A Thirty-Year-Old Man with Back Pain and Leg Weakness
June 19, 2013
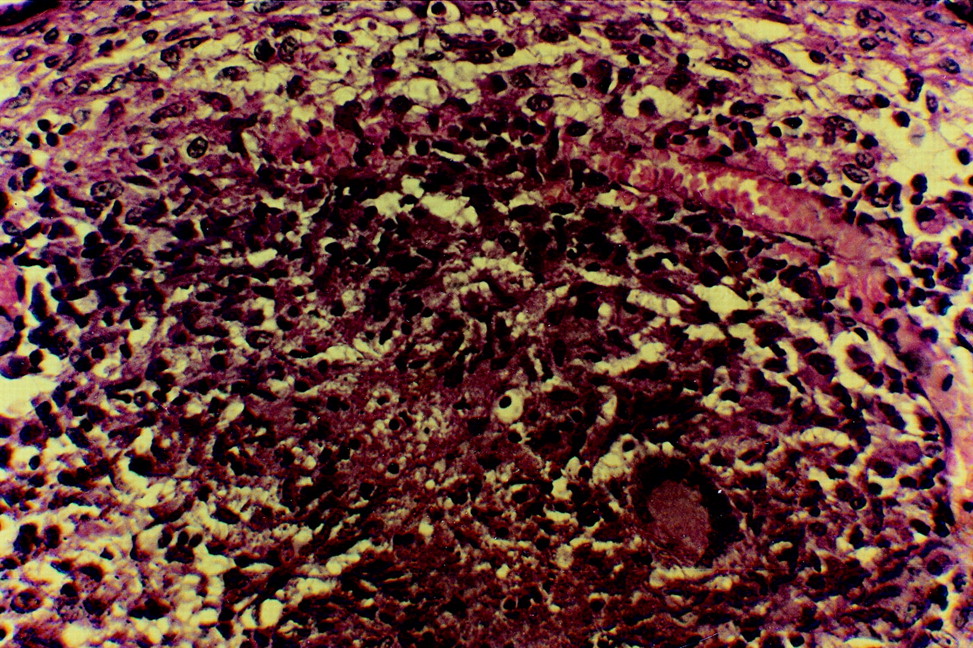
A thirty-year-old man who is a native of India presented with a one-month history of pain in the lumbar region, difficulty walking for one week, and urinary hesitancy for two days. There was weakness of the ankle plantar flexors (grade-2 of 5 strength) and dorsiflexors (grade-2 of 5 strength), and both ankle reflexes were absent. Hypoesthesia in the fourth lumbar to fifth sacral dermatomes (the right side was greater than the left) was noted. There was no deformity, but tenderness was elicited over the spinous processes of the third and fourth lumbar vertebrae. Radiographs of the lumbosacral spine revealed a loss of sharpness of the margins of the laminae of the fourth lumbar vertebra (Fig. 1). Magnetic resonance imaging of the lumbosacral spine showed altered signal intensity (a hyperintense signal in the T2-weighted image and a hypointense signal in the T1-weighted image) in the posterior elements of the third lumbar to the first sacral vertebra and in the posterior portions of the fourth and fifth lumbar vertebral bodies, with a large multiloculated fluid collection in the right paraspinal region. This epidural fluid collection caused marked extradural compression of the thecal sac and the cauda equina from the third lumbar to the first sacral vertebra (Figs. 2 and 3). Surgical exploration of the lumbosacral spine (the second lumbar to first sacral vertebrae) through a posterior midline approach was done. The laminae of the third and fourth lumbar vertebrae had roughened surfaces. Portions of these laminae were soft to the touch; however, no discontinuity was found. The diseased laminae of the third and fourth lumbar vertebrae were removed, and greenish-yellow pus was drained. The cauda equina was found ensheathed in what appeared to be an inflammatory membrane. Following careful removal of this membrane, the dural sheath was found to be intact and dural pulsations were present. A culture of the pus was sterile, and a biopsy specimen from the inflammatory membrane and resected osseous tissue was evaluated (Fig. 4).
The biopsy specimen from the inflammatory membrane and resected osseous tissue showed a typical tubercular granuloma with Langhans giant cells, epithelioid cells, and round cells, confirming the diagnosis of tuberculosis (Fig. 4). Antitubercular drug therapy (isoniazid, rifampin, pyrazinamide, and ethambutol) was started. The patient was continued on the four-drug antitubercular therapy (isoniazid, rifampin, pyrazinamide, and ethambutol) and bed rest. The surgical decompression and multidrug therapy resulted in rapid improvement in the neurological signs and a satisfactory recovery. Within twelve weeks, the patient had no motor weakness, sensory deficit, or bladder or bowel symptoms. The medical therapy was changed to two drugs (isoniazid and rifampin) at three months and was continued for a total of eighteen months. The patient was able to walk without any support six months after surgery. Normal alignment of the lumbosacral spine was maintained, and the patient was free of symptoms at the last follow-up examination at twenty-four months after surgery.
Proceed to Discussion >>Reference: Kapoor SK, Garg V, Dhaon BK, Jindal M. Tuberculosis of the posterior vertebral elements: a rare cause of compression of the cauda equina. A case report. J Bone Joint Surg Am. 2005 Feb;87(2):391-4.
Tuberculosis of the lumbosacral spine is uncommon, representing 3% of the cases in a series of 600 patients with spinal tuberculosis. Pain in the lumbosacral region is the most frequent symptom, and neurological involvement in this region of the spine is rare, as the vertebral canal is relatively large and contains the cauda equina rather than the spinal cord. Isolated involvement of vertebral laminae and/or posterior spinous processes is rare, and the prevalence has varied; however, it represented <2% of the 600 patients described by Tuli, 0.2% of the >2000 patients reported on by Adendorff et al., and 10% of the 228 patients in the study by Babhulkar et al. Since tuberculosis of the posterior vertebral elements (the pedicles, transverse processes, laminae, and spinous process) alone is rare, there is often a delay in the diagnosis and irreversible neurological sequelae may occur. However, with magnetic resonance imaging, the disease process can be seen in the very early stage of reactive bone-marrow edema, before osseous destruction has occurred, and the diagnosis can be established along with the clinical findings. Treatment started during this stage may prevent morbidity, spinal deformity, or even cord compression due to vertebral collapse. Anterior or anterolateral decompression is the appropriate surgical approach for operative management of the classic paradiscal form of tuberculosis, whereas we believe that laminectomy is required in such atypical cases of neural arch tuberculosis. Extrapulmonary tuberculosis is spread hematogenously. The typical paradiscal involvement in tuberculosis is explained by arterial spread. The uncommon involvement of the posterior element is better explained by venous spread. The posterior external venous plexus of vertebral veins is located on the posterior surfaces of the laminae and around the spinous, transverse, and articular processes. They anastomose freely with the other vertebral venous plexuses and constitute the final pathway for the infection to reach the neural arch. Such uncommon presentations are diagnosed on clinical suspicion, and appropriate diagnostic studies need to be obtained early. Once the diagnosis of tuberculosis of the posterior vertebral elements was established in our patient, the functional results following treatment were dramatic.
Reference: Kapoor SK, Garg V, Dhaon BK, Jindal M. Tuberculosis of the posterior vertebral elements: a rare cause of compression of the cauda equina. A case report. J Bone Joint Surg Am. 2005 Feb;87(2):391-4.
Cryptococcus infection
Toxoplasmosis
Tuberculosis
Behcet disease
Lyme disease

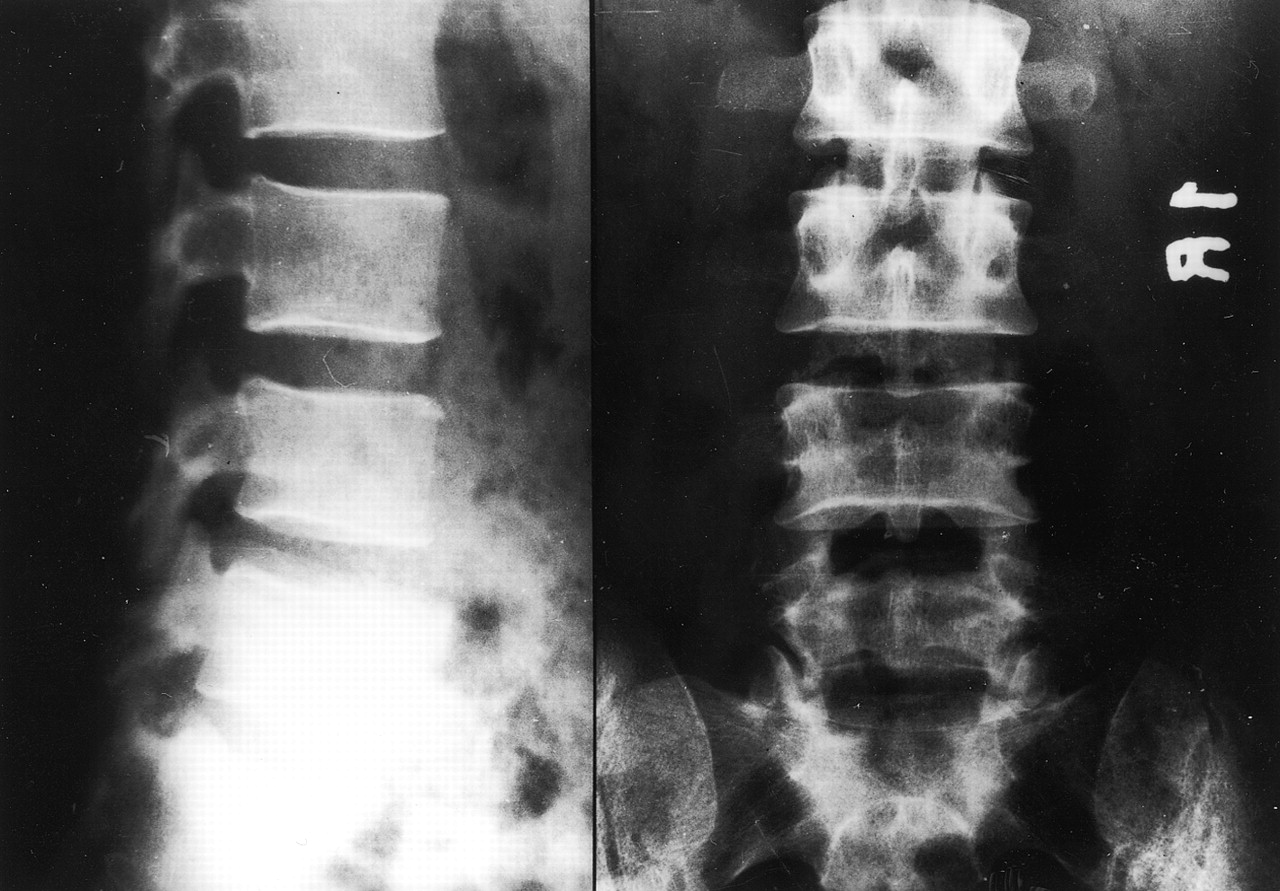
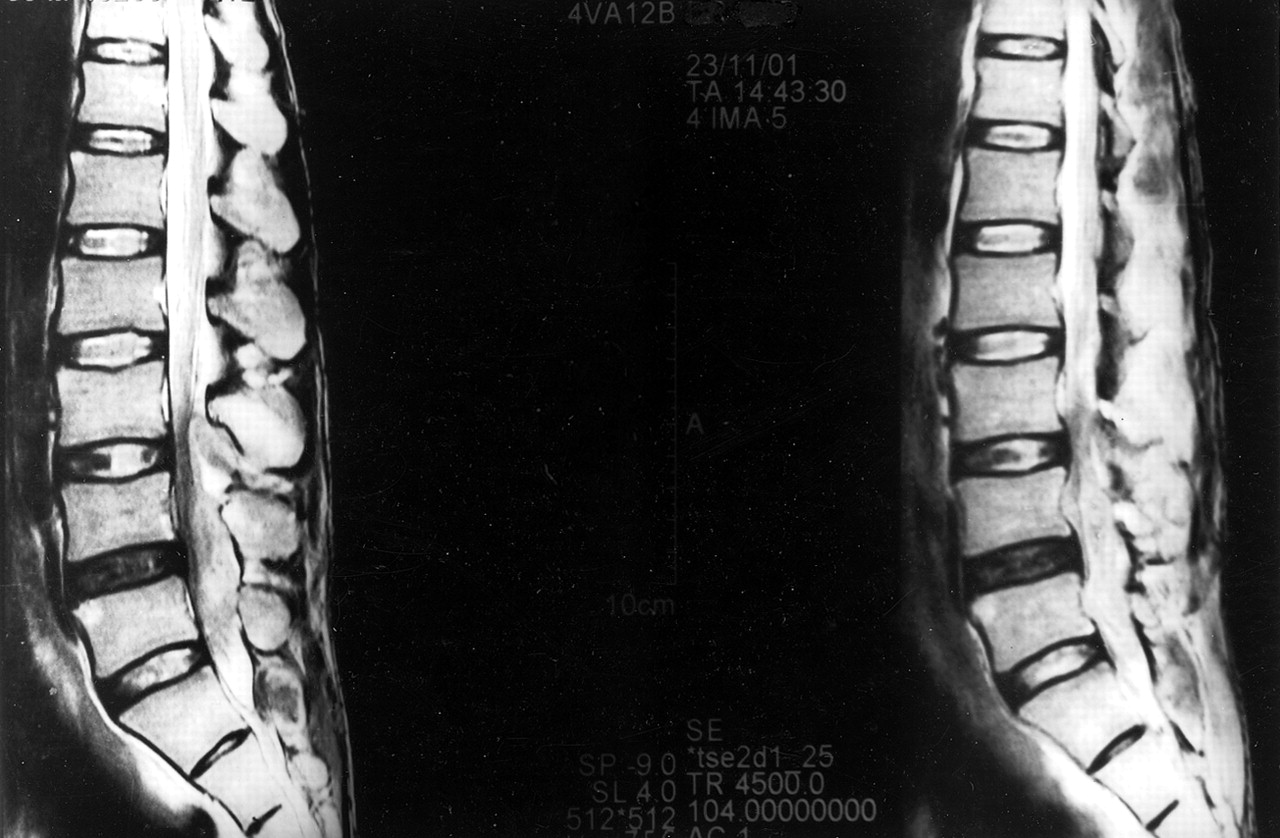
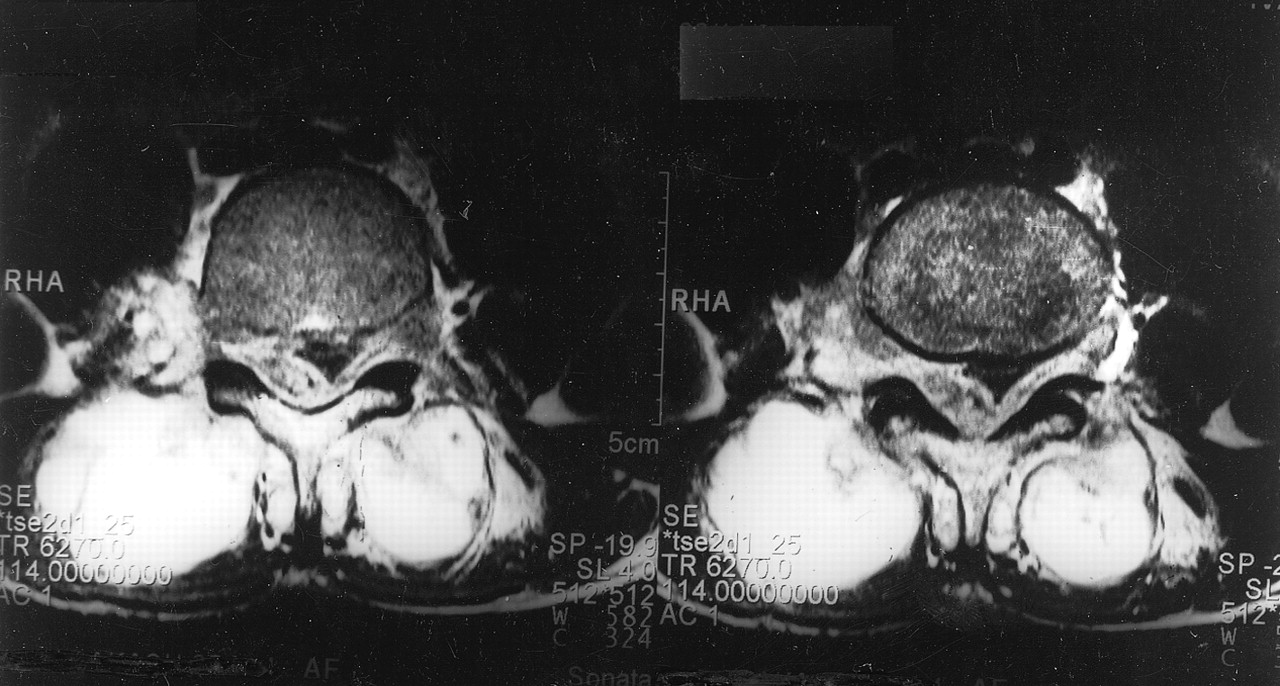
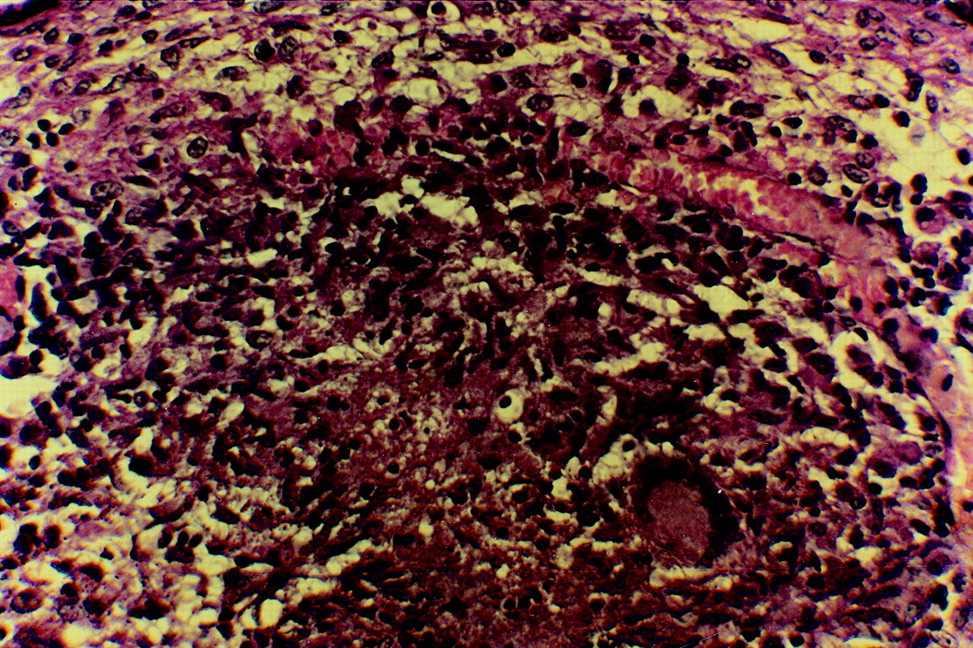
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4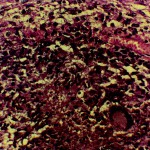 Fig. 4
Fig. 4