A fifteen-year-old gymnast with a medical history noteworthy for hypothyroidism secondary to Hashimoto thyroiditis presented to her primary care provider with a two-month history of right-sided foot pain. The pain was localized to the medial side of the first metatarsophalangeal (MTP) joint. She denied any specific trauma or injury to the foot, but did state that the pain worsened during high-energy tumbling activities. Radiographs obtained by the primary care provider demonstrated a well-corticated osseous fragment medial to the head of the first metatarsal (Figs. 1-A and 1-B). These images were compared with radiographs obtained one year prior for unrelated symptoms (Figs. 2-A and 2-B), and they demonstrated a slight increase in the size of the fragment. With concern for a possible stress fracture of the first metatarsal, the primary care provider referred the patient to a pediatric orthopaedic specialist for evaluation. On physical examination at the time of presentation, the patient had full active range of motion of the first MTP joint and no cutaneous sign of injury. She noted tenderness to palpation about the right medial MTP prominence, and an osseous excrescence was palpable but not mobile. There was no tenderness about the plantar plate or the sesamoids. Magnetic resonance imaging (MRI) confirmed the location of the osseous fragment, as well as a possible site of origin at the medial aspect of the distal part of the first metatarsal (Figs. 3-A through 3-D).
An initial trial of nonoperative management, including both activity and shoe modification, provided no relief. The patient and her parents decided on surgical removal of the suspected fragment. Intraoperatively, a 1-cm incision was made medial to the first MTP joint, and dissection was carried down to the joint capsule. The fragment was palpable deep to the capsule. An arthrotomy was performed; exposure of the presumed fragment revealed chalklike material that was easily friable, seemed to emanate from the capsule, and did not appear to be a fragment of bone. An intraoperative photograph of the mass is shown in Figure 4. The tophaceous material was sent for pathologic evaluation, and the joint was thoroughly irrigated with sterile normal saline solution. Pathologic evaluation confirmed dense fibrous tissue with calcification, consistent with a diagnosis of calcific tendinopathy. The patient recovered well and had returned to gymnastics by six months postoperatively.
Proceed to Discussion >>Reference: Berge M, Wagner S, Jex J. Calcific tendinopathy of the abductor hallucis tendon in an adolescent gymnast: a case report. JBJS Case Connect. 2015 Jan 28; 5(1):e9.
Calcific tendinopathy is rare in pediatric patients; few cases are reported in the literature, and most occur in the hand or shoulder. Most commonly, calcific tendinopathy results secondary to penetrating trauma or chronic, repetitive blunt trauma. Development of trigger finger in pediatric patients secondary to idiopathic calcific tendinopathy has been reported. In our patient, there was no history of penetrating trauma or any other predisposing injury to the foot. She was an active gymnast who denied any specific traumatic events. However, she did have a history of thyroid disease, which is a known risk factor for calcific tendinopathy, although most research has focused on its incidence in the shoulder. Hypothyroidism, particularly forms associated with autoimmune diseases such as Hashimoto thyroiditis, is associated with both an increased prevalence of calcific tendinopathy and an earlier onset of disease. The calcific deposit that was debrided from the abductor hallucis tendon was found intraoperatively to have a chalklike consistency, which is in accordance with the formative phase during the early calcific stage of calcific tendinopathy. Previous research has suggested that this phase is often the first point in the progression of calcific tendinopathy when patients are likely to become symptomatic. Drawing from the current paradigms for treatment of calcific tendinopathy of the rotator cuff, surgical intervention is indicated in patients who have progression of symptoms or symptoms that interfere with activities of daily living, or in those with unsuccessful conservative management. There are very little outcomes data in the literature regarding surgical treatment of calcific tendinopathy in pediatric patients, but several case reports have demonstrated good results in appropriately selected patients. In adult patients, therapeutic benefits to surgical management of calcific tendinopathy affecting the rotator cuff have been shown at one year; however, data at five and ten years’ follow-up do not clearly show improved outcomes, suggesting that surgical treatment may not ultimately affect the clinical course of the disease. This case report is unique insofar as it highlights calcific tendinopathy as a pathologic process that should be considered in pediatric patients. Pain with activity, tenderness, localized edema, or decreased range of motion, in conjunction with radiographic confirmation of a calcific abnormality, should warrant additional investigation. As in this case, refractory patients may benefit from surgical treatment. This report demonstrates that even in unlikely anatomic locations, calcific tendinopathy may occur and must remain on the differential diagnosis for pediatric patients with the appropriate clinical picture.
Reference: Berge M, Wagner S, Jex J. Calcific tendinopathy of the abductor hallucis tendon in an adolescent gymnast: a case report. JBJS Case Connect. 2015 Jan 28; 5(1):e9.
Avulsion fracture from the first metatarsal head
Calcific tendinopathy of the abductor hallucis tendon insertion
Tophaceous gout
Sesamoiditis
Periosteal chondroma





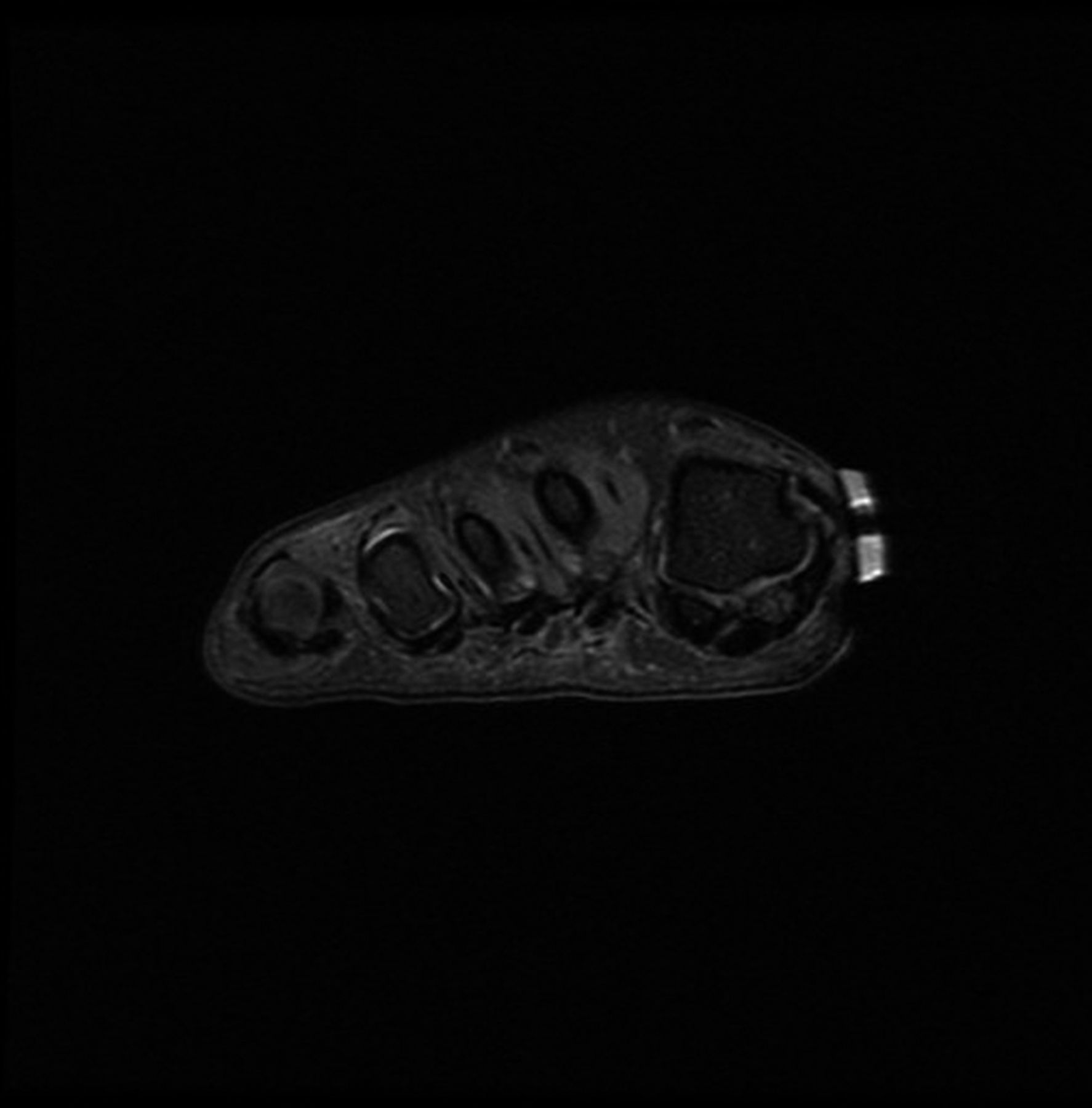



 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B Fig. 3-A
Fig. 3-A Fig. 3-B
Fig. 3-B Fig. 3-C
Fig. 3-C Fig. 3-D
Fig. 3-D Fig. 4
Fig. 4