A Ten Year Old Boy with a Two-Month History of Neck Pain
September 1, 2010
A ten-year-old boy was admitted to our institution for evaluation of a two-month history of neck pain associated with slight restriction of head rotation. The neck pain was continuous and progressively increasing, and the use of nonsteroidal anti-inflammatory medication had resulted in no improvement. Radiographs of the cervical spine revealed no abnormality. Technetium-99 methylene diphosphonate bone scintigraphy showed increased uptake on the left side of the upper cervical spine and no other skeletal lesions. A computed tomography scan revealed an osteolytic lesion in the left lateral mass of the atlas (Fig. 1-A).
The patient wore a stiff cervical collar for three months. By the end of that time, the symptoms had resolved and he had regained full motion of the neck. A computed tomography scan performed six months later showed complete reconstitution of the lateral mass of the atlas (Fig. 1-B). At the time of the six-year follow-up, he continued to be free of symptoms and computed tomography studies showed no evidence of recurrence.
Proceed to Discussion >>Reference: Puigdevall M, Bosio S, Hokama J, Maenza R. Langerhans cell histiocytosis of the atlas in the pediatric spine: total reconstitution of the bone lesion after nonoperative treatment. A report of two cases. J Bone Joint Surg Am. 2008;90:1994-7.
Involvement of the cervical spine is rare in children who have Langerhans cell histiocytosis, with the C3-C5 region being the most commonly involved location. There is usually an acute or gradual onset of neck pain with restricted range of motion or the presence of torticollis. Usually, there is no history of trauma. Laboratory findings are usually within normal limits. Neurological symptoms are rare in patients with cervical involvement and tend to occur more in patients with thoracic or lumbar involvement. Langerhans cell histiocytosis commonly affects the vertebral body, with less than 30% of the cases involving the posterior elements. It produces a rapidly destructive bone lesion, with varying degrees of vertebral collapse. The term vertebra plana is used if there is a complete collapse of the vertebral body. Many authors agree that a vertebra plana is pathognomonic of Langerhans cell histiocytosis and suggest that a biopsy is unnecessary in the presence of this radiographic finding, although a complete collapse of the vertebral body may be seen in many other bone lesions. Vertebra plana is seen in only 20% of the cases of Langerhans cell histiocytosis involving the cervical region in children, so this classic radiographic presentation is more the exception than the rule. In these children, the most common radiographic sign is a lytic lesion of the cervical vertebral body. In the atlas, the lateral mass represents the vertebral body; thus, Langerhans cell histiocytosis is usually associated with an osteolytic lesion in the lateral mass. The atlas is very difficult to see on radiographs and, as was the case in our two patients (see reference list for full case report), a computed tomography scan is usually necessary to depict the osteolytic lesion. The differential diagnosis of cervical pain when there is an osteolytic vertebral lesion seen on imaging studies includes benign fibrous histiocytoma, osteoid osteoma, osteoblastoma, giant-cell tumor, aneurysmal bone cyst, hemangioma, nonossifying fibroma, vertebral infection, and malignant neoplasms such as osteosarcoma and Ewing sarcoma. Many of these entities may also produce a complete collapse of the vertebral body, with a radiographic appearance of vertebra plana. As a result, some authors recommend computed tomography-guided percutaneous needle biopsy to confirm the diagnosis by histopathological evaluation. We support the recommendation of biopsy of any cervical osteolytic bone lesion, including those associated with vertebra plana. In patients who have multiple bone involvement, as did one of our patients, the biopsy can be made at the site that is most accessible. A technetium-99 methylene diphosphonate bone scan or a complete skeletal survey must be done routinely as part of the staging process to search for other sites affected with Langerhans cell histiocytosis. Some authors do not recommend bone scintigraphy as a screening method because of its poor sensitivity, while others prefer a technetium bone scan because the total dose of radiation is less than that associated with a skeletal survey. In both of our patients, the bone scans were positive and led to the computed tomography scan of the upper cervical spine. When the result of the technetium-99 methylene diphosphonate bone scan is negative, a complete skeletal survey may be necessary to exclude other lesions. In younger patients who, because of their age, are at a higher risk of having multisystem disease, consideration should be given to the performance of computed tomography scans of the chest, abdomen, and pelvis to search for visceral involvement. Several methods have been used for the treatment of Langerhans cell histiocytosis of the cervical spine, including immobilization, radiation therapy, chemotherapy, surgery, or combinations of these approaches. Other authors have reported the self-limiting course of this condition, and there is a general consensus that the prognosis for an isolated bone lesion is generally good, with often spontaneous remission of the disease. Patients who have multifocal osseous Langerhans cell histiocytosis but no visceral involvement also have a favorable prognosis. Satisfactory results have been reported with immobilization of the cervical spine. Our two patients with Langerhans cell histiocytosis of the atlas, one of them with multiple vertebral involvement, had complete reconstitution of the bone lesion with such nonoperative treatment. It is not possible to know if the reconstitution would have also occurred without the neck brace, but the brace also served to alleviate the patient's symptoms. Surgery has its specific indications and should be considered when there is a need for stabilization of the spine due to an extensive lesion that compromises mechanical stability or in the presence of neurological symptoms due to compression of the spinal cord by the collapsed vertebra or the soft-tissue mass itself. Multiple-agent chemotherapy should be reserved for patients who have multifocal lesions or visceral involvement. In the opinion of many authors, radiation therapy should not be used as a first-choice treatment in pediatric patients because there may be an increased risk of malignant secondary changes as well as nondesirable side effects on the mucosa of adjacent tissues (the trachea and the esophagus). There is also some concern regarding vertebral growth-plate damage in the skeletally immature patient. Because of this potential morbidity, radiation therapy is reserved for selected patients in whom the disease continues to progress. We agree with others that there is no single strategy in the treatment of Langerhans cell histiocytosis of the cervical spine. The treatment depends on the extent of the disease and on the neurological or mechanical conditions produced by the bone lesion. However, regardless of the treatment method used, the outcome in the reported cases of cervical Langerhans cell histiocytosis generally has been good. Our two patients with Langerhans cell histiocytosis of the atlas were managed satisfactorily with immobilization of the cervical spine and had complete reconstitution of the bone lesion. The cases of these patients add support to the idea that the natural history of Langerhans cell histiocytosis of the cervical spine is benign, since these lesions can resolve without surgical treatment. Based on these findings, we recommend a nonoperative approach to Langerhans cell histiocytosis of the atlas when there are no neurological or mechanical complications.
Reference: Puigdevall M, Bosio S, Hokama J, Maenza R. Langerhans cell histiocytosis of the atlas in the pediatric spine: total reconstitution of the bone lesion after nonoperative treatment. A report of two cases. J Bone Joint Surg Am. 2008;90:1994-7.
Aneurysmal bone cyst of C1
Osteomyelitis of C1
Langerhans cell histiocytosis of C1
Unicameral bone cyst of C1

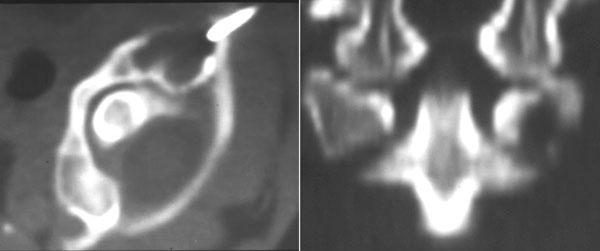
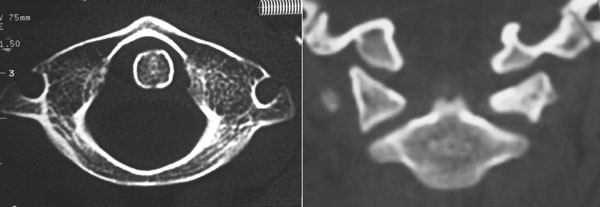
 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B