A Sixty-Year-Old Man with Acute Wound Redness Eight Weeks After Hip Replacement
January 16, 2013
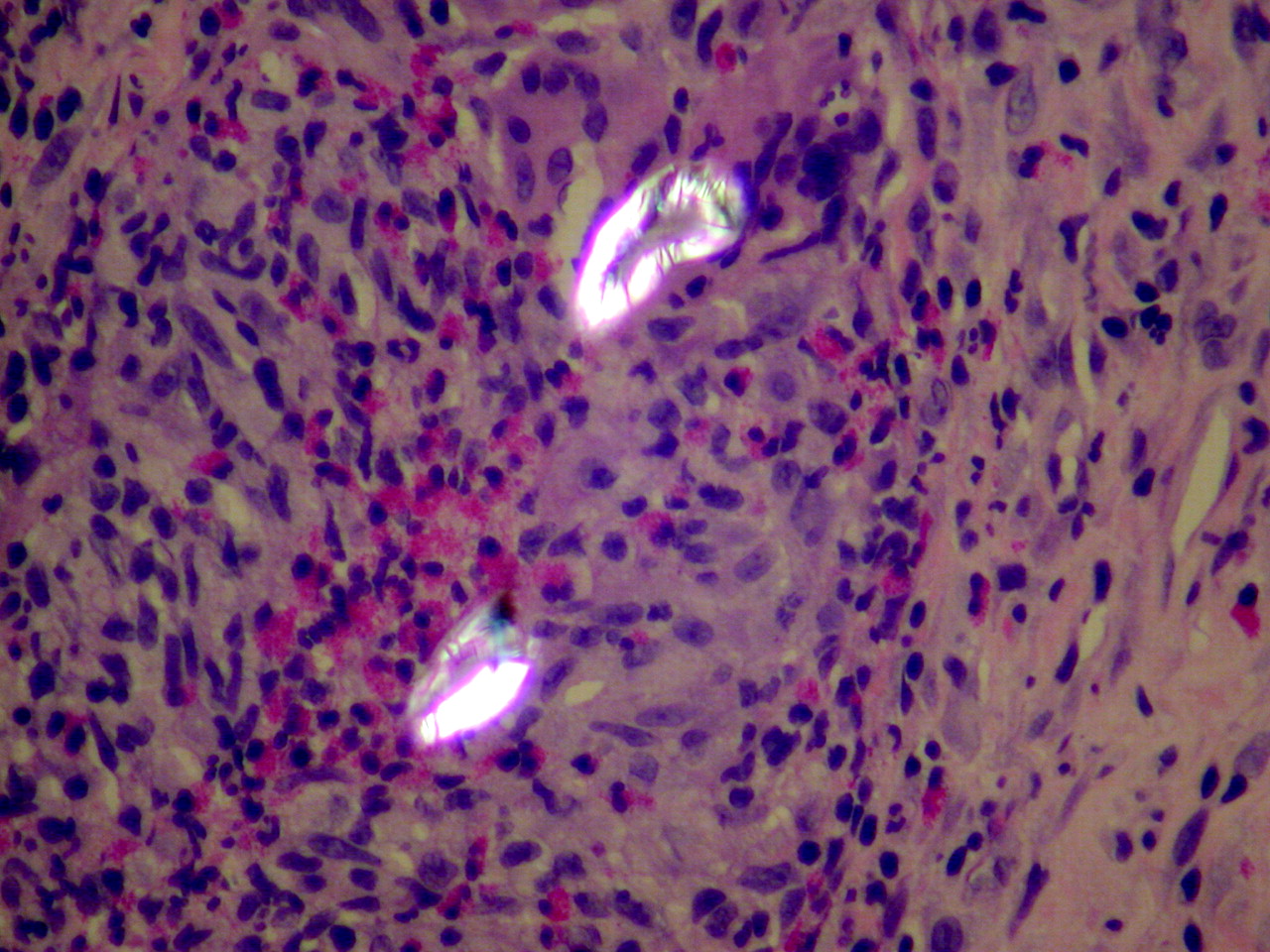
A sixty-year-old man underwent total hip arthroplasty for osteoarthritis (uncemented acetabular component, cemented femoral component). Wound closure was routine with the deep and superficial fascial layers closed with coated Vicryl suture. Staples were used for the skin closure. The initial postoperative course was uneventful; there were no symptoms or signs of abnormal wound-healing or unusual pain. Eight weeks after the operation, the patient noticed redness that progressed rapidly (within twenty-four hours) along the entire length of the surgical incision. When seen by his surgeon the following day, the patient was not in pain but was mildly febrile with a temperature of 37.9°C. The entire surgical incision was swollen and moderately erythematous, and there was some seropurulent drainage. Laboratory examination revealed a normal white blood-cell count (9.4 × 109/L), hypereosinophilia (12% [normal, 0% to 7%]), a normal erythrocyte sedimentation rate (16 mm/hr), and an elevated C-reactive protein level (65 µg/L). A presumptive diagnosis of acute wound infection was made, and the patient was taken directly to the operating room. During surgery, multiple punctate centers of abscess formation were noted in the subcutaneous tissue. Specimens were obtained for culture, and the deep fascia was opened. Similar abscesses were noted to extend down to the joint capsule. The hip joint was opened; there was no intra-articular fluid. Multiple specimens were obtained for culture. The prosthesis was dislocated, the capsule was débrided, and the joint was thoroughly irrigated. All abscesses were débrided. The prosthesis was left in place, the scar was excised, and the wound was closed. Pathologic examination revealed numerous foreign-body giant-cell granulomas with acute and chronic inflammation containing a large number of eosinophils (Fig. 1).
All initial Gram stains and cultures (bacteria, mycobacteria, and fungus) were negative. The patient was treated with antibiotics pending the final culture reports. However, because those reports indicated that all cultures were negative and because the postoperative clinical course had been benign, the antibiotic therapy was discontinued. Polarized light microscopy of the tissue removed at the irrigation and debridement surgery revealed the foreign bodies to be strongly birefringent, corresponding to suture material (Fig. 2). The diagnosis of granulomatous reaction to suture material was confirmed. At the most recent follow-up visit thirteen months postoperatively, the patient was asymptomatic and had excellent restoration of hip function. No additional wound abnormalities had occurred.
Proceed to Discussion >>Reference: Sayegh S, Bernard L, Stern R, Pache JC, Szalay I, Hoffmeyer P. Suture granuloma mimicking infection following total hip arthroplasty. A report of three cases. J Bone Joint Surg Am. 2003 Jan;85(10):2006-9.
To our knowledge, granulomatous reaction to suture material following total hip arthroplasty has not been reported as a complication. Granulomatous inflammation is a distinct type of chronic inflammation that is characterized by an accumulation of activated epithelioid macrophages. There are two types of reactions: the nonimmunologic, foreign-body reaction, and the immunologic, hypersensitivity reaction. Granulomas of the foreign-body-reaction type consist of macrophages that have been activated by the ingestion of material. They form multinucleated giant cells that contain foreign material. The undegraded ingested materials induce the macrophage to secrete degradative enzymes, which in turn stimulate blood-borne monocytes to converge around the macrophages and create a granuloma. Standard light microscopic examination of specimens from our patient showed multinucleated giant cells containing a large number of eosinophils and some neutrophils encircled by epithelioid histiocytes. Importantly, the suture material was not visible with use of standard microscopy but, because of its strong birefringence, was visible with use of polarized light microscopy. Suture granulomas have produced perplexing diagnostic problems following general surgery, as they have mimicked neoplasm or infection. They have been seen as late as ten years after the index operation. Suture (usually nonabsorbable) granulomas mimicking neoplasms have been reported following surgery of the eye, bladder, biliary system, lung, colon, esophagus, head and neck, omentum, and breast as well as after hernia repair and after closure of a ventricular septal defect. The orthopaedic literature contains two case reports of bone and joint involvement by a necrotizing suture granuloma years after the use of silk suture during the original operation. In comparison to natural sutures such as catgut and treated catgut, synthetic absorbable sutures are much less likely to cause a foreign-body reaction, whereas sutures of polyglycolic acid (Dexon) and polyglactin 910 (Vicryl) have been associated with abscess, granuloma, or sinus formation. Also, it has been reported that bioabsorbable fixation with polyglycolide devices may lead to an inflammatory reaction and granuloma formation Böstman reported that a foreign-body reaction occurred in seventy-four patients after fracture stabilization with absorbable pins and screws, and that moderate or severe osteoarthritis of the ankle developed in ten of those patients three to nine years after the operation. Inflammatory changes, synovitis, and osteolysis have been reported in studies of sheep after fracture fixation with such implants. In our patient, intraoperative findings revealed multiple punctate abscesses in the subcutaneous tissue as well as deep to the fascia and extending to the capsule of the hip joint. The surgical procedure consisted of excision of the affected tissues, débridement of the joint capsule, and extensive wound lavage. The prosthesis was left in place. Gram stains and final cultures (bacteria, mycobacteria, and fungus) were all negative. Pathologic findings showed numerous giant-cell granulomas and large numbers of eosinophils. Analysis with polarized light microscopy revealed strongly birefringent linear foreign bodies corresponding to surgical suture material. Although true postoperative infection following total hip arthroplasty is more frequent, granulomatous suture reaction must be considered when the cultures are negative but local hypereosinophilia and signs of infection are present. The diagnosis can be confirmed by pathologic examination. In conclusion, when making a differential diagnosis, it is important to consider the possibility of a foreign-body granuloma that mimics infection and to understand the value of polarized light microscopy in making the correct diagnosis.
Reference: Sayegh S, Bernard L, Stern R, Pache JC, Szalay I, Hoffmeyer P. Suture granuloma mimicking infection following total hip arthroplasty. A report of three cases. J Bone Joint Surg Am. 2003 Jan;85(10):2006-9.
Granulomatous reaction to talc
Granulomatous reaction due to fungal infection
Uric acid deposits from unrecognized gout
Granulomatous reaction to Vicryl suture
Granulomatous reaction to implant biomaterials


 Fig. 1
Fig. 1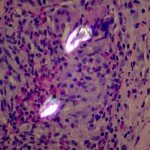 Fig. 2
Fig. 2