A Painful Mass in the Region of the Tibial Tubercle in a Thirty-one-Year-Old Man
January 6, 2010
A thirty-one-year-old man presented to the orthopaedic department because of pain and swelling in the right knee one month after he had been involved in a bicycle accident in which the right knee had been forced into hyperextension. The patient had sought treatment at another hospital and the right lower limb had been immobilized with a below-the-knee cast for one month, but the symptoms remained after the cast was removed. Physical examination revealed swelling of the right knee and a mild joint effusion. Multiple firm masses were palpable over the anterior aspect of the proximal part of the tibia and the patellar tendon. The masses were ill-defined, hard, and rough-surfaced, and some of them were mobile. There was no local warmth, and the overlying skin was normal. The active range of motion of the right knee was slightly limited with 10° of extension and 125° of flexion. Muscle atrophy was observed in the right thigh. Laboratory tests indicated no abnormalities. The patient reported that he had had mild discomfort in the affected knee for approximately one year before the bicycle accident. Approximately fifteen years previously, the patient had belonged to a baseball club and had experienced right anterior knee pain. Although he had consulted a physician and had been diagnosed with Osgood-Schlatter disease, he had not received any medical treatment at that time. After the diagnosis, he had intermittent knee pain but the symptoms resolved before the patient reached the age of twenty years. Radiographs of the right knee revealed an osseous mass that was attached to the tibial tubercle. The mass extended to the inferior aspect of the patella and was surrounded by several loose osseous fragments (Fig. 1). Computed tomography scans of the knee confirmed an osseous stalk originating from the tibial tubercle (Fig. 2). A swollen infrapatellar bursa containing multiple loose bodies was noted at the anterior aspect of the osseous stalk. Computed tomography scans that were made after air arthrography showed no communication between the bursa and the knee joint. T2-weighted magnetic resonance images revealed fluid and multiple hypointense nodules in the infrapatellar bursa (Fig. 3).
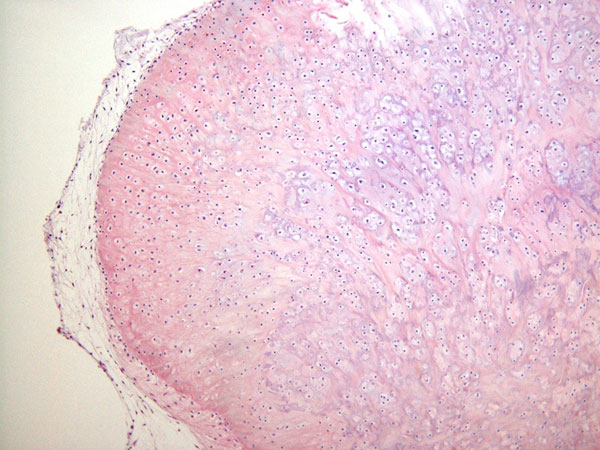
At the time of surgery, the infrapatellar bursa and the osseous stalk of the tibial tubercle were totally excised. The patellar tendon had been thinned and stretched by the swollen bursa. The osseous stalk was densely adherent to the patellar tendon and originated from the tibial tubercle. A total of twenty-six loose bodies were detected within the excised bursa. There was no communication between the bursa and the knee joint cavity. Histologically, the infrapatellar bursa was lined with synovial lining cells and edematous changes were observed in the sublining areas. Several metaplastic chondroid islands were observed beneath the synovial membranes. The chondrocytes were hypercellular but were devoid of nuclear atypia, and some ossification foci were seen in the matrix (Fig. 4). The loose bodies were composed of mature trabecular bone, with fatty bone marrow at the center of the lesions and benign hyaline cartilage with varying degrees of endochondral ossification at the periphery. Dense collagen fibers from the patellar tendon were attached to the surface of the osseous stalk. The radiographic and histologic findings suggested infrapatellar bursal osteochondromatosis associated with a large, unresolved Osgood-Schlatter lesion. The symptoms completely resolved three weeks after surgery. At the time of the most recent follow-up examination, three years after surgery, the patient remained free of symptoms and there was no evidence of local recurrence of the lesion as confirmed by computed tomography and magnetic resonance imaging studies.
Proceed to Discussion >>Reference: Ishida K, Kuroda R, Sato K, Iguchi T, Doita M, Kurosaka M, Yamamoto T. Infrapatellar bursal osteochondromatosis associated with unresolved Osgood-Schlatter disease. A case report. J Bone Joint Surg Am. 2005;87:2780-3.
Synovial osteochondromatosis can develop in any space that is lined with synovium. It commonly involves large joints such as the knee and shoulder. Intrabursal osteochondromatosis is exceptionally uncommon. There have been a few reported cases of bursal osteochondromatosis involving the retrocalcaneal, subacromial, and subcoracoid bursae; however, it does not appear that infrapatellar bursal osteochondromatosis has ever been reported in the English-language literature. In addition, the present case is unique in that the lesions developed in association with a large, unresolved Osgood-Schlatter lesion. Synovial and bursal osteochondromatoses are known to arise following minor or major trauma, and in this case the bursal osteochondromatosis seems to have been caused by chronic, repetitive minor trauma due to the osseous stalk of the old Osgood-Schlatter lesion. In the case of this patient, histologic studies of the excised bursa revealed osteochondral metaplastic changes in the sublining areas and the lesion was classified as a stage-2 lesion according to the system of Milgram. Similarly, it has been reported that a reactive bursa can form over an osteochondroma as a result of friction between the osteochondroma and the overlying soft tissues. Some previous investigators have reported the development of osteochondromatosis in the bursa over an osteochondroma. The etiology of such lesions is considered to be similar to that of the lesion in this patient. It is now generally agreed that Osgood-Schlatter disease is caused by an avulsion fracture of the growing tibial tubercle. The vast majority of Osgood-Schlatter lesions respond to nonoperative treatment that is aimed at decreasing the stress on the tibial tubercle and reducing the tension in the extensor mechanism. The natural course of Osgood-Schlatter disease is that the symptoms resolve with closure of the proximal tibial growth plate. However, patients in whom an ossicle forms deep to the patellar tendon might continue to have mild knee pain. Bursal chondromatosis should be considered in the differential diagnosis of chronic knee pain in adult patients with an unresolved Osgood-Schlatter lesion, although the phenomenon is extremely uncommon.
Reference: Ishida K, Kuroda R, Sato K, Iguchi T, Doita M, Kurosaka M, Yamamoto T. Infrapatellar bursal osteochondromatosis associated with unresolved Osgood-Schlatter disease. A case report. J Bone Joint Surg Am. 2005;87:2780-3.
Calcific bursitis of infrapatellar bursa
Tophaceous gouty deposits in infrapatellar bursa
Infrapatellar bursal osteochondromatosis




 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4