A Fourteen-Year-Old Girl with Pain, Numbness, and Tingling in the Left Hand
March 18, 2015
A fourteen-year-old girl was referred to our clinic with ulnar-sided wrist pain, numbness, and tingling of the left hand. She reportedly had been having these symptoms for two years since a rollover accident with a go-cart. The records indicated that she had sustained an open left elbow dislocation and immediately had been taken to the operating room for irrigation and debridement. It was noted that there was brachial artery disruption even though she had palpable peripheral pulses and capillary refill of less than three seconds prior to surgery. The artery subsequently had been repaired. Postoperatively, motor function and sensory function were intact in the radial, ulnar, and median nerve distributions with palpable radial pulses bilaterally. The patient had been transferred from the outside hospital to our pediatric orthopaedic surgery unit on postoperative day one for additional monitoring, wound care, and rehabilitation. She subsequently had required a second irrigation and debridement, split-thickness skin-grafting, and rotational flap coverage to the antecubital fossa. For two years after the reconstructive surgery, she continued to experience the stated symptoms on an ongoing basis, with increasing severity within the last three months. These symptoms included ulnar-sided wrist pain, cold intolerance, numbness, and tingling along the ulnar border of the left hand. She stated that the pain was relieved when she extended the elbow and was aggravated with certain activities such as writing. On examination, she did not have point tenderness over the extensor carpi ulnaris tendon sheath, the fovea, or the distal radioulnar joint. A distal radioulnar joint stress test revealed equal laxity bilaterally without pain. The Tinel sign was positive at both Guyon’s canal and the cubital tunnel. The Allen test was equal and negative bilaterally. The left hand, however, was cooler to the touch than the right hand. She had full active range of motion of the elbow, the forearm, the wrist, and the digits. Sensation to light touch was normal in the median, ulnar, and radial nerve distributions. Magnetic resonance imaging of the left wrist with contrast injection, which had been performed at an outside institution, demonstrated a triangular fibrocartilage complex injury. We ordered an electromyography (EMG) and an arterial Doppler ultrasound examination to further investigate the etiology of the symptoms. The EMG revealed mild median and ulnar nerve mononeuropathies at the wrist and the elbow. The arterial Doppler examination did not detect brachial, radial, or ulnar artery pressures. Digital pressures were also absent, but waveforms were within normal limits. An angiogram was then obtained (Fig. 1).
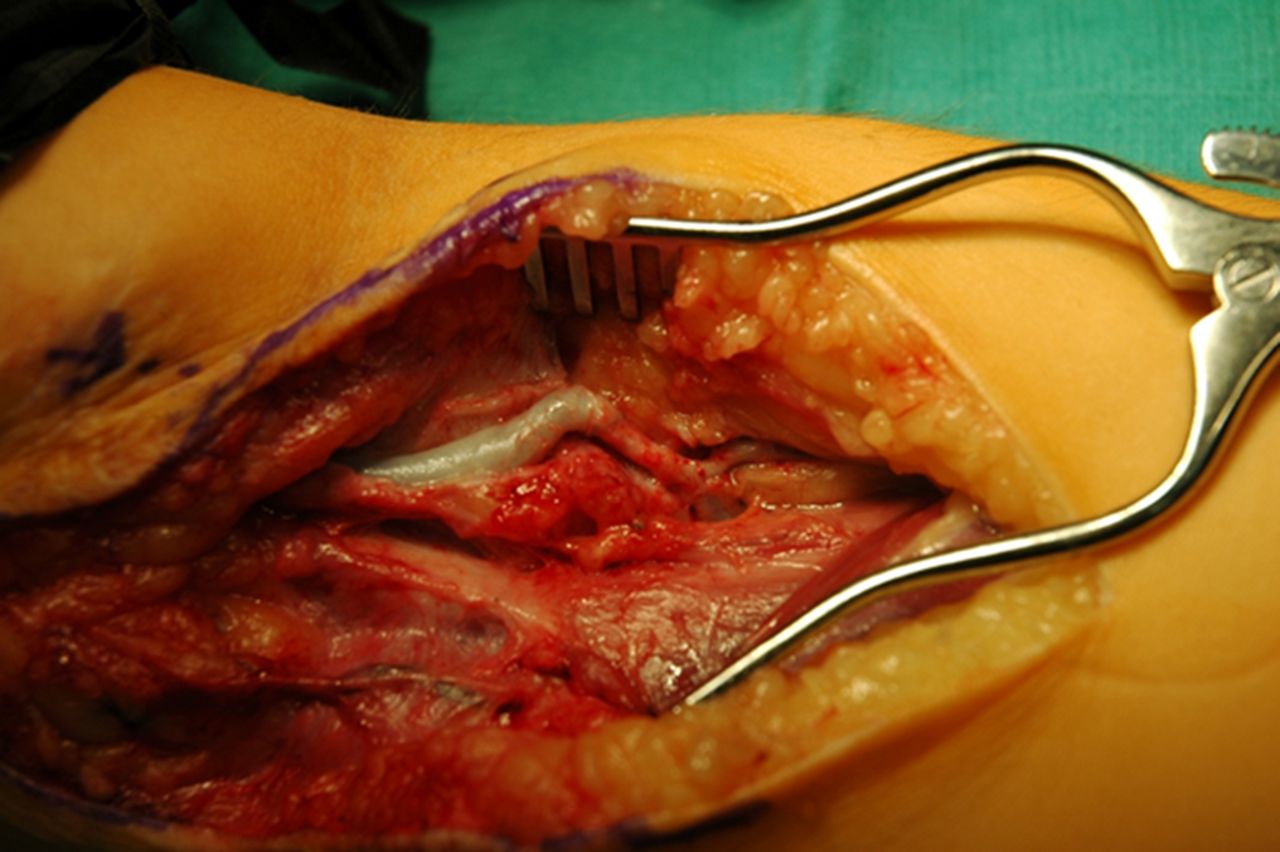
The angiogram demonstrated a widely patent basilic vein bypass graft with no evidence of thrombosis. After sharing the contradictory Doppler and angiogram results with the family, a decision was made to proceed with exploration and nerve releases. Intraoperatively, it was discovered that the brachial artery remained patent in extension, but occluded in flexion secondary to kinking of the graft (Fig. 2). Graft measurements were performed with the elbow in flexion, and 3 cm of excess graft were excised, with the ends repaired primarily. We also released the ulnar nerve in situ at the elbow and performed a carpal tunnel release at the wrist. A long arm splint was placed with the elbow in 90° of flexion. Postoperatively, the radial pulse was noted to be substantially stronger than prior to surgery. At the two-week follow-up, the patient stated that the sensitivity to cold and the pain in the forearm had improved, but she still experienced residual numbness and tingling in the ring and little fingers. Examination revealed a 2+ radial pulse and slightly decreased sensation in the ulnar nerve distribution. At the two-month follow-up, she reported complete resolution of the symptoms, including the cold intolerance.
Proceed to Discussion >>Reference: Zhu AF, Seeley MA, Ozer K. Positional occlusion of an interposition vein graft for brachial artery reconstruction following open elbow dislocation in a pediatric patient. A case report. JBJS Case Connect. 2015 Jan 14;5(1):e3.
Our patient presented with cold intolerance and a cooler hand on the affected side. Preoperative arterial Doppler examination and an angiogram demonstrated contradictory results regarding the patency of the brachial artery. Intraoperative examination revealed positional kinking of the basilic graft, which explained the contradictory vascular test results. This case report highlights the importance of checking for appropriate graft length following vascular repairs. Because of their thin walls, vein grafts can easily be occluded in flexion, resulting in vascular insufficiency in the extremity. The discrepancy in test results can be attributed to the differences in extremity positioning with the Doppler examination and the angiogram. The proper technique to measure an ankle-brachial index, as recommended by the American Heart Association, is to have the patient in a supine position so as not to falsely elevate ankle pressure. However, studies have shown that brachial artery pressures do not vary substantially between the seated and supine positions. Thus, upper-extremity pressure measurements are typically performed in the seated position with the forearm placed on a table, resulting in variable degrees of flexion at the elbow. In our patient, this flexion likely produced occlusion in the graft, accounting for the abnormal Doppler results. Angiography is typically performed with the patient supine with the upper extremity in full extension, which allowed for stretching and unobstructed flow through the graft in our patient. Positional disruption of arterial flow is a phenomenon that is well described in the vascular surgery literature in regards to the vertebral artery and the internal carotid artery. Bow-hunter’s syndrome is a well-documented condition in which mechanical occlusion of the vertebral artery occurs at the atlantoaxial level during head rotation, resulting in symptomatic vertebrobasilar insufficiency. It is also well known that elongation and kinking of the internal carotid artery is a common variant of the anatomy that can, in rare instances, become symptomatic. Few reports exist in the orthopaedic literature regarding positional disruption of arterial flow in relation to orthopaedic injuries and its treatments. In rare cases, repetitive compression of the axillary artery in overhand-throwing athletes has led to focal arterial pathology; however, to our knowledge, there has been no description of complete occlusion of arterial flow based on extremity positioning after an orthopaedic injury. Open elbow dislocations are rare injuries that occasionally are associated with vascular complications. Currently, we are not aware of any specific treatment guidelines for elbow dislocations with concomitant arterial injury. Arterial compromise in the setting of a perfused supracondylar humeral fracture is a more common injury that has received increasing attention regarding treatment. Reports of early vascular exploration in this setting have demonstrated mixed results, with asymptomatic vessel reocclusion rates from as low as 9% to as high as 25%. There is abundant literature regarding management of arterial injuries in supracondylar fractures; we were able to use this information to help guide the management of our patient. She initially had presented with an open elbow dislocation and the incidental discovery of a transected brachial artery. Because the injury had been visualized during the standard washout for an open injury, repair of the artery had been indicated, even in the setting of a palpable distal pulse with a well-perfused limb. Two years later, when the patient remained symptomatic, a nerve exploration was performed with excision and repair of the graft. The repair was uneventful, and the patient did well, with improvement of motor and sensory deficits over the next two months.
Reference: Zhu AF, Seeley MA, Ozer K. Positional occlusion of an interposition vein graft for brachial artery reconstruction following open elbow dislocation in a pediatric patient. A case report. JBJS Case Connect. 2015 Jan 14;5(1):e3.
Brachial artery aneurysm
Arteriovenous malformation, brachial artery to cephalic vein
Patent basilic vein graft
Brachial artery false aneurysm


 Fig. 1
Fig. 1 Fig. 2
Fig. 2