A Forty-nine-Year-Old Man with Ankle Pain for One Year
September 5, 2012
A forty-nine-year-old man presented with a one-year history of pain in the right ankle and no history of any traumatic causative event. Physical examination revealed a slight but diffuse swelling in the right ankle, which was painful with movement and during weight-bearing. All laboratory data, including the serum alkaline phosphatase level, were within normal limits. A radiograph demonstrated an ill-defined lucent lesion with cloudy mineralization from the head of the talus to the anterior one-third of the body of the talus (Fig. 1). A T1-weighted sagittal magnetic resonance image (Fig. 2-A) revealed a lesion that had low signal intensity and that extended from the talar head to the talar neck. The low signal area also extended beyond what seemed to be the posterior margin of the tumor. A short tau inversion recovery (STIR) image (Fig. 2-B) revealed high signal intensity throughout the entire talus (suggesting bone marrow edema) and the presence of an effusion (suggesting inflammation). An extraosseous tumor was seen in the anterior aspect of the talar neck. A plain computed tomographic scan revealed cortical destruction of the anterior aspect of the talar neck. A bone scan and positron emission tomography with use of [18F]-2-fluoro-2-deoxy-D-glucose (FDG-PET) showed uptake only in the right ankle. An open biopsy was done (Fig. 3).
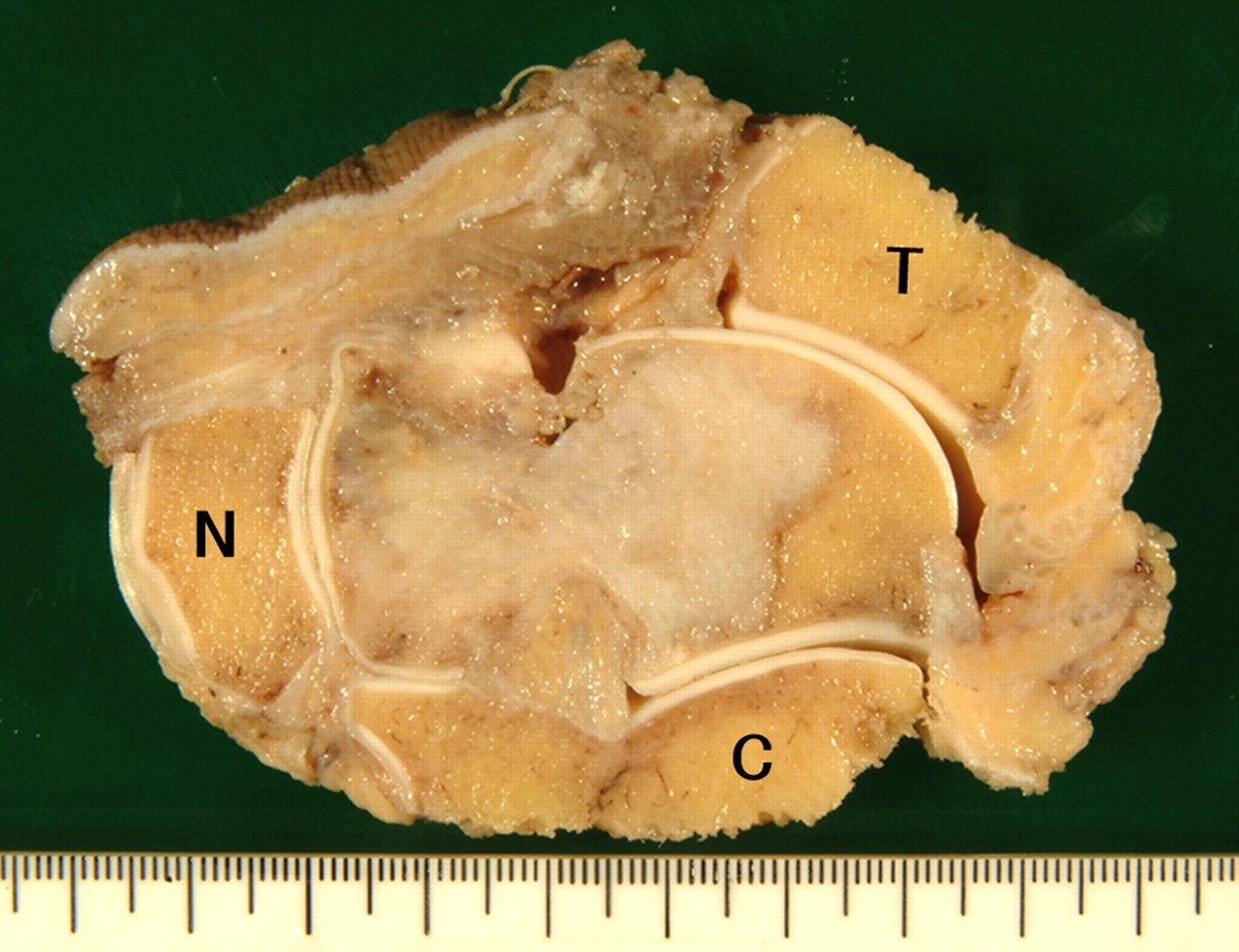
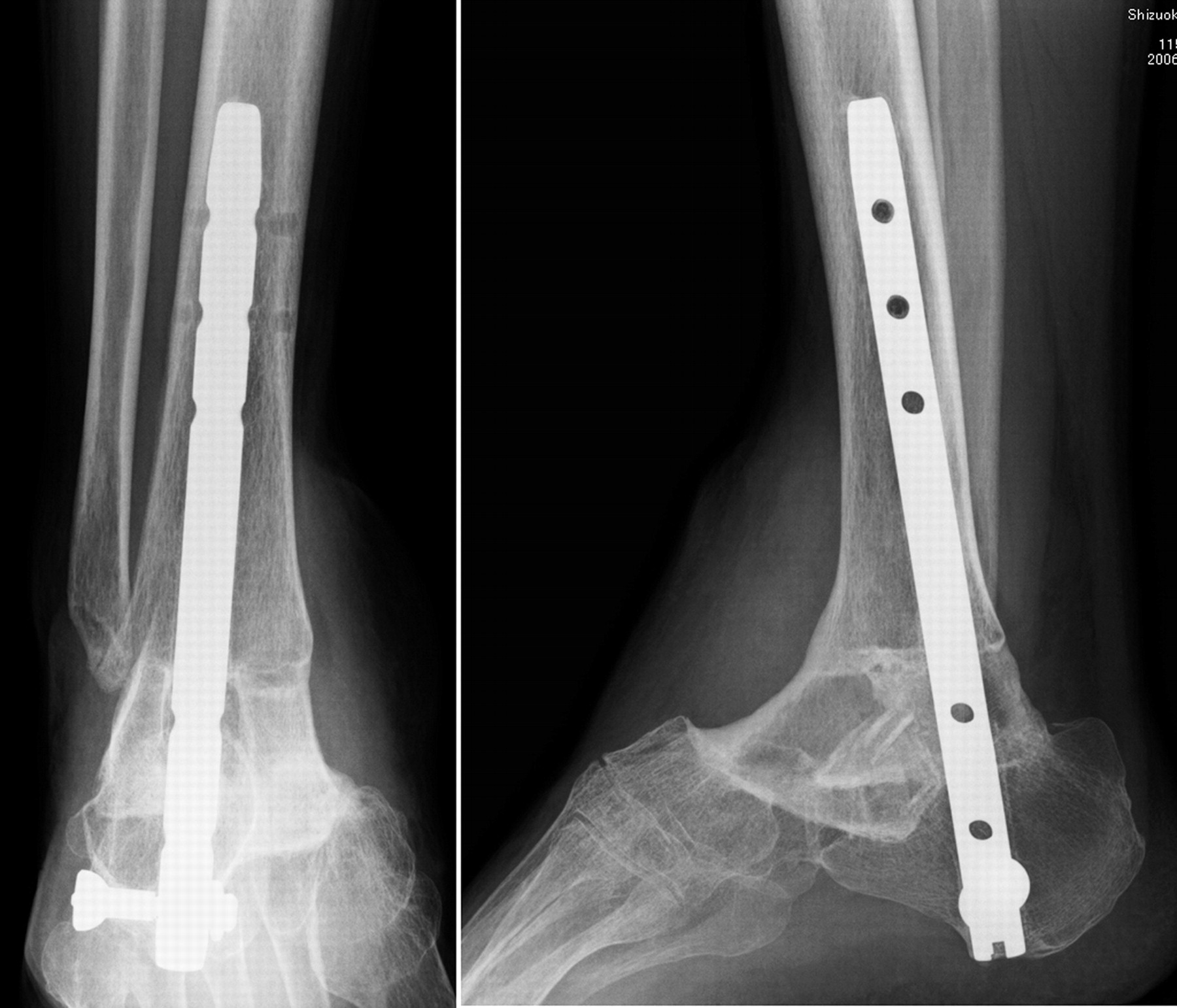
The histological examination of the biopsy revealed that the lesion was a high-grade fibroblastic osteosarcoma (Fig. 3). Preoperative systemic chemotherapy, consisting of two courses of cisplatin, two courses of high-dose methotrexate, and two courses of ifosfamide plus doxorubicin, was administered intravenously over the course of twelve weeks. After chemotherapy, the pain and swelling disappeared. The posterior part of the body of the talus demonstrated normal bone-marrow intensity on repeat magnetic resonance imaging. In addition, extraosseous tumor in the anterior aspect of the talus had shrunk, and the ankle joint effusion was no longer visible on magnetic resonance imaging. Uptake of FDG-PET also decreased after chemotherapy. From these physical and radiographic findings, preoperative chemotherapy was believed to have been effective. Two methods of surgery were proposed to the patient after completing chemotherapy: below-the-knee amputation and a limb-salvage procedure. After thorough discussion, the patient gave his informed consent for the limb-salvage procedure. The operation was begun by making bilateral parallel skin incisions along the medial neurovascular bundle and laterally along the peroneus longus muscle. The biopsy scar was resected with a 2-cm margin. The distal parts of the tibia and fibula were transected just above the attachment of the joint capsule. Distally, an osteotomy of the calcaneus was done just below the sustentaculum tali along the groove for the flexor hallucis longus. The anterior resection line was between the navicular and the medial cuneiform. Thus, the talus was resected together with its surrounding tissues (Fig. 4). After a wide resection, ankle arthrodesis was performed with use of an intramedullary nail and autogenous bone graft from the ipsilateral ilium. Two blocks of iliac bone were inlaid on the medial and lateral sides of the nail with the cancellous surfaces of the graft facing the cancellous bone in the cut surface of the tibia and calcaneus. Supplementary cancellous bone chips were added around the host-graft junction. To fill the dead space and skin defect, a free latissimus dorsi musculocutaneous flap was harvested and placed over the iliac bone graft. A vascular anastomosis to the anterior tibial artery and vein was performed so that the grafted bone would be covered by a vascularized muscle. Histological examination of the surgical specimen revealed clear resection margins and chemotherapy-induced tumor necrosis of 90%. A below-the-knee splint was worn by the patient for four weeks postoperatively, at which point he was permitted to walk with a patellar tendon-bearing brace. After completing seven courses of postoperative chemotherapy, the patient was able to return to work. Union between the distal part of the tibia and the grafted iliac bone was not achieved after one year. Consequently, dynamization of the nail by removal of the proximal locking screws was done, and two months later, bone union was achieved (Fig. 5). The result of surgical treatment, as measured with use of the functional rating system of the Musculoskeletal Tumor Society (MSTS), was 90%. The numerical values achieved by our patient in the six categories included in this rating system were 5 points for the category of pain (none), 4 points for function (heavy labor being restricted but no restriction in patient’s lifestyle), 5 points for emotional acceptance, 4 points for supports (a shoe-type orthosis was necessary only outdoors), 4 points for walking ability (continuous outdoor walking was possible for more than an hour but walking uphill was a bit difficult), and 5 points for gait (no alteration). Disability was measured with use of the Toronto Extremity Salvage Score (TESS), which ranges from 0 to 100, with higher scores indicative of less disability. The patient had a score of 89. He continued to be disease-free forty-seven months after surgery and was able to walk with an orthotic device in his shoe.
Proceed to Discussion >>Reference: Katagiri H, Takahashi M, Takagi T, Nakagawa M. Osteosarcoma of the talus treated successfully with limb-sparing surgery. A case report. J Bone Joint Surg Am. 2008;90:869-74. doi:10.2106/JBJS.G.00040
Osteosarcomas typically affect the metaphyseal part of long bones, with the knee being affected in almost 50% of cases. These tumors most frequently occur in the second decade of life. Excluding osteosarcoma of the jaw, 79% of osteosarcomas arise in long tubular bones. In patients who are older than forty years, however, osteosarcoma tends to occur in atypical areas, such as axial bone, and only 51% arise in long tubular bones. It is also reported that foot osteosarcomas tend to occur in older patients. Our patient was forty-nine years of age. The reported prevalence of osteosarcoma arising in the foot is only 0.5% to 1.3% of all osteosarcomas. Moreover, almost half of osteosarcomas of the foot are located in the calcaneus. Osteosarcoma of the talus is very rare. It was reported by Biscaglia et al. that only three of 1929 cases of osteosarcoma (0.2%) arose in the talus. We found only two well-documented case reports in the literature; in both, the neck of the talus was the origin. In the case of our patient, the osteosarcoma also arose in the neck of the talus and extended to the talar body and talar head. Biscaglia et al. reported that five of twelve osteosarcomas of the foot were low grade and that eight of twelve patients survived with no evidence of disease. However, only one of three patients with talar involvement survived; the other two patients died of the disease. Both patients in the case reports by Amini and Colacecchi and Matsumoto et al. and one patient in the series by Choong et al. also died of the disease. Thus, only one of six patients reported in the literature has survived, and all six had been treated with amputation. Even the patient with a parosteal osteosarcoma, which is histologically of lower grade than conventional osteosarcoma, eventually required amputation. In lower extremity osteosarcoma, there are two options for achieving local control: amputation or a limb-sparing procedure. When sufficient margins of resection can be achieved, limb-sparing surgery with use of various reconstruction techniques (such as arthrodesis, allografting, or endoprosthetic arthroplasty, as compared with amputation) has become the contemporary standard treatment for osteosarcoma of the extremity. However, below-the-knee amputation seems to be the standard operation for osteosarcoma of the foot because the procedure is associated with good local tumor control, excellent postoperative function, a low complication rate, and technical feasibility. The drawbacks of below-the-knee amputation are that a prosthetic limb is always necessary and that some patients have phantom limb pain and chronic episodes of skin breakdown. A limb-salvage procedure, on the other hand, may provide better patient satisfaction and the ability to walk without an artificial leg. Nevertheless, limb-sparing surgery for foot osteosarcoma has drawbacks and limitations. First, the close anatomic confines of the ankle and foot make it technically difficult to achieve a sound oncologic margin of resection. Second, the limb-salvage procedure cannot be performed on patients who have extensive soft-tissue involvement, because the foot and ankle have only thin soft tissues and little muscular coverage of the bone. In addition, some patients may require a free musculocutaneous flap to fill the dead space and skin defect, as was required in our patient. Third, the complications following a limb-sparing procedure are more frequent compared with those encountered after amputation. Fourth, early complications such as deep infection, soft-tissue necrosis, venous thrombosis, or damage to vascular structures can prolong hospitalization and cause a delay in the administration of chemotherapy. Fifth, with limb-sparing ankle arthrodesis, complete bone union is necessary to achieve painless and stable walking, and complete bone union normally takes several months or more to achieve. However, once bone union has occurred, painless walking is possible with only the aid of a shoe-type orthosis. Controversy still persists about whether limb-salvage surgery provides improved function and better quality of life than that provided by amputation. Previous studies support the improved function afforded by limb-sparing surgery. However, most of the patients in these studies had osteosarcoma about the knee or hip joint. Osteosarcoma in the foot or ankle is rare: only one patient in the series by Renard et al. and only one patient in the study by Hopyan et al. were treated with below-the-knee amputation. The MSTS scores for these two patients were 60% and 70%, respectively. In a study in which foot and ankle tumors were analyzed, two patients were treated with below-the-knee amputation and had MSTS scores of 83% and 70%. In comparison, our patient had an MSTS score of 90%. Davis et al. reported that the mean TESS for a group of patients who had below-the-knee amputation was 75.6, whereas the score for a matched group of patients who had limb-sparing surgery was 85.71. They concluded that there was a trend toward increased disability for patients in the amputation group compared with patients in the limb-sparing group. In our patient, the TESS was 89, which was higher than the literature-reported scores of the patients who had below-the-knee amputation. Patients with osteosarcoma of the foot are usually not considered as candidates for limb-salvage surgery. With accurate imaging, a good response to chemotherapy, and advanced operative techniques, some individuals may undergo limb-sparing surgery with acceptable outcomes.
Reference: Katagiri H, Takahashi M, Takagi T, Nakagawa M. Osteosarcoma of the talus treated successfully with limb-sparing surgery. A case report. J Bone Joint Surg Am. 2008;90:869-74. doi:10.2106/JBJS.G.00040
Ewing sarcoma
Osteosarcoma
Multiple myeloma
Hodgkin lymphoma
Fibrosarcoma



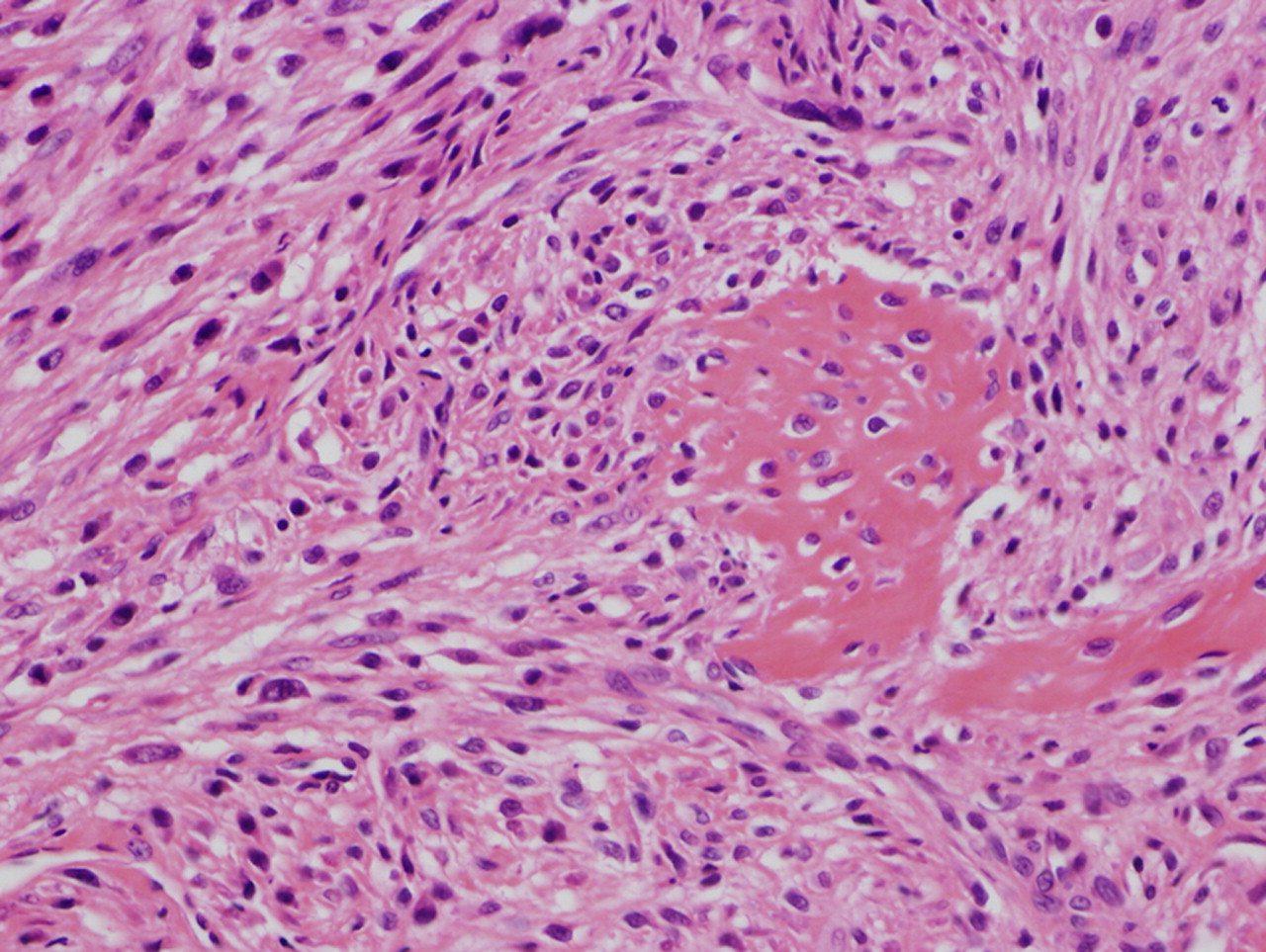
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3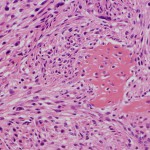 Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5
Fig. 5