A Seventy-four-Year-Old Woman with Right Midfoot and Hindfoot Pain
November 20, 2013
A seventy-four-year-old woman was admitted to the hospital in December 2011 with right midfoot and hindfoot pain. Clinical and radiographic evaluation showed midfoot arthritis and chronic tendinopathy of the Achilles tendon. The local vascular and neurological status did not raise clinical concerns. Medical history included several miscarriages, use of oral anticoagulation for repetitive thrombosis for thirty years, and severe wound complication following cholecystectomy twenty years prior. Preoperative blood test results, including leukocyte count and C-reactive protein (CRP) level, were normal. On December 9, the patient underwent complex right midfoot fusion and ipsilateral Achilles tendon reconstruction. On December 11, the foot was moderately painful with severe swelling. Blood tests showed leukocytosis (11.2 × 109/L) and an increased CRP level (15.8 mg/dL). Her temperature was 37.9°C. Because of ongoing swelling, reddening of the foot, and persistent high signs of inflammation in the blood, the diagnosis of infection was considered. On December 15, the first debridement was performed. Empiric antibiotic therapy (cefuroxime, 1.5 g three times daily) was started after the biopsy. However, the postoperative lesion spread progressively and rapidly in a centrifugal manner, with a purulent base limited by an active and detaching reddish-purple edge. Repeat debridements with installation of a vacuum-assisted closure device (V.A.C. Therapy; KCI, Wiesbaden, Germany) were performed on December 23, December 27 (Fig. 1), January 2, 2012 (Fig. 2), and January 6. The ulcerations became deeper, and the skin borders consistently became necrotic after each debridement. Subcutaneous and fascial sutures failed, and the extensor tendons, metatarsal bones, and Achilles tendon were exposed. The implants were removed and the Achilles tendon was resected. The ulcerations with undermined borders were surrounded by erythema with a well-defined border and a violaceous and reddish color. The biopsies of the ulcerated lesion showed an unspecific leukocyte infiltration, consistent with an inflammatory process (Fig. 3). Because all repeat superficial and deep bacteriologic cultures were negative, an infection was never confirmed. Angiography of the extremity showed no relevant circulatory disorder (Fig. 4). The immunology and hematology tests were normal, including tests for thrombophilia and antiphospholipid syndrome. On January 12, the patient was referred to the plastic surgery department for a latissimus dorsi myocutaneous flap transfer. During this surgical procedure, the first metatarsal was resected. Ulcerated lesions occurred at the donor site (Fig. 5) and abdomen after injection of subcutaneous low-molecular-weight heparin. Despite good viability of the graft, an infection occurred with Staphylococcus epidermidis and Enterobacter aerogenes; the infection was treated with antibiotics.
Given the previous negative bacteriologic tests, the suspicious findings of the initial wounds, and the ulcerations on the abdomen and the graft donor site, the diagnosis of pyoderma gangrenosum (PG) was made. The treatment algorithm was determined with our immunologic department. Despite infection of the graft, the administration of prednisolone (100 mg per day) was initiated under antibiotic (clindamycin, ciprofloxacin) cover to prevent the spread of infection; within two days, lesion progression had been halted. A below-the-knee amputation was performed because of the lack of options for reconstruction of the affected foot. The amputation wound also showed signs of inflammation; therefore, an additional 100 g of polyclonal immunoglobulin was administered over a five-day period (20 g per day). Because of the dramatic clinical improvement, the prednisolone (100 mg per day) dose was sequentially reduced according to the CRP level and wound-healing condition. The amputation wound and the ulceration on the abdomen eventually healed. The wound of the donor site was treated successfully with skin-grafting under immunosuppressive treatment. The patient was discharged on a reducing course of oral prednisolone. At the one-year postoperative follow-up, the patient was able to walk with a prosthesis, and there was no recurrence of wound complications from PG in the follow-up period.
Proceed to Discussion >>Reference: Fang Z, Waizy H, Berger S, Stukenborg-Colsman C, Plaass C. Pyoderma gangrenosum following orthopaedic surgery: a case report and literature review. JBJS Case Connector. 2013 Aug 28;3(3):e84.
Symptom aggravation after correct antibiotic therapy and/or debridement is the principal warning sign for PG. The clinical appearance of the characteristic ulcerations surrounded by undermined violaceous edges is the cornerstone of diagnosis. Orthopaedic surgeons consider several conditions in the differential diagnosis of PG, including early lesions that spread despite antibiotic therapy; severe inflammatory syndrome with negative bacteriologic findings; and associated systemic disorders, including familial history of hematologic, immunologic, rheumatologic, and neoplastic pathology. In 50% to 70% of patients with PG, there is an underlying immunologic, inflammatory, or neoplastic systemic disorder. Review of the literature supports this association. When the suspected diagnosis has been made, rapid implementation of corticosteroid therapy is the decisive diagnostic test; corticosteroid therapy provides prompt resolution of PG. Of note, up to 20% to 30% of cases are initiated and aggravated by minor trauma, which is known as the “pathergy phenomenon” (the development of a new inflammatory lesion at the site of trauma). Similar to the medical history in our patient, Armstrong et al. reported a case of PG secondary to total hip replacement, with a history of refractory ulceration. However, with early diagnosis and management, this patient was treated successfully with steroids. The medical history of wound complication after surgery and other indirect signs of immunogenic disease was given by our patient only after symptoms occurred; as a result, we did not initially suspect PG. Foot surgery had initiated the onset of PG in this case. Powell et al. reported that the lower limb is involved in more than 70% of patients with ulcerative PG. Charles et al. reported that the ulcers of patients with PG and arthritis seemed more refractory to treatment than those with PG alone, possibly as a result of venous insufficiency in patients with arthritis. This reasoning may partially account for the refractory wound complication in our patient since she had midfoot arthritis. Histopathology that illustrates ulcerative lesions with polynuclear neutrophil infiltrate and associated capillary network disorder is nonspecific and insufficient to differentiate from infection, especially after surgical interventions. General measures, including pain relief, bed rest, proper nutrition, and management of associated systematic diseases, are important components of treatment for PG. The treatment is contrary to the management of infection. Debridement, which can cause additional dermatologic lesions and aggravate the pathological process in the traumatized areas, is contraindicated before immunosuppressive therapy is initiated. Our case reminds orthopaedic surgeons to consider the diagnosis of PG when patients present with early superficial purulent lesions with negative cultures, especially after surgery when these lesions show rapid extension despite empiric antibiotic therapy and surgical debridement. PG requires high doses of corticosteroids or other complementary immunosuppressive drugs (e.g., human immunoglobulin, azathioprine, and cyclosporine). Skin grafts, flap transplants, and the application of bioengineered skin may be helpful for reconstruction as a complement to immunosuppressive treatment. Nakajima et al. reported their first successful reconstruction of a large soft-tissue defect resulting from repeated surgical debridement of a PG lesion after total knee arthroplasty; they used a full-thickness skin graft and a latissimus dorsi myocutaneous flap around the knee joint. It is important to emphasize that the administration of prednisolone (1 to 2 mg/kg of body weight per day) is the basis for all treatments. Powell and O’Kane recommend that systemic steroid administration be given to the patient until the graft and the donor site are healed. In our case, the flap transplant failed before the immunosuppressive treatment had begun. However, skin-grafting achieved a satisfying outcome after we had administered prednisolone. Additionally, prophylactic steroids may be indicated before surgery in patients with a history of PG. Our case report and the review of the literature demonstrate the importance for making an early diagnosis of PG and initiating immunosuppressive treatment after surgical interventions. Knowledge of the clinical character and awareness that PG is a rare but severe postoperative complication that mimics early infection can avoid delay in initiating appropriate therapy.
Reference: Fang Z, Waizy H, Berger S, Stukenborg-Colsman C, Plaass C. Pyoderma gangrenosum following orthopaedic surgery: a case report and literature review. JBJS Case Connector. 2013 Aug 28;3(3):e84.
Clostridium species infection
Atypical mycobacterium infection
Necrotizing fasciitis
Pyoderma gangrenosum
Methicillin-resistant Staphylococcus aureus



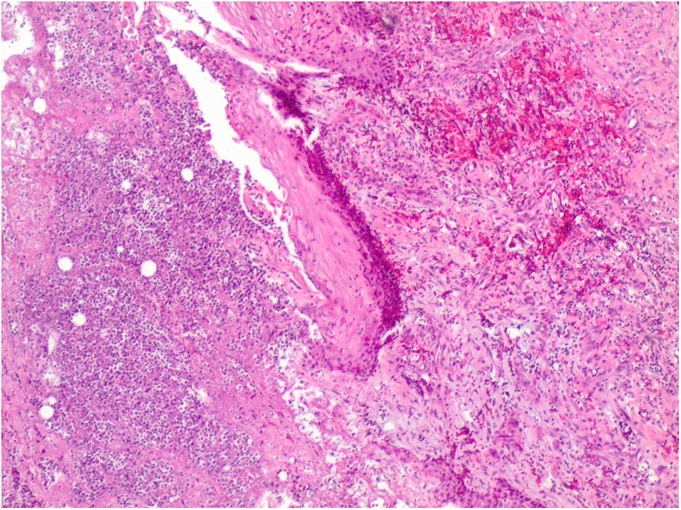


 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5
Fig. 5