A Three-Year-Old Boy with Elbow Trauma and Abnormal Radiographic Elbow Calcification
December 4, 2013
A three-year-old boy landed on the left elbow after jumping, and he was taken to another institution’s emergency department for evaluation and treatment. He was diagnosed with an olecranon fracture, which was treated with a long arm splint. The patient continued to have pain that was exacerbated by movement and, ten days later, presented to our orthopaedic clinic. Physical examination revealed a moderate amount of swelling at the anterior aspect of the elbow. The patient had no neurologic or vascular deficit. He refused active range of motion, but the arm was passively flexed to 90° and extended to 30°, with pain on pronation and supination. Anteroposterior, lateral, and oblique radiographs of the proximal part of the left radius and ulna were obtained. The anteroposterior and oblique views showed a nondisplaced ulnar fracture and a radius that aligned well with the capitellum. However, there was a small calcification whose origin could not be definitively identified (Figs. 1-A and 1-B). Neither the initial nor the follow-up radiology reports commented on the fleck or its potential clinical significance.
Given the persistent clinical guarding, the unclear radiographic picture, and the level of skeletal maturity, the patient was taken to the operating room for additional evaluation via an arthrogram under general anesthesia. The arm was found to have internal and external rotation of only 30° in each direction. The radial head was not palpable. The arthrogram showed a completely displaced radial head with 80° of angulation (Fig. 2). Manipulation reduction under fluoroscopy was unsuccessful. Given the severe degree of angulation and several unsuccessful attempts at closed reduction, the fracture was reduced percutaneously with a Kirschner wire (Fig. 3-A) and held in place with use of the Metaizeau technique. An intramedullary pin was inserted distally to proximally, engaging and stabilizing the fracture (Fig. 3-B). Intraoperatively, the elbow range of motion was 0° to 120°, with 60° of pronation and supination. A repeat arthrogram showed a reduced radial head (Fig. 4); a long-arm soft cast was applied. The fracture healed, and the wire was removed five weeks after injury. At the six-month follow-up, full range of motion had returned.
Proceed to Discussion >>Reference: Zhu AF, Sponseller PD. An undiagnosed fracture of the radial neck in a young child: the radial neck fleck sign: a case report. JBJS Case Connector, 2013 Oct 09;3(4):e97.
Fractures of the proximal part of the radius are relatively uncommon and comprise approximately 4% to 5% of all childhood elbow fractures. One study showed that there is a higher incidence and greater variability in elbow fracture patterns in the pediatric population than in the adult population. Even though the general order of ossification is relatively predictable, the actual appearance may vary from individual to individual, making the diagnosis of fractures around the elbow in the pediatric population a unique challenge. Fracture of the radial neck in a pediatric patient younger than four years old is rare and not well described in the literature. Such fractures usually occur in children eight to twelve years of age as a result of a fall on the outstretched hand that causes impaction of the radial head against the capitellum, often coupled with valgus stress of the joint. This injury may be rare because ossification of the radial head does not begin until 4.5 years of age; therefore, some of the forces experienced by the radial neck may be dissipated. Traditional radiographic signs of a radial neck fracture include a visible fracture line involving the physis, displacement of the epiphysis, disruption of the radiocapitellar line, and a positive posterior fat pad sign. Clinicians should be aware of several other important radiographic findings: the radial neck of an infant is slightly medially angulated, mimicking a dislocation; the early proximal radial epiphysis is wedge shaped, simulating an avulsion fracture; and notches and clefts in the proximal radial metaphysis may closely resemble posttraumatic appearances. Because the radial head has radiolucent cartilage before the age of four, many of the common radiographic signs become unreliable. Nondisplaced fractures of the radial neck are the second most common fracture diagnosed on follow-up radiographs when an isolated posterior fat pad elevation is seen on an initial radiograph. Other methods of identifying radial neck fractures are needed to guide diagnosis in younger patients. Therefore, we would like to stress the importance of the radial neck fleck sign, which is a small portion of ossified radial head that may be visualized on radiographs and represents a radial neck fracture that is translated or angulated. The fleck represents only a small portion of the radial metaphysis, but its displacement signals the amount of translation of the unseen radial head in patients who have not begun secondary ossification of the radial head. On an anteroposterior radiograph of the elbow, a small radiopacity at the level of, or right below, the radial neck may be visible, which may represent a laterally and distally displaced radial head. This subtle ossified fragment may signal displacement of a larger segment. If the radial neck fleck sign is present or physical examination is concerning, an arthrogram or magnetic resonance image is recommended to elucidate the exact injury. Arthrography, rather than magnetic resonance imaging, was our preference because it allowed treatment at the same time. Early diagnosis and treatment is necessary to allow reduction. The most common complications involve loss of pronation and supination. Our patient, a three-year-old child, had an undiagnosed completely displaced radial neck fracture with an associated nondisplaced olecranon fracture. We believe that the radial neck fleck sign is a diagnostic aid with radial neck fractures in pediatric patients who have no secondary ossification of the radial head.
Reference: Zhu AF, Sponseller PD. An undiagnosed fracture of the radial neck in a young child: the radial neck fleck sign: a case report. JBJS Case Connector, 2013 Oct 09;3(4):e97.
Heterotopic ossification
Completely displaced radial neck fracture
Radial collateral ligament avulsion fragment
Septic arthritis

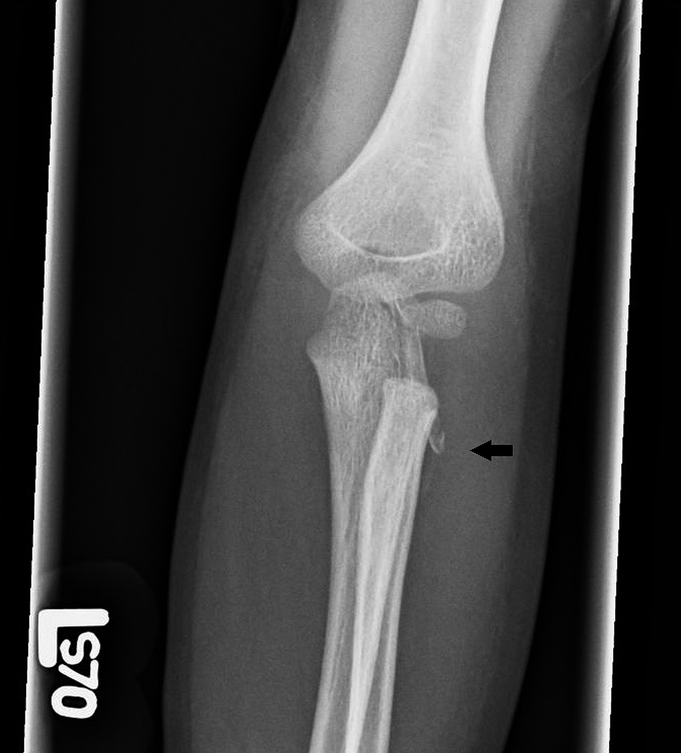

 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 2
Fig. 2 Fig. 3-A
Fig. 3-A Fig. 3-B
Fig. 3-B Fig. 4
Fig. 4


