Trochanteric Bursitis Refractory to Treatment in a Forty-two-Year-Old Woman
February 3, 2010
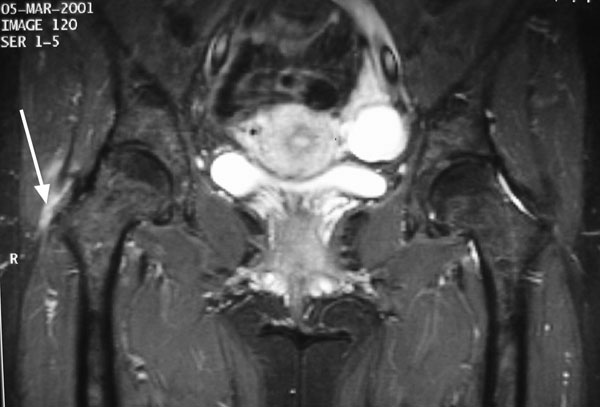
A forty-two-year-old woman presented with a seven-month history of atraumatic, moderate-to-severe debilitating pain in the lateral aspect of the right hip. In the months preceding presentation, the condition had been treated as trochanteric bursitis by her primary care physician. Treatment had included nonsteroidal anti-inflammatory drugs, several cortisone injections, and physical therapy. After failure of nonoperative treatment, narcotics were prescribed for pain control and the patient was referred to an orthopaedic specialist for evaluation. On evaluation, the patient had no history of any medical problems nor did she have any predisposing conditions that would cause tendon rupture. She also had no history of related trauma, lumbar spine disease, or contralateral hip pain. Her lifestyle was moderately active. On examination, the patient weighed 68 kg and was 173 cm tall. She had normal spine movement, no pelvic tilt, and no limb-length discrepancy. She had an antalgic gait and a positive Trendelenburg sign. There was mild tenderness over the right subcutaneous trochanteric bursa and severe tenderness over the insertion of the gluteus medius and minimus tendons. No palpable lesions were noted. There was full, symmetric range of motion of both hips and no groin pain with provocative maneuvers. There was weakness and trochanteric pain with resisted hip abduction and flexion as well as mild tightness but no snapping of the iliotibial band. Straight-leg-raising was unrestricted and pain free, and the deep tendon reflexes were normal. Plain radiographs did not demonstrate bone avulsion or calcification adjacent to the greater trochanter or within the substance of the gluteal tendons. There was no sclerosis of the greater trochanter or degenerative disease of the hip. To rule out any abnormality related to the greater trochanter, magnetic resonance images of the pelvis were acquired, including a coronal T1-weighted image, a coronal short tau inversion recovery image, an axial T1-weighted image, a sagittal T2-weighted fast-spin-echo image with fat saturation (Fig. 1), and small-field-of-view coronal proton-density-weighted images with fat saturation.
Surgical reattachment was offered to the patient because of the severe debilitating symptoms and failed nonoperative treatment, and the patient agreed. A longitudinal incision was made over the right hip, and the tensor fasciae latae was incised in line with its fibers. The subcutaneous trochanteric bursa was noted to be normal. The anterior portion of the gluteus medius tendon was noted to be partially avulsed from the greater trochanter, and the tendon was released anteriorly to expose the gluteus minimus tendon. The majority of the gluteus minimus was found to be avulsed. Several sutures were placed in the free end of this tendon, and it was repaired back to the greater trochanter through drill holes. The repair was augmented with use of an orthobiologic patch (Restore Orthobiologic Soft Tissue Implant; DePuy OrthoTech, Warsaw, Indiana). The patch was unwrapped, reconstituted, cut to fit the repaired area, and then sutured under slight tension to the gluteus minimus and the trochanteric remnant with 2-0 Vicryl sutures (polyglactin; Ethicon, Somerville, New Jersey). The anterior portion of the gluteus medius tendon was then advanced and repaired back to the cuff of tendon, which had remained attached to the greater trochanter. Sutures were also used to secure the repair of the gluteus medius tendon to the greater trochanter. The wound was closed in layers. The patient was discharged home on the next day and had no postoperative complications. After two weeks of protected weight-bearing with use of two crutches, she was started on resistance-free abduction exercises and graduated to one crutch. At five weeks, the pain and limp were gone and she had full return of abduction and flexion strength. By four months after the operation, she was symptom-free and able to walk 3 km without difficulty. Five years later, she presented with a four-month history of spontaneous progressive lateral pain and weakness of the left hip and no history of trauma. The physical examination was similar to that at the time of her previous presentation except that the limp and Trendelenburg sign were not as pronounced. As before, magnetic resonance imaging revealed a rupture of the gluteus minimus tendon and possible tear of the gluteus medius tendon. The right hip was normal. Because of her history, nonoperative as well as surgical treatment was offered to the patient, and she opted for surgical treatment. Surgical repair was performed with use of the same technique as in the first operation. Six months after surgery, the patient was walking without pain, crutches, or a limp.
Proceed to Discussion >>Reference: Fisher DA, Almand JD, Watts MR. Operative repair of bilateral spontaneous gluteus medius and minimus tendon ruptures. A case report. J Bone Joint Surg Am. 2007;89:1103-7.
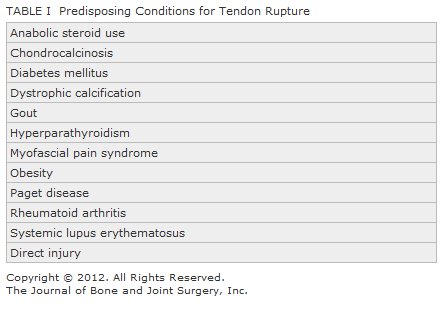
Although rupture of the gluteus tendons is considered to be an uncommon injury, unilateral ruptures have been reported recently in both the orthopaedic and radiographic literature. However, the literature to date does not describe spontaneous bilateral ruptures or a description of surgical repair. The characteristic findings of gluteus medius and minimus ruptures are similar to those of trochanteric bursitis and may lead to the wrong diagnosis. This may result in prolonged treatment with nonsteroidal anti-inflammatory drugs, cortisone injections, and physical therapy, leading to improvement in some patients but lingering symptoms with intractable pain and hip weakness in most. Patients usually present with chronic lateral pain in the hip, often associated with a disabling limp and no history of trauma. They may describe a grinding sensation and have difficulty climbing stairs. On examination, there often will be exquisite tenderness over the insertion of the gluteus medius tendon and occasionally over the trochanteric bursa. The two most reliable clinical signs are the Trendelenburg sign and pain on resisted hip abduction, both of which are reported to have greater than 70% specificity and sensitivity for diagnosing this condition. Pain on resisted hip internal rotation is a helpful sign but is not as reliable. Conditions such as fibromyalgia, mechanical low back pain, lumbar spinal stenosis, lumbar radiculopathy and femoral nerve irritation, stress fracture, and osteonecrosis may mimic this condition and should be considered in the differential diagnosis. A variety of systemic conditions (Table I) may predispose to degenerative changes in the tendon, and these changes may lead to eventual rupture of the tendon. It has been postulated that pelvic morphology, a high valgus angle of the knee, and leg-length discrepancy predispose patients biomechanically to injury as the greater trochanter impinges on a tight iliotibial band. Tension within the iliotibial band may result in frictional trauma to the gluteal tendons, just as the acromial process causes trauma to the rotator cuff in the shoulder. An alteration in gait is likely a predisposing factor and may play a role in causation as well. The clinical diagnosis of gluteus medius or minimus tendon rupture alone is often difficult. Plain radiographs are usually not helpful but may show calcification within the gluteal tendons or a bone avulsion. Tendinous calcification has been reported in up to 40% of patients diagnosed with greater trochanteric bursitis; however, other studies have found radiographic signs to be less common. For example, Schapira et al. found positive signs in only nine of seventy-two patients. Scintigraphic findings typically consist of nonspecific uptake at the lateral aspect of the greater trochanter. However, some researchers have suggested that bone scan findings may indicate gluteal tendinitis and not bursitis because of the characteristic appearance of a short linear band of increased uptake confined to the superior and lateral aspects of the greater trochanter on early blood-pool or delayed images. Tendinitis, tears, and ruptures of the gluteal tendons are most accurately diagnosed by magnetic resonance imaging, with coronal T1-weighted images with fat saturation and axial fast-spin-echo T2-weighted images. These techniques may reveal calcification within the tendons and edema within the muscle and adjacent compartments. Ultrasound can also be a useful aid in detecting gluteal injuries. The overall prevalence of disruptions of the gluteus medius and minimus tendons is unknown, as is the prevalence of clinically important symptoms. Howell et al. found degenerative tears of the gluteus medius or minimus in 20% of 176 patients undergoing total hip arthroplasty, and Bunker et al. reported a 22% prevalence of tears in a prospective study of fifty consecutive patients with femoral neck fractures. The percentage of symptomatic patients in these two studies was not known. Gluteus tendon ruptures, if diagnosed early, can be treated nonoperatively by unloading the involved hip with crutches or a cane, prescribing nonsteroidal anti-inflammatory drugs, and having the patient undergo physical therapy once the acute symptoms have subsided. Local corticosteroid injections are often used, but their effect on the tendinopathy is not clear. Surgical management may be necessary if the patient fails to respond to nonoperative treatment. Operative treatment should include conjoined tendon débridement, transosseous fixation, and possibly augmentation with soft-tissue graft material. The latter could include autograft, allograft, or xenograft. In conclusion, gluteus medius and minimus tears are often misdiagnosed or underrecognized and may be more common than previously appreciated. Disruption of the gluteus medius and minimus should be included in the differential diagnosis of patients who present with acute or chronic hip pain.
Reference: Fisher DA, Almand JD, Watts MR. Operative repair of bilateral spontaneous gluteus medius and minimus tendon ruptures. A case report. J Bone Joint Surg Am. 2007;89:1103-7.
Stress fracture of the greater trochanter
Tendonitis of vastus lateralis origin
Gluteus medius and minimus tendon rupture
calcific bursitis over greater trochanter

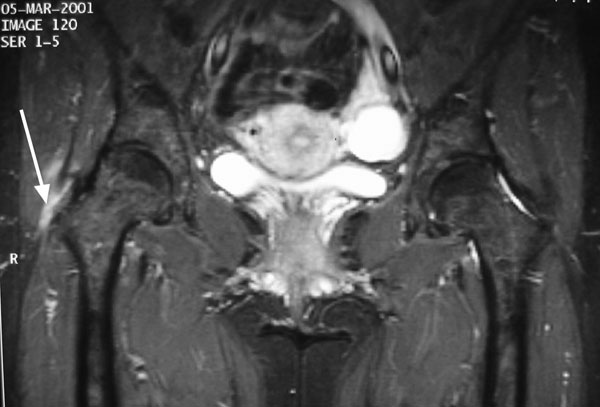
 Fig. 1
Fig. 1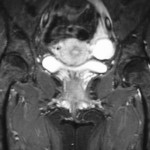 Fig. 1
Fig. 1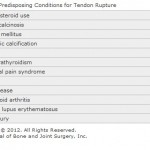 Table 1
Table 1