A Thirty-five-Year-Old Man with Progressive Leg Weakness
October 17, 2012
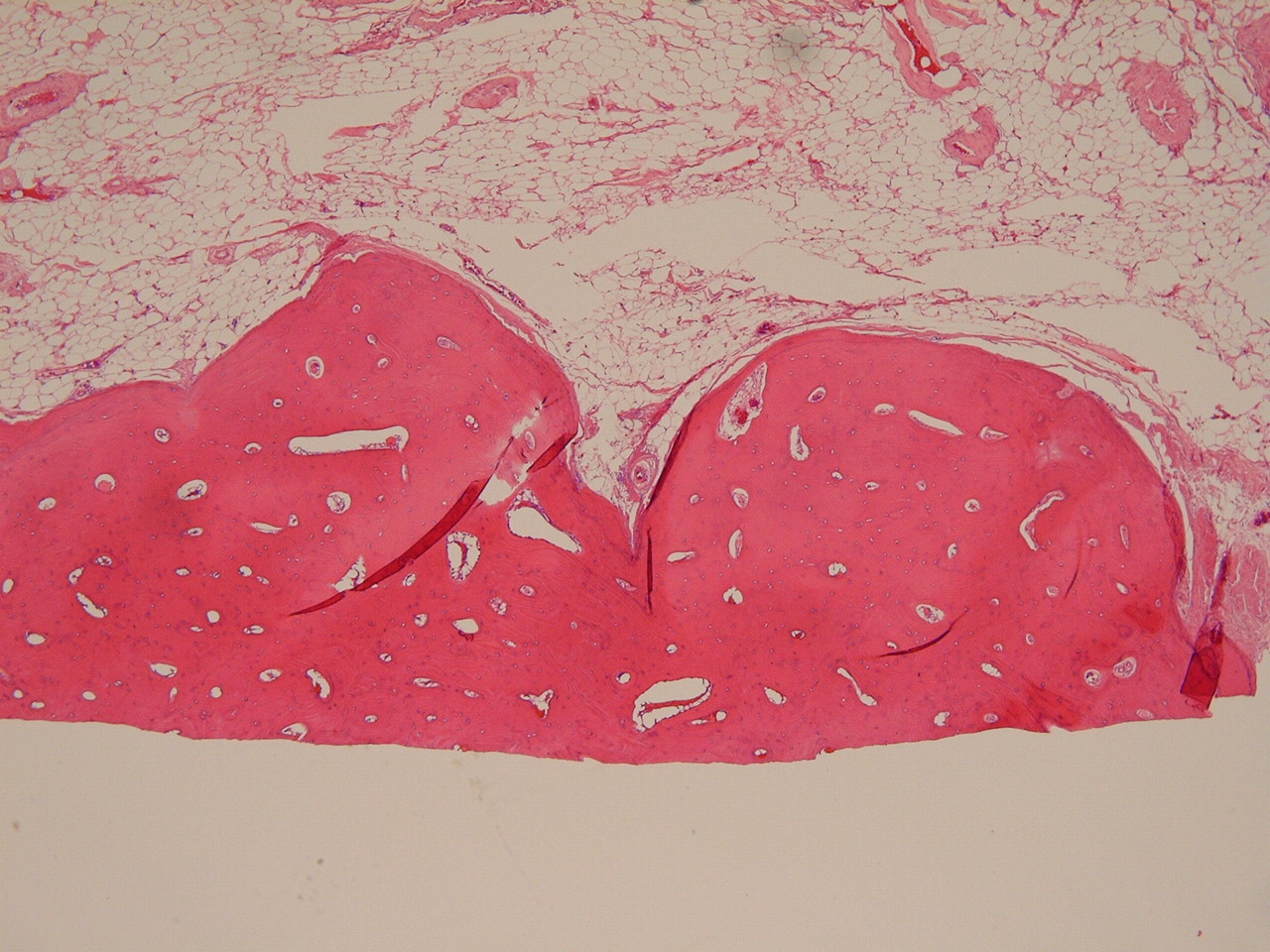
A thirty-five-year-old man was evaluated as an outpatient for the subjective complaint of progressive bilateral lower extremity weakness and difficulty with walking. The patient reported that the weakness had started one year prior to presentation and had been progressive in nature with substantial worsening during the previous two months. The patient stated that he was able to walk only one-half block with the assistance of a cane. He also reported difficulty rising from a seated position, with numbness of both lower extremities, and the recent development of urinary frequency. He stated that he had not had any fevers, chills, night sweats, dysuria, or urinary incontinence. The medical history was positive for a diagnosis of fibrous dysplasia due to multiple rib lesions noted on a chest radiograph made twenty years earlier. The patient was not taking any medication and had been participating in physical therapy without any notable improvement in lower extremity strength. On physical examination, the patient was 1.6 m tall and weighed 150 kg. He walked with a wide-based, shuffling gait with extreme difficulty, requiring the assistance of a cane. Pertinent findings on motor examination included bilateral muscle strength of grade 4 of 5 for the iliopsoas and quadriceps, grade 3 of 5 for the tibialis anterior and gastrocnemius, and grade 2 of 5 for the extensor hallucis longus. The patient was hyperreflexic in both lower extremities and had positive Babinski signs and sustained ankle clonus. Anteroposterior and lateral radiographs of the cervical spine showed dense sclerotic hypertrophic changes involving the right first rib as well as the right posterior elements of the seventh cervical vertebra. Anteroposterior and lateral radiographs of the upper thoracic spine were difficult to interpret because of the body habitus of the patient. A radiograph of the chest demonstrated sclerotic osseous proliferation of multiple ribs on the right side. A computed tomographic scan of the cervical, thoracic, and lumbar spine demonstrated multiple areas of sclerotic hypertrophy of the ribs and anterior and posterior spinal elements on the right side. The most notable involvement was at the level of the first thoracic through the fourth thoracic vertebra, where osseous hypertrophy of the posterior elements resulted in canal stenosis that ranged from 50% to 90% (Figs. 1-A and 1-B). Because of the worsening neurologic condition, the patient agreed to proceed with a cervicothoracic decompressive laminectomy and instrumented arthrodesis. The posterior decompression was carried out pedicle to pedicle from the seventh cervical vertebra to the fifth thoracic vertebra with the use of a high-speed side-cutting burr (Fig. 2). A photomicrograph of the histological appearance of the excised lamina is shown in Figure 3.
Toward the completion of the decompression, sudden complete loss of motor signals to the lower extremities was noted on motor evoked potentials. The decompression was completed, and the instrumented arthrodesis portion of the procedure was aborted because of the intraoperative changes noted on the spinal cord monitoring and the desire to obtain nondistorted postoperative magnetic resonance images to assess spinal cord parenchymal changes. The blood pressure was continuously maintained at a mean arterial pressure of >90 mm Hg, and methylprednisolone was administered at the standardized dose for spinal cord injury (30 mg per kg loading dose followed by 5.4 mg per kg for twenty-three hours). Magnetic resonance imaging scans performed after the patient had stabilized postoperatively demonstrated edema within the spinal cord from the seventh cervical through the fourth thoracic vertebra with adequate decompression of the neural elements. Postoperatively, the patient was noted to have no motor function in the lower extremities with preservation of light touch and pinprick (T3 ASIA [American Spinal Injury Association] B with sacral sparing). The final report on the microbiological culture of the specimen indicated no growth, and melorheostosis was diagnosed on the basis of the pathological evaluation of the specimen (Fig. 3). At the time of the follow-up examination six months after surgery, the patient was noted to have 4+ of 5 strength in the iliopsoas, quadriceps, and tibialis anterior muscles bilaterally and 4 of 5 strength in the extensor hallucis longus and gastrocnemius muscles bilaterally. In addition, he had a positive Babinski sign bilaterally and sustained ankle clonus in the left lower extremity. No evidence of sagittal plane deformity either clinically or on the lateral radiograph was noted. Since the patient underwent a multilevel laminectomy that crossed the cervicothoracic junction without an arthrodesis, he is at an increased risk for the development of sagittal plane instability. Therefore, he will need evaluation with anteroposterior, lateral, and flexion-extension radiographs at regular intervals to monitor for this complication.
Proceed to Discussion >>Reference: Zeiller SC, Vaccaro AR, Wimberley DW, Albert TJ, Harrop JS, Hilibrand AS. Severe myelopathy resulting from melorheostosis of the cervicothoracic spine. A case report. J Bone Joint Surg Am. 2005 Dec;87(12):2759-62.
Since the original description of melorheostosis by Leri and Joanny in 1922, the cases of approximately 400 patients have been described in the literature. The mesodermal defect that leads to melorheostosis is unknown, but one hypothesis, espoused by Murray and McCredie, has gained favor. They suggested that an abnormality of a spinal sensory nerve or nerves enables the disease to affect that sclerotome. This theory explains why the disease process is almost always unilateral in nature and affects the osseous and soft-tissue elements within a given spinal segment or segments. In a case series of thirty patients, those authors reported that nineteen patients had abnormalities in one sclerotome and eleven had involvement of multiple sclerotomes. Typically, melorheostosis is diagnosed in young adults during the second or third decade of life, with men and women being affected equally by the disease process. Radiographs are sufficient to make the diagnosis, although computed tomography and magnetic resonance imaging may be warranted in select situations. Melorheostosis may present in a monostotic (involvement of one bone), polyostotic, or monomelic (involvement of one limb) form. The monomelic variant is the most common presentation of the disease. Campbell et al. reported on eight of fourteen patients with the disease who had the monomelic variant, and Morris et al., in a retrospective review, found that 81% of 131 patients had the monomelic variant. Other areas that are affected much less frequently include the ribs, skull, pelvis, and spine. Ossification of soft tissues adjacent to areas of osseous involvement as well as fibrolipomatous lesions and vascular and lymphatic malformations have also been reported. Involvement of the appendicular skeleton or adjacent soft tissues may present with symptoms from long-bone deformity, joint contractures, and generalized limb stiffness. Involvement of the axial skeleton may be associated with pain or signs of neural compression. The differential diagnosis for other sclerosing bone dysplasias that may affect the appendicular or axial skeleton include progressive diaphyseal dysplasia, osteopoikilosis, osteopathia striata, and possibly diffuse idiopathic skeletal hyperostosis. Typically, these entities are differentiated from melorheostosis on the basis of whether the sclerosing bone dysplasia is of endochondral bone or intramembranous formation and whether it occurs during skeletal development or at skeletal maturity. Progressive diaphyseal dysplasia is a mixed sclerosing bone dysplasia affecting predominantly intramembranous ossification that is inherited in an autosomal dominant fashion. Patients with diaphyseal dysplasia present with symmetric involvement of the extremities with fusiform thickening of the osseous cortex. Osteopoikilosis is characterized by multiple bone islands, typically clustered near the articular surfaces of long bones. Osteopathia striata is characterized by linear striations in the metaphysis or diaphysis of long bones at sites of rapid growth. In the vertebral column, diffuse idiopathic skeletal hyperostosis can produce dense osseous proliferation. The lack of syndesmophytes and unilateral involvement with melorheostosis differentiates this disorder from diffuse idiopathic skeletal hyperostosis. Fortunately, melorheostosis is a rare, benign sclerosing bone dysplasia. Involvement of the appendicular skeleton and adjacent soft tissue can result in pronounced morbidity. Nonoperative treatment is the mainstay for these symptomatic patients; however, in select patients, operative treatment is directed at the restoration of function and the reduction of pain. Involvement of the axial skeleton with neurologic sequelae is exceedingly rare, with only one such case reported in the literature as far as we know. The indication for decompression of spinal stenosis due to melorheostosis is the same as that for advanced spondylosis and is intended to relieve pressure on the affected neural elements.
Reference: Zeiller SC, Vaccaro AR, Wimberley DW, Albert TJ, Harrop JS, Hilibrand AS. Severe myelopathy resulting from melorheostosis of the cervicothoracic spine. A case report. J Bone Joint Surg Am. 2005 Dec;87(12):2759-62.
Melorheostosis
Calcified fibrous dysplasia
Osteopetrosis
Osteopoikilosis
Idiopathic skeletal hyperostosis

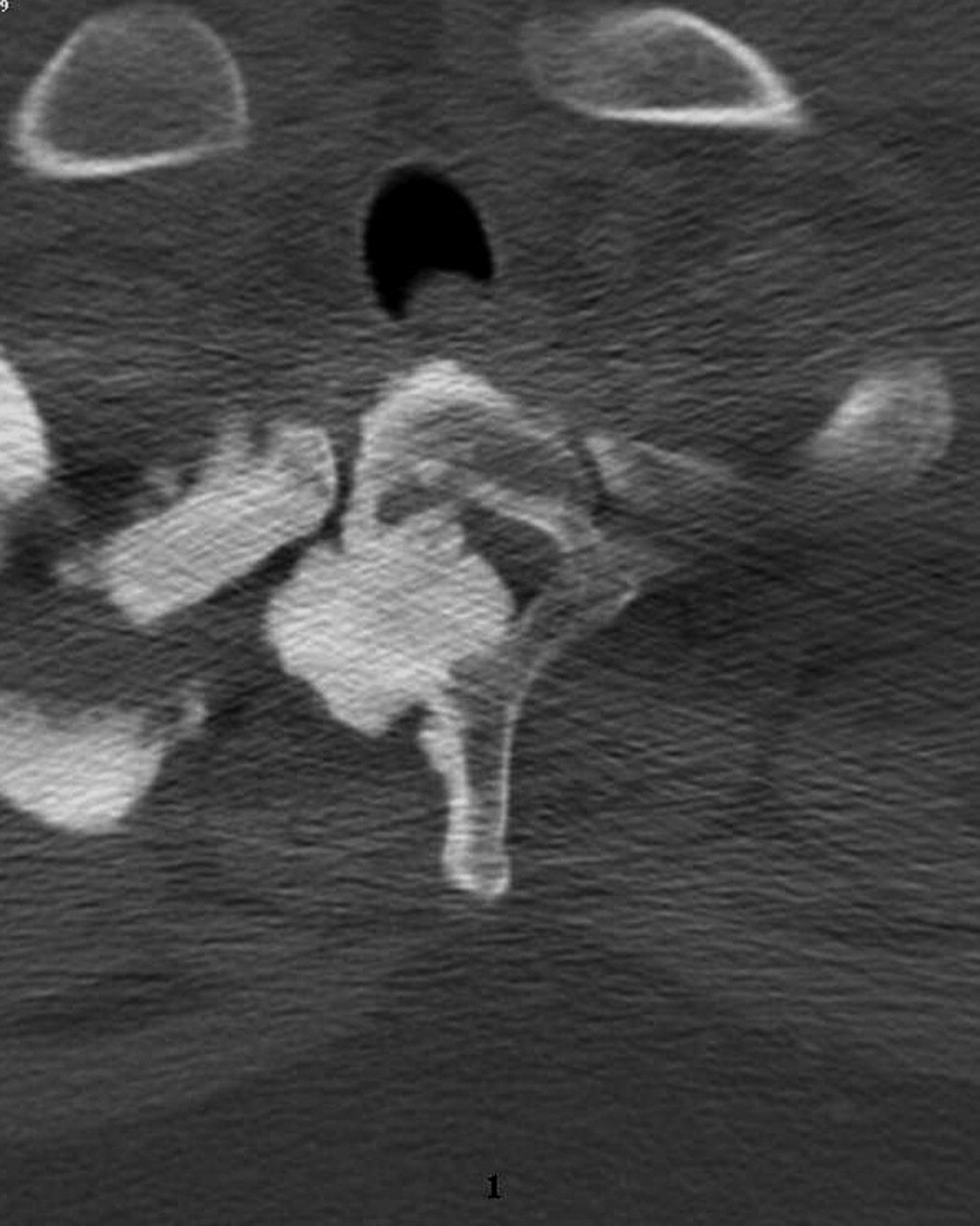
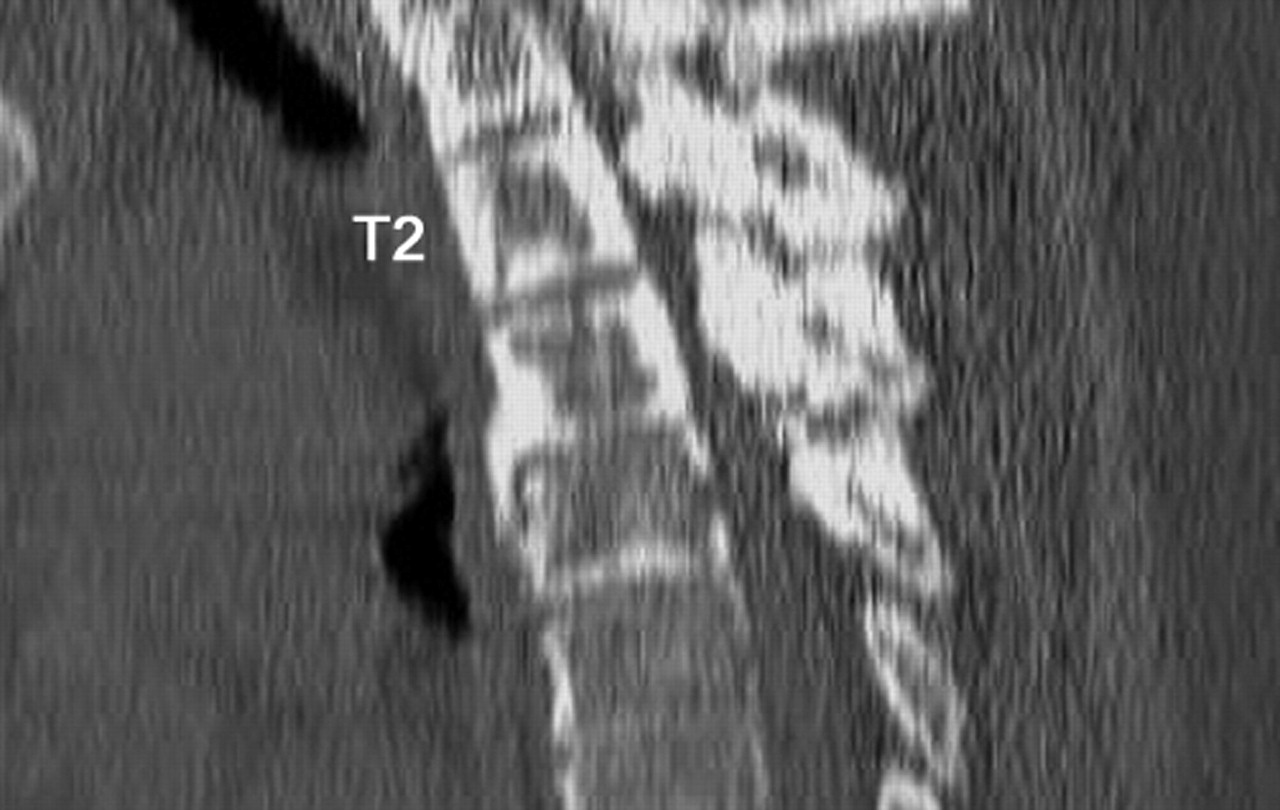

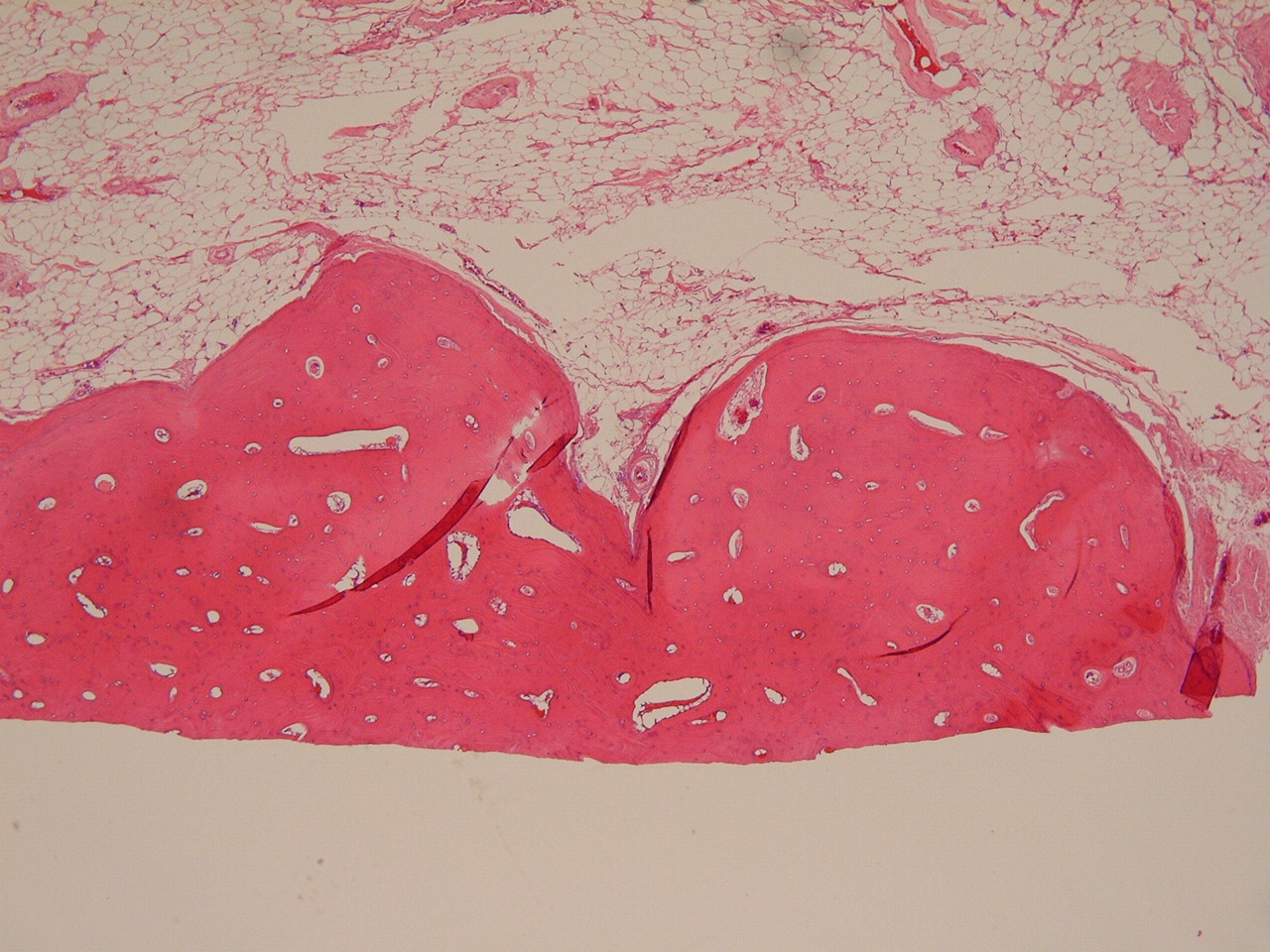
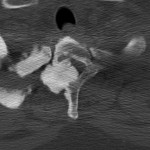 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B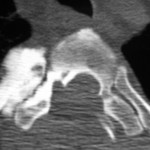 Fig. 2
Fig. 2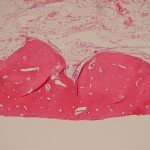 Fig. 3
Fig. 3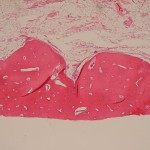 Fig. 3
Fig. 3