A Forty-six-Year-Old Man with a Right Thigh Mass
April 6, 2011
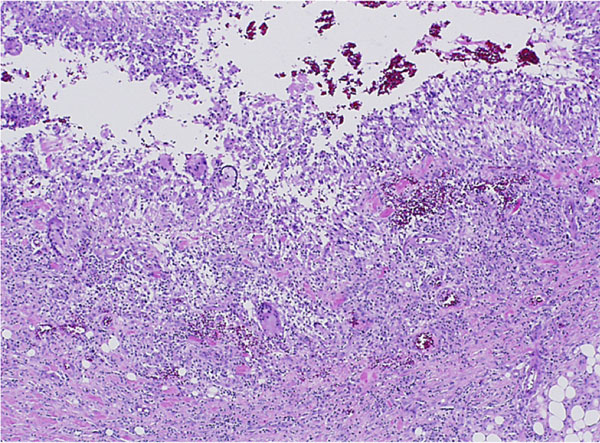
A forty-six-year-old man who was otherwise healthy was seen in the orthopaedic oncology clinic because of a mass in the proximal aspect of the right thigh. This mass was first noticed six weeks earlier, after he had experienced "pressure" in this area while cycling. His primary care physician initially treated him conservatively, thinking this was likely from an injury. As the mass slowly enlarged, concern for a primary oncologic process was raised. The patient reported no functional limitation, no pain, and denied having any fevers, chills, puncture wounds, or other trauma to this area. There was only a remote history of depression and an uncomplicated appendectomy thirty years previously. He took no medication and had no drug allergy. He did not smoke or use intravenous drugs, and he denied having previous transfusions. He consumed alcohol socially and reported a single long-term monogamous relationship. For the previous twenty years, he was employed as a laboratory manager in a finch aviary where he routinely cleaned cages. He reported no pets and no recent travels. On examination, the circumference of the right thigh was noticeably larger than that of the left. There were no overlying dermatologic changes, cellulitis, or fluctuant masses. There was a deep, well-circumscribed, firm mass on the medial aspect of the proximal part of the right thigh. Inguinal lymphadenopathy was not appreciable, and motor, sensory, and vascular testing was unremarkable. The Tinel test was also negative. A magnetic resonance imaging scan revealed a 5 × 3.8 × 4.3-cm mass abutting the femoral neurovascular bundle in the adductor musculature of the proximal part of the right thigh. The mass was characterized by areas of subtle increased T1 signal and high T2 signal with heterogeneous enhancement on images after the administration of contrast medium (Figs. 1 and 2). Computed tomography of the chest revealed a 2 × 1.7-cm nonspecific mass in the left lower lobe and several mediastinal lymph nodes, measuring <1 cm, bilaterally. These findings raised the concern for a primary metastatic soft-tissue sarcoma, and a core-needle biopsy was performed (Figs. 3 and 4).
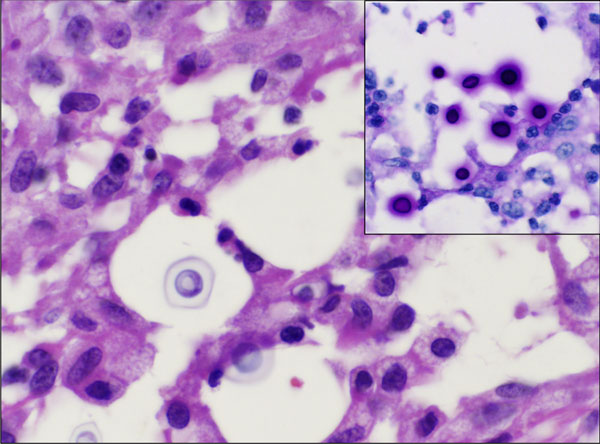
Histological analysis of the biopsy specimen revealed a florid granulomatous response (Fig. 3), scattered small round organisms, and no evidence of malignant cells. Because of the patient's occupational exposure, staining for periodic acid-Schiff, Grocott-Gomori methenamine silver, and mucicarmine was undertaken. These stains specifically enhance the polysaccharide capsule of yeast, which revealed in this patient the thick-walled, encapsulated cryptococcal organisms (Fig. 4). The patient was referred to the infectious disease service, and fluconazole monotherapy was begun immediately. He was found to have a positive (1:32) cryptococcal titer, negative findings on testing for the human immunodeficiency virus (HIV), a normal CD4 count, and an appropriate immunologic response to anergic skin testing. The risks and benefits of surgical debridement were discussed, and the thigh abscess was ultimately decompressed. Surgical findings included a well-circumscribed mass consisting of thick mucinous fluid. After evacuation, the pseudocapsule of the mass was excised, and the wound was irrigated and closed over a drain. Oral fluconazole was continued postoperatively per the recommendation of the infectious disease consultant. The patient recovered without incident and was discharged home on postoperative day 2. Cryptococcus neoformans var. gattii was isolated from intraoperative cultures, and pathologic evaluation was consistent with the diagnosis of a cryptococcal abscess. The surgical incision healed uneventfully. At the time of the one-year follow-up, the activity level of the patient was nearly normal and he reported no symptoms of a systemic infection.
Proceed to Discussion >>Reference: Gaskill T, Payne D, Brigman B. Cryptococcal abscess imitating a soft-tissue sarcoma in an immunocompetent host. A case report. J Bone Joint Surg Am. 2010; 92:1890-3.
Cryptococcus neoformans is an opportunistic yeast commonly found in soil contaminated by bird feces throughout the world. It is an encapsulated organism, demonstrating a complex polysaccharide capsule with antiphagocytic properties. Low concentrations of anticryptococcal antibodies (typically immunoglobulin M) are normally found in immunocompetent people because of daily exposure. Although exposure in some regions of the world is nearly ubiquitous, this organism rarely causes clinically important infection in immunocompetent hosts. In contrast, it has become a notable opportunistic infection in those possessing a compromised cell-mediated immune response. Two varieties of Cryptococcus exist. Neoformans var. neoformans is more prevalent in temperate climates, and neoformans var. gattii is more prevalent in tropical and subtropical areas. Inoculation of Cryptococcus is presumed to occur through inhalation of aerosolized yeast. The normal immune system is capable of eliminating or sequestering this pathogen, rendering it innocuous. In an immunosuppressed patient, reactivation with hematogenous spread and disseminated disease is possible. In these patients, the central nervous system is most commonly involved, although there have been reports of skin lesions, septic arthritis, prostatitis, hepatitis, osteomyelitis, and intestinal infections. A current search of the literature for cryptococcal osteomyelitis or subcutaneous abscess reaffirms its rarity. Since 1953, the cases of less than sixty patients have been reported in the English-language literature, with the largest series including seven patients. These cases include both pediatric and adult patients and most commonly involve the vertebrae. Osteomyelitis of the ribs, skull, clavicle, femur, tibia, humerus, scapula, and ilium is also described. The cases of five patients initially raised concern regarding neoplasia because of marrow signal changes on magnetic resonance imaging or a lytic appearance on radiographs. None of those cases involved soft-tissue masses outside the central nervous system. An inflammatory pseudotumor can also present clinically as a soft-tissue mass and has been associated with cryptococcal organisms. Histologically, this disorder is characterized by abundant spindle cells, making it quite distinct from a soft-tissue abscess. Cases of cryptococcal infections in an immunocompetent host have been reported and primarily include pulmonary manifestations and cutaneous lesions. A history of a hobby or occupational exposure to soil, dust, sticks, or bird feces was noted in most cases. Because of the typical quiescent nature of isolated pulmonary Cryptococcus, and because spontaneous resolution of infection can occur, data describing the natural history and management in this setting are scant. It is important to recognize, however, that untreated cryptococcal infection has resulted in severe pulmonary infections with respiratory failure, or systemic dissemination even in immunocompetent hosts. Fluconazole appears to be the mainstay of treatment of pulmonary and cutaneous Cryptococcus infection in these patients. What has yet to be solidified in the literature is the appropriate duration of treatment for the immunocompetent host. It is unclear how infections in apparently immunocompetent patients occur. One possibility is that an overwhelming pathogen load or transient immunosuppression allows hematogenous seeding of cryptococcal organisms. It is also possible that some patients possess an unidentifiable immune abnormality making them susceptible to certain strains of cryptococcal organisms. Interestingly, evidence demonstrating that specific serotypes affect normal and immunocompromised hosts disproportionately has emerged. Those reports have indicated that Cryptococcus neoformans var. gattii, as isolated in this patient, is predominantly found in immunocompetent hosts. Although enzyme production and antiphagocytic capsular properties vary by serotype, the true importance of these findings remains unknown. The case of our patient is unusual in that it represents an isolated soft-tissue cryptococcal abscess without osseous involvement in an apparently immunocompetent host. History and physical examination were unable to expose any mechanism capable of locally inoculating the organism. HIV, CD4, and skin testing revealed no evidence of immune system compromise, and no immune-modulating medications were being taken. Assuming local inoculation did not occur, the most reasonable explanation for dissemination in this patient is hematogenous spread. This likely occurred after long-term and high-concentration exposure to cryptococcal organisms over two decades of handling bird feces while he was employed in an aviary. The lung nodules identified on computed tomography presumably represent a byproduct of this exposure. The radiographic and clinical presentation in this patient is also notable. The patient described a slow growing, deep-seated, painless mass that was indistinguishable from that expected of a soft-tissue sarcoma. Appropriate imaging, including a magnetic resonance imaging scan and a staging computed tomography scan, was ordered. The magnetic resonance imaging scan revealed a heterogeneously enhancing mass on T1 and T2-weighted images, and chest computed tomography showed a 2-cm mass and several nodules measuring <1 cm, all of which could be consistent with metastatic sarcoma. Reaffirming the importance of tissue diagnosis prior to treatment, the true identity of the mass was apparent only after core biopsy and specific histologic staining. Treatment of systemic manifestations of cryptococcal infections remains debated and nonstandardized. Surgically, our management was akin to that for any other large soft-tissue abscess, and debridement was recommended. Pharmacological treatment is not as clearly defined. Most experts suggest antifungal agents should be tailored on the basis of the site of infection and immune status. Some evidence suggests miconazole and ketoconazole are unable to achieve therapeutic concentrations in some tissues, and flucytosine results in resistance if used as monotherapy. Successful treatment has been reported with amphotericin B, itraconazole, ketoconazole, and fluconazole with or without flucytosine. The literature supports the use of azole compounds for several weeks to months to achieve complete healing on the basis of the site and immune status. In this patient, surgical debridement in conjunction with twelve weeks of oral fluconazole was successful in treating this soft-tissue abscess. At eighteen months postoperatively, no recurrent disease was evident. The rapid resolution of the abscess provides some evidence that surgical decompression, along with antimicrobial therapy, can be effective in managing this entity. Despite these reports, little comparative data are available to guide treatment.
Reference: Gaskill T, Payne D, Brigman B. Cryptococcal abscess imitating a soft-tissue sarcoma in an immunocompetent host. A case report. J Bone Joint Surg Am. 2010; 92:1890-3.
Fibrosarcoma of the thigh
Extraosseous giant cell tumor
Soft-tissue tuberculous infection
Fungal or yeast infection of the thigh

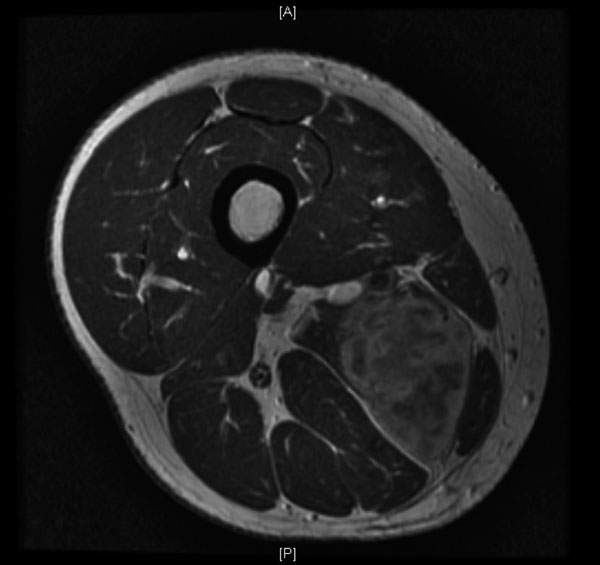

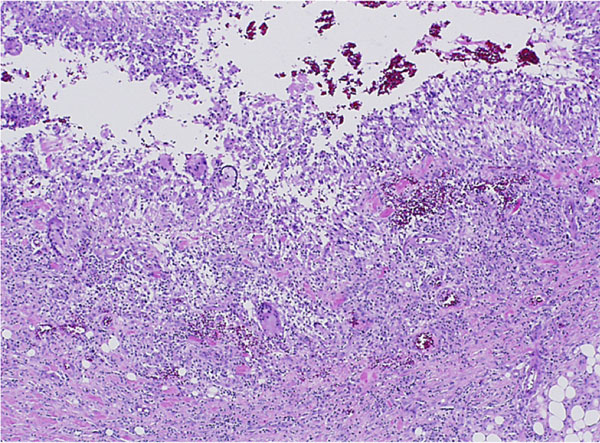
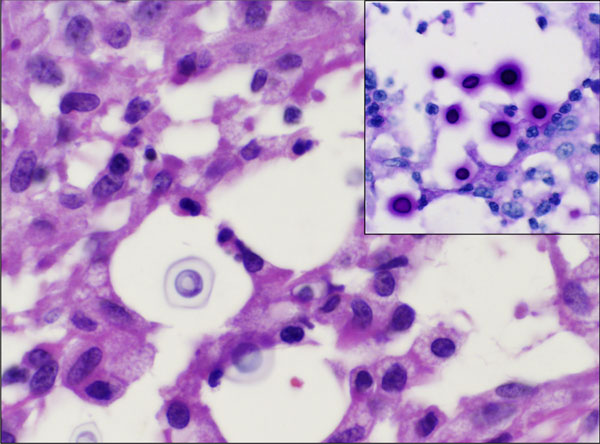
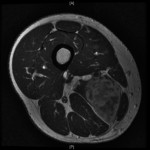 Fig. 1
Fig. 1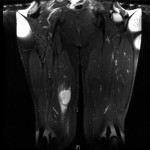 Fig. 2
Fig. 2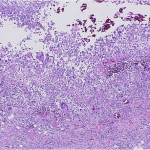 Fig. 3
Fig. 3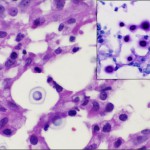 Fig. 4
Fig. 4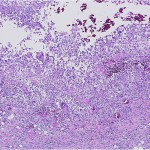 Fig. 3
Fig. 3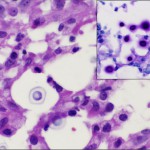 Fig. 4
Fig. 4