A sixty-one-year-old man presented with what appeared to be a red rash that had presented on the right knee three months after a total right knee arthroplasty for severe osteoarthritis damage. DePuy Sigma implants and DePuy SmartSet Bone Cement (DePuy Orthopaedic) had been used for the procedure. The patient failed to respond to several courses of oral antibiotics, topical miconazole, and topical corticosteroids for possible postsurgical wound infection, tinea corporis, and contact dermatitis, respectively. Examination revealed a healthy-appearing man with no systemic symptoms. He had a subtle 8 × 7-cm blanchable erythematous patch without warmth or tenderness that was located lateral to the surgical scar on the right knee (Fig. 1). A biopsy was performed.
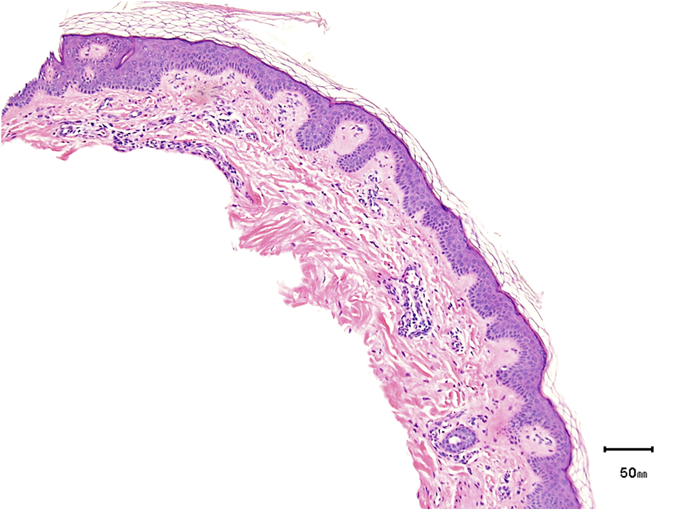
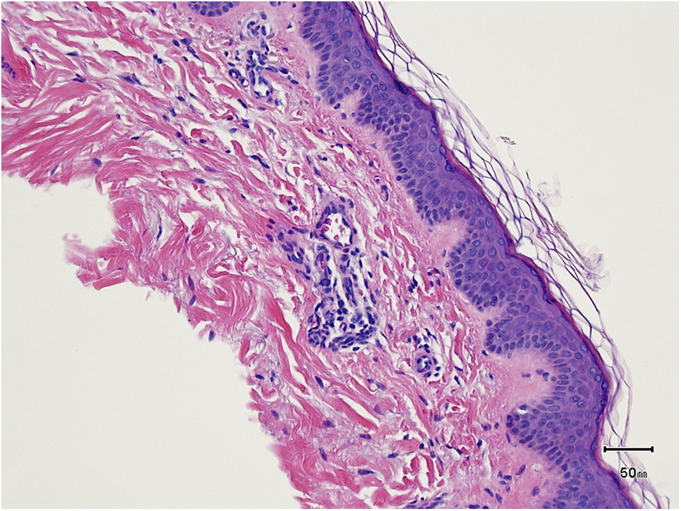
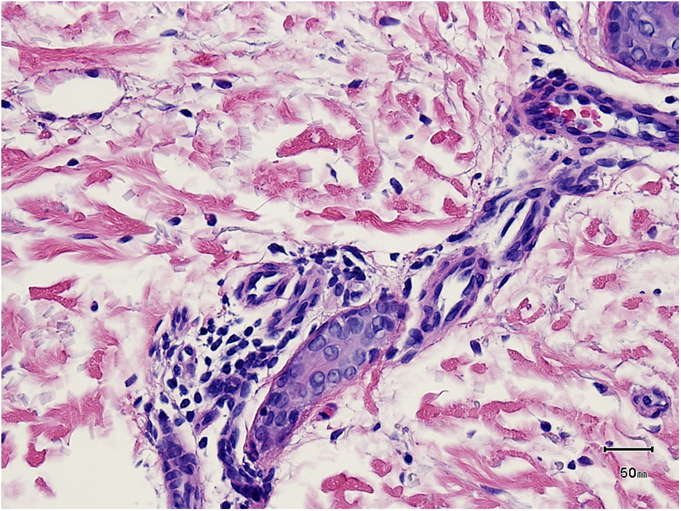
Histological findings showed sparse telangiectasias without perivascular lymphocytes and no features of angioendotheliomatosis and cutaneous pyoderma (Figs. 2-A, 2-B, and 2-C). These histological findings were compatible with reticular telangictatic erythema (RTE). At the six-month follow-up, the RTE had completely resolved (Fig. 3).
Proceed to Discussion >>Reference: Do HK, Mousdicas N. Reticular telangiectatic erythema after total knee replacement surgery: a report of two cases. JBJS Case Connector. 2013 May 22;3(2):e49.
Telangiectasias are chronically dilated preexisting blood vessels in the skin. They commonly represent a so-called wear-and-tear effect of the skin. Many pathogenic etiologies can give rise to telangiectasias, including aging, chronic sun exposure, rheumatic diseases, hereditary diseases, and estrogen-induced conditions. RTE is a benign cutaneous process involving dilated blood vessels in a reticulated network pattern that is associated with an underlying medical prosthesis. It is an asymptomatic, nontender, erythematous, nonpalpable but blanchable patch of telangiectasias in a reticular or blotchy pattern in close proximity to implant sites. These devices include cardiac defibrillators, orthopaedic prostheses, morphine pumps, sternal wiring for coronary artery bypass grafting, and spinal cord stimulators. The pathogenesis of RTE formation needs additional elucidation. It has been hypothesized that the formation of this benign cutaneous reaction that is associated with implantable devices can be caused by a localized electromagnetic field or heat generated by the device, which causes damage to the surrounding skin, or by mechanical impingement to the superficial and deep vascular beds of the surrounding skin, caused by the device generating a localized passive hyperemia. Although RTE can persist for years, most cases become less visible over time. RTE has been reported to completely resolve following removal of the implanted device. It has been speculated that RTE is an allergic reaction. Most orthopaedic implants are composed of metal alloys that contain classic contact allergens, including nickel, cobalt, and chromium. However, closed patch testing has failed to identify responsible allergens in the majority of the reported cases of RTE. Three case reports have described positive skin reactions but, according to the authors, they did not have associated clinical relevance to the pathogenesis of RTE. Although patch testing has not had a high predictive value of success in the general population, Atanaskova Mesinkovska et al. reported a higher frequency of positive skin tests in a subset of arthroplasty patients who had a history of metal allergy when compared with arthroplasty patients who did not have a history of metal allergy. RTE associated with medical prosthetic implantation is a rare cutaneous manifestation with distinct clinical and histological features that are unrelated to allergic contact dermatitis. Clinical clues are both the spatial relationship (RTE located on or near the device) and the temporal relationship (appearance of the rash after placement of the device). Examination reveals a patch of blotchy or reticulated blanchable telangiectatic erythema with no signs of frank eczematous weepy dermatitis or tenderness, warmth, edema, or purulent discharge to suggest possible contact dermatitis or an infectious process. Furthermore, RTE exhibits histological findings of vascular dilation, usually with a mild perivascular lymphohistiocytic infiltrate. Finally, RTE is associated with negative cultures for infectious agents and negative closed patch testing for relevant antigens. We present this case to highlight the existence of RTE, a benign cutaneous entity that is different from allergic contact dermatitis. Clinical recognition will allow for prompt reassurance to the patient and avoidance of unnecessary and expensive investigations and treatments. In cases where there may be a question as to the definitive diagnosis, patch testing with an appropriate orthopaedic and metal series of allergens as well as punch biopsy of the skin could be useful.
Reference: Do HK, Mousdicas N. Reticular telangiectatic erythema after total knee replacement surgery: a report of two cases. JBJS Case Connector. 2013 May 22;3(2):e49.
Intralymphatic histiocytosis
Pressure dermatitis
Reticular telangiectatic erythema
Cutaneous fungal infection
Intravascular reactive angioendotheliomatosis


 Fig. 1
Fig. 1 Fig. 2-A
Fig. 2-A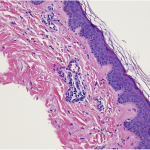 Fig. 2-B
Fig. 2-B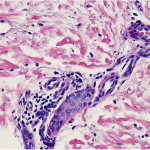 Fig. 2-C
Fig. 2-C Fig. 3
Fig. 3