A Twenty-two-Year-Old Male Swimmer with Acute Leg Weakness
April 20, 2011
A twenty-two-year-old Olympic-caliber collegiate swimmer presented to the emergency department with complaints of progressive weakness in both lower extremities. Two days earlier, the patient had noted sharp pain in the neck and the middle part of the back on waking; however, he was able to complete his morning swimming practice. He could not recall a traumatic event, but he had participated in a rigorous swim practice the day before. One day before presentation, the pain completely resolved. However, on the day of presentation, the patient had awoken from a nap with searing interscapular back pain and decreased strength in the legs. He reported no bladder or bowel difficulties at that time. He was unable to stand and was immediately taken to the emergency department. The medical history was unremarkable for any previous spine trauma. The surgical history was noncontributory, and the patient reported no previous bleeding dyscrasias. He was not taking any medications, and he reported no history of illicit drug use. Manual motor testing revealed normal strength throughout both upper extremities. The patient had strong biceps, triceps, and brachioradialis reflexes and had no difficulty with rapid fine alternating motions. He had a negative Hoffman reflex, a negative inverted radial reflex, and no upper motor neuron findings in the upper extremities. In the lower extremities, however, the patient had no strength in the iliopsoas, quadriceps, hamstrings, tibialis anterior, extensor hallucis longus, or gastrocnemius/soleus muscles. The patient had absent patellar and Achilles tendon reflexes bilaterally, and he had no rectal tone. He had no sensation to light touch, pain, or temperature from the nipple line down to the toes. Blood tests were unremarkable, with a hematocrit of 42.4%, an international normalized ratio of 1.1, a prothrombin time of 13.8 seconds, a partial thromboplastin time of 26.3 seconds, a C-reactive protein level of 0.2 mg/dL, and an erythrocyte sedimentation rate of 2 mm/hour. A drug screen was negative for any illicit substances. The emergency department administered intravenous Decadron (dexamethasone) immediately, given as a bolus of 30 mg/kg of body weight, followed by infusion at 5.4 mg/kg/hr. The infusion was continued for approximately two hours and then was discontinued by the surgical team. Radiographs revealed no acute changes in the cervical, thoracic, or lumbar spine. Magnetic resonance imaging revealed a lesion extending from C2 to L3, located ventral to the spinal cord from C2 to T12 and dorsal to the spinal cord from T12 to L3 (Figs. 1 and 2). Minimal compression of the spinal cord was noted below T10. A spinal angiogram demonstrated no vascular lesions.
Within four hours after presentation, the patient was taken to the operating room for a decompressive procedure. He was placed in the prone position on a Jackson flat-top table. Multilevel noncontiguous laminectomies were performed at T2, T4, T6, and T8, with a partial laminectomy at T9. A large hematoma, creating substantial pressure on the spinal cord, was encountered. The performance of partial laminectomies minimized the potentially destabilizing effects of the extensive decompression and, because the hematoma was still in a liquid state, the segments above and below each laminectomy level could be evacuated circumferentially from around the spinal cord with gentle manipulation and suction. The laminectomies were performed with use of a high-speed burr and Kerrison rongeurs, with care being taken to minimize disruption of the facet joints. No obvious arteriovenous malformation or active bleeding was noted. Several submuscular drains were left in place, just dorsal to the spine, and the patient was transferred to the intensive-care unit for further care. By the fourth postoperative day, the patient had experienced dramatic recovery of lower extremity strength and restoration of patchy areas of sensation to light touch. By four months postoperatively, the patient had full strength in both lower extremities with full sensation, and he had no residual bowel or bladder symptoms. A repeat magnetic resonance imaging scan with contrast showed no evidence of residual epidural hematoma or spinal cord compression and a normal spinal cord signal (Fig. 3). The patient had returned to swimming, although not at his prior competitive level. In terms of overall subjective assessment, the patient thought that he was 90% back to normal. Of note, a hematologic workup did not identify any coagulopathies.
Proceed to Discussion >>Reference: Fleager K, Lee A, Cheng I, Hou L, Ryu S, Boakye M. Massive spontaneous epidural hematoma in a high-level swimmer. A case report. J Bone Joint Surg Am. 2010; 92: 2843-6.
Spontaneous spinal epidural hematoma is defined as an epidural hematoma developing without any specific cause such as trauma, vascular malformation, neoplasm, or systemic hemorrhagic tendency. It is a rare disorder, with a reported incidence of 0.1 case per 100,000 population per year, but, to our knowledge, it has not been reported in an otherwise healthy, Olympic-level athlete. It presents in all age groups, but most cases occur after the fourth decade, with a male:female ratio of 1.4:1. Classically, patients report sharp, severe, radicular back pain, followed by neurological symptoms of cord compression. Most reported cases involve the cervicothoracic and thoracolumbar regions, and the hematoma is typically dorsal to the spinal cord. The etiology of the hematoma has been debated, but, because of its typical dorsal location, it is thought to be venous in nature and related to the posterior internal vertebral venous plexus. Hypertension, coagulopathy, cocaine and alcohol, and straining have been identified as predisposing factors by some authors. The differential diagnosis of this condition includes acute ischemia of the spinal cord, acute herniated intervertebral disc, epidural abscess, neoplasm, spondylitis, lipoma, transverse myelitis, and dissecting aortic aneurysm. Magnetic resonance imaging is the diagnostic test of choice, and an early diagnosis is critical to prevent further neurological deterioration, although complete recovery without surgical intervention has been reported. The primary factors determining neurological recovery are the location of the involved vertebral segments, the patient's baseline neurological condition, and the time between diagnosis and surgical decompression. Recovery is significantly better when decompression is performed in less than thirty-six hours after the initial symptoms in patients with complete sensorimotor loss and in less than forty-eight hours after the initial symptoms in patients with an incomplete sensorimotor deficit. Patient age and sex and the location and size of the hematoma do not appear to influence the outcome. Our patient had a classic presentation. He experienced sharp upper back pain that radiated first to the neck and later down the spine. He had no neurological deficits at that time and was able to continue with his normal activities the following day. Approximately forty-eight hours after the initial symptoms, he developed numbness and weakness in the lower extremities, which eventually progressed to complete paraparesis. Similar to the findings in many previous case reports, the etiology of our patient's condition was unclear. He was a young, elite-level athlete with no relevant medical history. He had no history of trauma, was not receiving anticoagulation treatment, had no underlying coagulopathies, was not hypertensive, and tested negative for illicit substances. The only inciting event may have been a rigorous swimming practice, which is consistent with previous reports of "straining" as an etiology of a spontaneous spinal epidural hematoma. The pain, however, did not begin until approximately twelve hours after that physical exertion. In addition, the patient had participated in equally strenuous activities for many years as an athlete and had never experienced such symptoms. To our knowledge, the case described here is the first reported case of a spontaneous spinal epidural hematoma spanning the cervical, thoracic, and lumbar spine in an elite athlete, and the lesion in our patient appears to be the most extensive spinal epidural hematoma reported thus far. There have been several case reports of spontaneous spinal epidural hematomas following routine exercise, but those lesions were in patients who were not high-level athletes. There was one similar case in a young, healthy, professional trumpet player who developed a hematoma while playing the trumpet. As in the case of our patient, it is unclear why, after years of performing the same high-level activity, the trumpet player would suddenly develop a spinal epidural hematoma. We report the case of our patient to increase awareness among physicians and training staff working with collegiate and professional athletes in order to expedite the diagnosis. We believe that a rapid workup followed by timely surgical intervention can lead to an excellent functional outcome for patients with this rare but potentially devastating condition.
Reference: Fleager K, Lee A, Cheng I, Hou L, Ryu S, Boakye M. Massive spontaneous epidural hematoma in a high-level swimmer. A case report. J Bone Joint Surg Am. 2010; 92: 2843-6.
Ependymoma within the spinal canal
Subacute epidural abscess
Acute epidural hematoma
Intraspinal lipoma

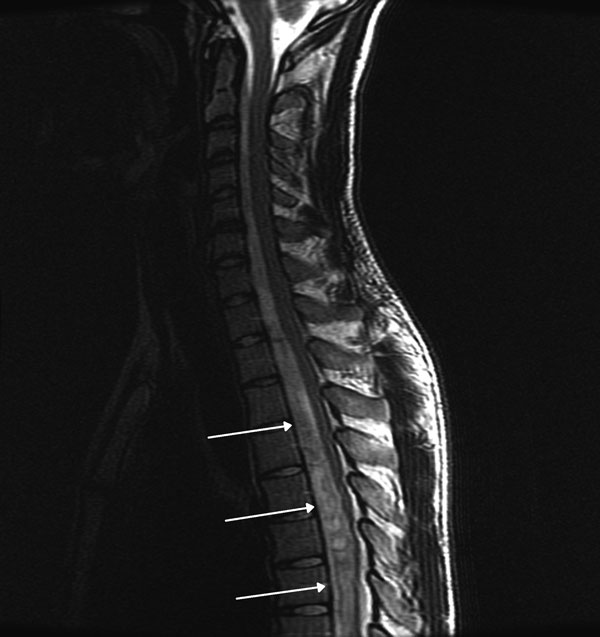
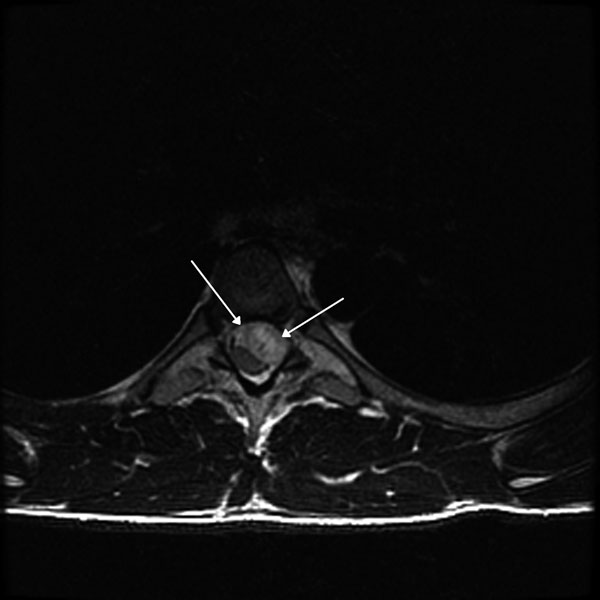
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3