A Forty-two-Year-Old Man with Neck Pain and Abnormal Upper Cervical Spine Imaging
December 18, 2013
A forty-two-year-old man with a history of smoking, intravenous drug use (heroin), and hepatitis C presented to the emergency department with nuchal pain, which became worse with cervical motion and radiated to the right side of the head. The symptoms had progressively worsened in the past two weeks after a low-energy fall (2 m high) without direct trauma to the cervical spine or skull. He had been evaluated in another hospital three months earlier for cervical pain and torticollis, and he had been given analgesic treatment, which partially relieved the symptoms. Physical examination revealed apyrexia, right torticollis with limited motion in rotation and flexion to the right, tinnitus, dysphagia, and dysarthria. He also had atrophy of the right side of the tongue and ipsilateral deviation on protrusion. The neurologic examination was otherwise normal. Upon admission, laboratory studies showed a normal white blood-cell count (WBC) and an elevated C-reactive protein level (20.7 mg/dL; normal <3 mg/dL). Blood and urine cultures were negative. The serology studies were positive only for hepatitis C; they were negative for hepatitis B, human immunodeficiency virus, brucellosis, and syphilis. The screening for tuberculosis was also negative. Radiographs of the cervical spine showed abnormal craniocervical alignment in the frontal plane, with a right-sided tilt of the head and atlantoaxial subluxation (Fig. 1). Computed tomography (CT) of the brain did not demonstrate any intracranial pathologic change. The CT scan of the cervical spine showed lytic destruction of the right atlantooccipital joint with lateral right atlantooccipital subluxation and anterior atlantoaxial subluxation (Figs. 2-A through 2-D). Magnetic resonance imaging (MRI) with gadolinium enhancement showed altered signal intensity of the clivus, occipital condyles, atlas, axis, and the surrounding soft tissues (Fig. 3). Magnetic resonance angiography identified occlusion of the right vertebral artery at the C1 level (Fig. 4). Considering the neurological deficits and the instability of the craniocervical junction, surgical treatment was proposed.
A posterior craniocervical approach was performed, followed by debridement of the region around the atlantooccipital joint. An instrumented fusion from the occiput to C5 was then performed with an occipital plate (only two occipital screws obtained purchase in the bone), pars interarticularis screws in the C2 vertebra, lateral mass screws in the C3 to C5 vertebrae, and two longitudinal rods connected by a cross-link (Fig. 5). Considering the right vertebral artery occlusion, we decided that a safer option would be to use C2 pars interarticularis screws as an alternative to C2 pedicle screws. C1-C2 transarticular screws were rejected because of the right C1 lateral mass destruction and altered C1-C2 anatomy. A corticocancellous graft obtained from the iliac crest was inserted between the occiput and the decorticated posterior arch of C1 and C2, and cancellous graft was applied around the facet joints of C2 to C5 after decortication. After surgery, the patient wore a Miami J cervical collar for twelve weeks. The microbiologic examination of the samples that had been harvested from the occipital condyle identified methicillin-sensitive Staphylococcus aureus (MSSA); antibiotherapy was initiated with intravenous flucloxacillin. On the second postoperative day, septic arthritis of the right knee was diagnosed, and the patient underwent anterior drainage. Once again, the identified agent was MSSA. After three weeks of intravenous therapy, the antibiotic treatment was changed to oral therapy for an additional four weeks. The patient was discharged from our institution after six weeks of hospitalization without any symptoms or neurological deficits other than an improving right hypoglossal nerve palsy. Laboratory studies, including C-reactive protein level, erythrocyte sedimentation rate, and WBC, were normal at discharge. On follow-up examination at three months, the patient demonstrated a full recovery with no pain or other symptoms, and the neurological examination was normal.
Proceed to Discussion >>Reference: Barbosa TR, Pereira PM, Silva PS, Monteiro PM, Vaz RM. Osteomyelitis of the atlantooccipital joint in an intravenous drug user: a case report and review of the literature. JBJS Case Connector, 2013 Oct 23;3(4):e101.
Early diagnosis of osteomyelitis of the occipitocervical junction is difficult for many reasons. This region is very rarely affected; the symptoms are subtle, variable, and nonspecific; and the neurological changes are often absent or slight and overlooked. Occipital headaches and constitutional symptoms like weight loss can be the only symptoms at presentation. Moreover, the occipitocervical junction is not easily visualized on conventional radiographs. Even open-mouth radiographs may not be conclusive because the osseous changes observed in osteomyelitis can only be identified weeks or months after the first symptoms. Early diagnosis of occipitocervical osteomyelitis is of major relevance because of important neurovascular relationships within this anatomical region and the risk of serious consequences. Our patient demonstrated some of these consequences. He originally had benign symptoms that deteriorated after a minor trauma; he presented with neurovascular deficits, namely compression of the hypoglossal nerve and occlusion of the right vertebral artery. A high level of suspicion is crucial for the diagnosis of craniocervical junction osteomyelitis and is particularly relevant in intravenous drug users, immunocompromised patients, diabetics, and people with chronic renal insufficiency. Differential diagnosis should include rheumatoid arthritis involvement and tumor pathology. CT and MRI are the main diagnostic imaging studies used to diagnose osteomyelitis of the upper cervical spine. However, CT scans only show typical signs of osteomyelitis after a long period of inflammation. Thus, MRI is the gold standard for providing early identification of tissue-density changes, definition of anatomic detail, and appreciation of the extent of neural compression, which helps to guide treatment. MRI has been shown to have a sensitivity of 96%, a specificity of 93%, and an accuracy of 94% in detecting cervical osteomyelitis. Radionuclide bone scans (gallium 67 and technetium 99m) and indium-111-tagged WBC scans may also be useful in recognizing the disease and in follow-up. Pseudomonas species is the predominant organism identified in intravenous drug users with osteomyelitis. Nevertheless, some series have reported a high prevalence of S. aureus infections in intravenous heroin users, as was the case with our patient. The most common route of bacterial spread to the cervical spine is hematogenous; the source of the S. aureus infections in our patient was probably the skin at the injection sites. Osteomyelitis of the cervical spine can also arise from an infection that spreads from adjacent tissues or contamination after invasive diagnostic or therapeutic procedures. In a review of the literature, we found six patients with occipitocervical osteomyelitis, three of whom had associated otorhinolaryngologic pathology. Nonsurgical management of occipitocervical osteomyelitis includes antibiotic therapy and external immobilization. However, in the presence of an epidural or paravertebral abscess or septicemia (despite antibiotic therapy), substantial neurological deficits, and spinal deformity or instability, surgical treatment is required. Also, if intractable pain emerges, as can occur in postinfectious arthrosis, surgical arthrodesis is indicated. Prolonged antibiotic therapy (intravenous or oral) is crucial and required in both nonsurgical and surgical management. We found six well-documented cases of pyogenic osteomyelitis of the atlantooccipital junction in the literature. Two of them were treated conservatively, and the other four underwent surgery.
Reference: Barbosa TR, Pereira PM, Silva PS, Monteiro PM, Vaz RM. Osteomyelitis of the atlantooccipital joint in an intravenous drug user: a case report and review of the literature. JBJS Case Connector, 2013 Oct 23;3(4):e101.
Osteoblastoma of C1
Metastatic lung carcinoma involving C1
Nonunion of a hangman (C1) fracture
Osteomyelitis of the atlantooccipital articulation
Hemangioma of C1

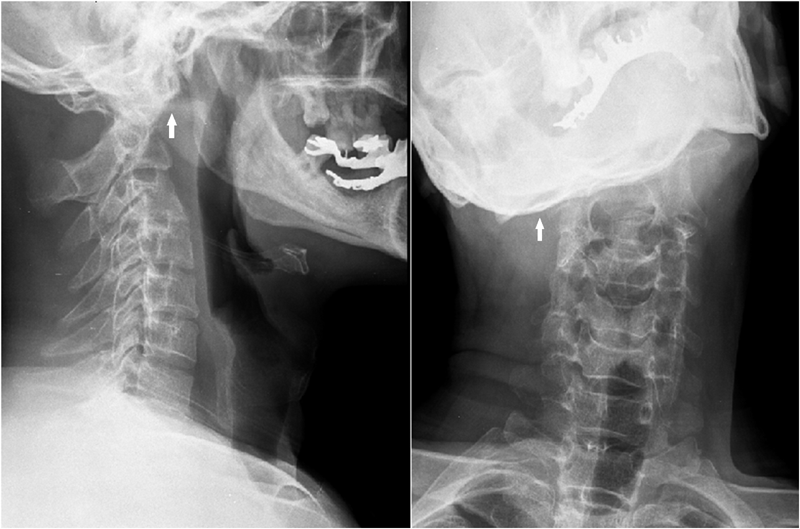
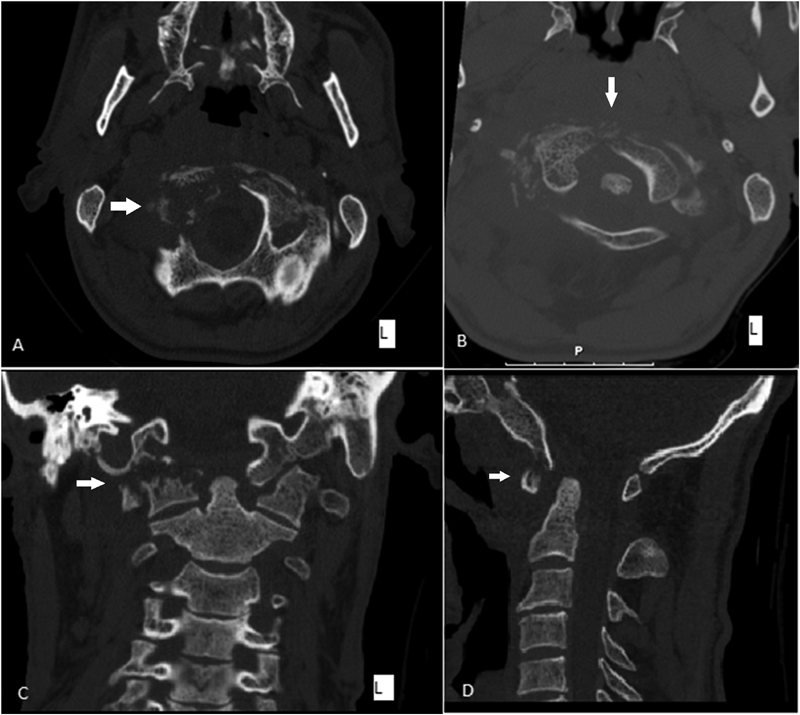

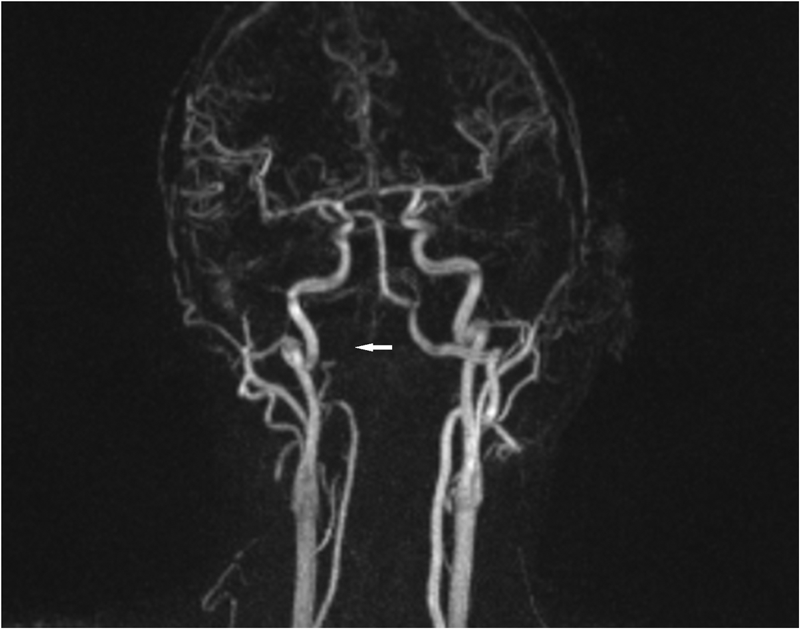
 Fig. 1
Fig. 1 Fig. 2
Fig. 2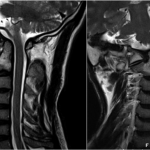 Fig. 3
Fig. 3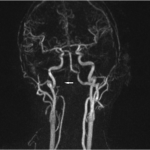 Fig. 4
Fig. 4 Fig. 5
Fig. 5