarpal joints. The patient was treated with synovectomy and wrist fusion. The histological characteristics of the lesion were similar to those in our case, with the lesion containing hypertrophic noninflammatory synovial tissue that was entirely involved by a diffuse neurofibroma with plexiform features. In summary, this case serves as a reminder that, as orthopaedic surgeons, we must always be aware of the less common causes of shoulder pain and employ a multidisciplinary approach to achieving the correct diagnosis. The diagnosis in this case was facilitated by the patient's genetic history of neurofibromatosis-1. However, the imaging studies did not lead to a clear-cut diagnosis, and a biopsy was used to distinguish the rare intra-articular neurofibroma from the more commonly occurring erosive inflammatory arthropathy. Approximately half of malignant peripheral nerve sheath tumors are associated with neurofibromatosis-1 and are often due to malignant transformation of a neurofibroma. There is a 5% lifetime risk of a neurofibrosarcoma developing somewhere in the body, but it is not possible to state the risk for an individual lesion.
Reference: Goel DP, Drosdowech DS, Turner RG, Lawendy A-H, Garvin G. Periarticular neurofibroma of the shoulder. A case report. J Bone Joint Surg Am. 2010;92:715-20.
Intra-articular hemangioma
Neurofibrosarcoma
Periarticular neurofibroma
Synovial sarcoma


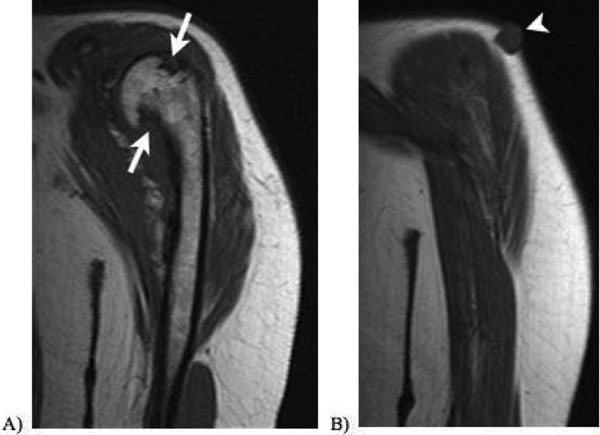
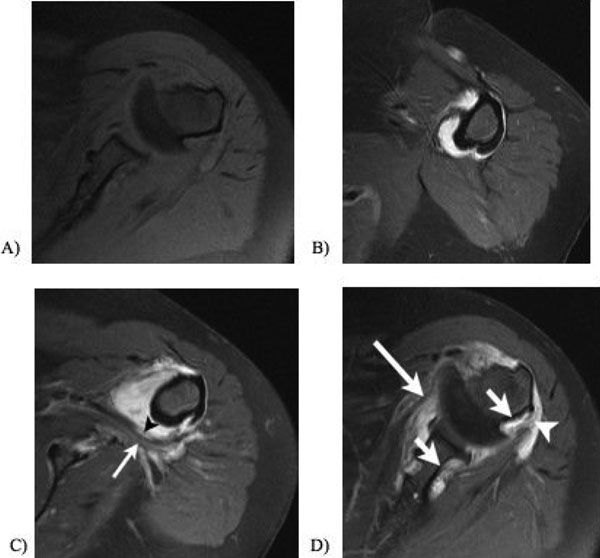
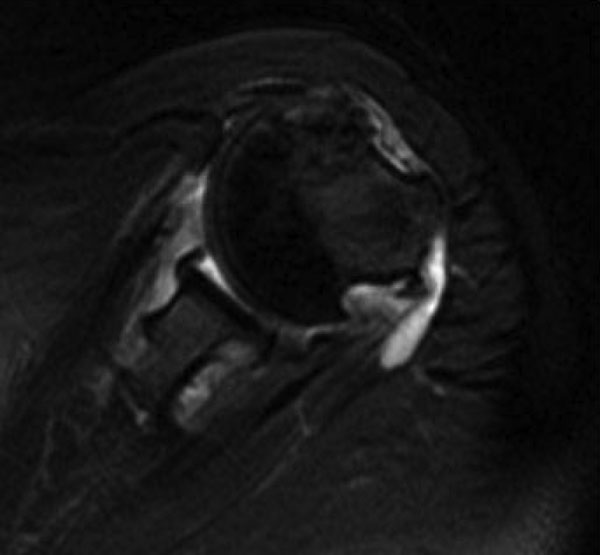
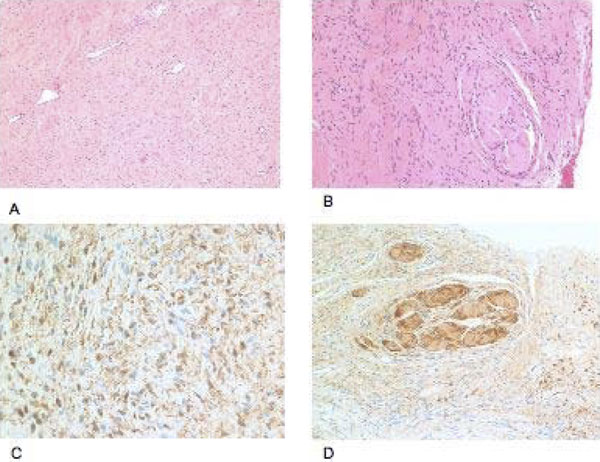
 Fig. 1
Fig. 1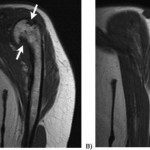 Fig. 2
Fig. 2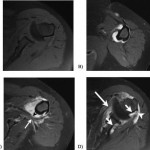 Fig. 3
Fig. 3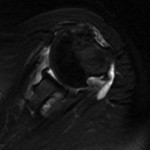 Fig. 4
Fig. 4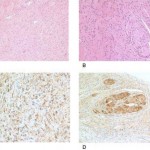 Fig. 5
Fig. 5