A Twenty-seven-Year-Old Man with Lifelong Left Foot Pain
March 19, 2014
A twenty-seven-year-old man presented with the symptom of lifelong left foot pain. He had started having problems with a “blood blister” on the plantar aspect of the second metatarsal head when he had just begun walking at the age of one year. According to his mother, after evaluation from several physicians, the lesion had been diagnosed as a benign “birthmark” that would spontaneously regress. Watchful waiting was the initial treatment of choice, but over the following years, the lesion had become progressively painful. Multiple cryotherapy and conventional wart treatments had failed to improve symptoms or eliminate the lesion. Intensity of pain increased during the six to eight months prior to presentation. A superficial debridement during that time worsened the pain and made walking difficult. Prescribed custom orthotics were of minimal benefit. Physical examination revealed a lesion under the left second metatarsal head composed of petechiae or punctate lesions, surrounded by a callus measuring 2 × 2 cm (Fig. 1). This area was extremely tender to palpation. The remainder of the foot and ankle examination was normal. To exclude hemangioma or vascular malformation, radiographs and magnetic resonance imaging (MRI) were obtained, and demonstrated a 15 × 19 × 24-mm lobular T1-weighted hypointense, T2-weighted enhancing lesion with extension into the subcutaneous tissue (Figs. 2-A and 2-B). A small area within the lesion was consistent with low-flow vascular abnormality. There was no abnormality or involvement of the musculature. Surgical excision of the lesion was performed through an incision just medial to the second metatarsal head. The entire mass was identified and removed, including 100% of the cutaneous lesion. The wound was fully closed with adequate soft-tissue coverage. The foot was placed in a walking boot, and the patient was non-weight-bearing for two weeks; he then was able to wear his normal footwear and begin weight-bearing. Histopathology revealed a gross specimen with a gray-to-tan ill-defined skin lesion that had a rough surface. The subcutaneous portions were shaggy, lobulated, yellow adipose tissue streaked with gray. Microscopic sections showed hyperkeratosis, papillomatosis, and acanthosis with dilated vascular papillae extending to the skin (Figs. 3-A and 3-B). At the one-month follow-up, the pain had greatly decreased and the wound had healed. A superficial suture that was causing irritation was removed. At the twenty-one-month follow-up, there was no evidence of recurrence on clinical examination (Fig. 4). The patient reported that he had no pain at the surgical site with weight-bearing or at rest. No additional procedures have been performed.
Reference: Haskins SM, Shields NN. Verrucous hemangioma of the plantar surface of the foot: a case report. JBJS Case Connector. 2014 Jan 22;4(1):e10.
Verrucous hemangiomas were first defined and characterized in the literature in 1967, although they had been described previously. They are vascular malformations that begin as a soft, bluish-red, nonkeratotic lesion that grows and becomes hyperkeratotic and verrucous over time. Patient history often includes identification of a vascular birthmark that becomes wartlike or hyperkeratotic after trauma or infection. Although 95% are found on the lower extremity, the plantar surface of the foot is an uncommon location. Diagnosis must be made by histological analysis because the lesion may clinically resemble other lesions, most notably angiokeratoma. Histologically, verrucous hemangiomas are characterized by hyperkeratosis, papillomatosis, and epidermal acanthosis overlying a nondescript proliferation of capillaries and dilated veins and lymphatics. Extension into the subcutaneous reticular and adipose tissue is a distinguishing feature. Because of this extension, superficial treatments, including cryotherapy, laser therapy, and electrocautery, are uniformly followed by recurrence, making surgical excision the definitive treatment. Incomplete resection of the lesion may lead to recurrence, which makes preoperative imaging important. Postexcision laser treatment is also a beneficial option to reduce the risk of recurrence. In our patient, the accurate diagnosis was missed for nearly three decades, resulting in long-term pain and multiple failed treatments. Initially, during childhood, treatment with observation of the possible hemangioma was appropriate since most will involute and resolve between the ages of five and seven. In adolescence and young adulthood, initial treatments that focused on superficial measures (e.g., cryotherapy, callus debridement, and wart applications) were appropriate, but after repeated failures, advanced imaging was warranted. Close physical examination revealed a vascular appearance that suggested a more uncommon etiology. MRI revealed a vascular malformation with extension into the soft tissues and also identified margins for surgical removal. At the last follow-up, surgical excision had greatly decreased the pain; excision of the entire lesion most likely reduced the risk of recurrence. A high degree of clinical suspicion is necessary for diagnosing verrucous hemangioma, and it should be included in the differential diagnosis for long-standing hyperkeratotic nodular lesions of the lower extremity. Identification of the combination of a vascular and hyperkeratotic lesion with a histological specimen is crucial to diagnosis. Histology shows hyperkeratosis and epidermal acanthosis with extension into the subcutaneous tissue. Definitive treatment must include excision of the full lesion or there is risk of a high rate of recurrence.
Reference: Haskins SM, Shields NN. Verrucous hemangioma of the plantar surface of the foot: a case report. JBJS Case Connector. 2014 Jan 22;4(1):e10.
Plantar fibromatosis
Verrucous hemangioma
Malignant melanoma
Arteriovenous malformation
Squamous-cell carcinoma



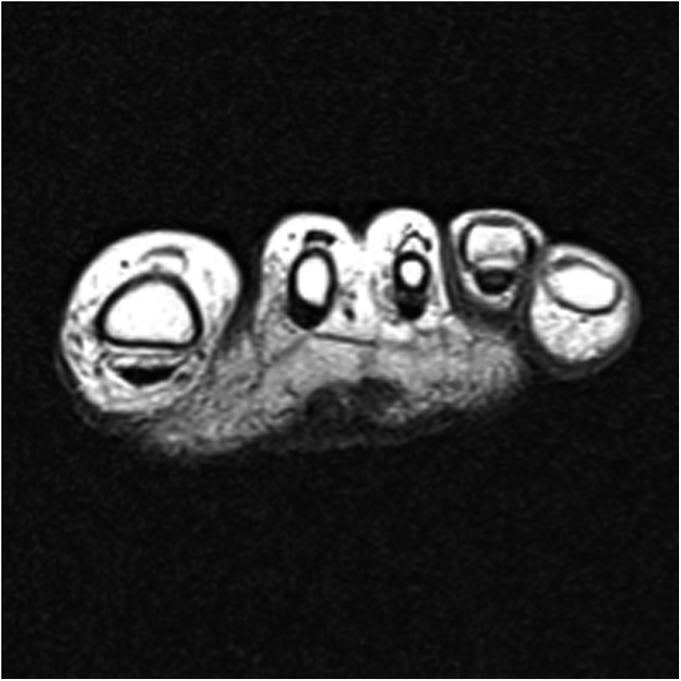
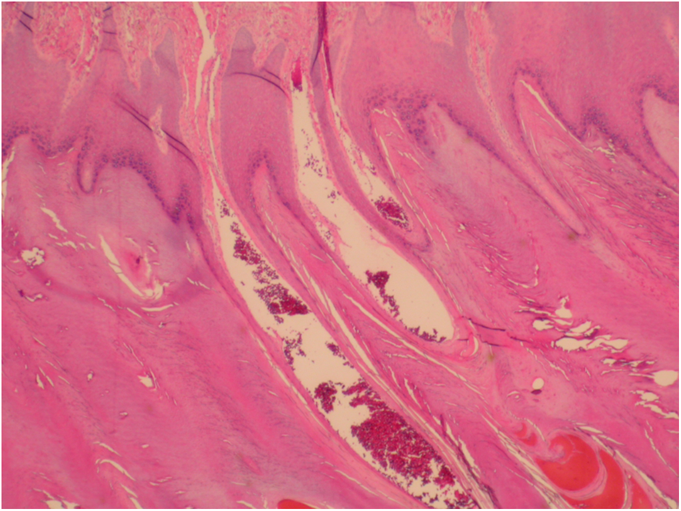
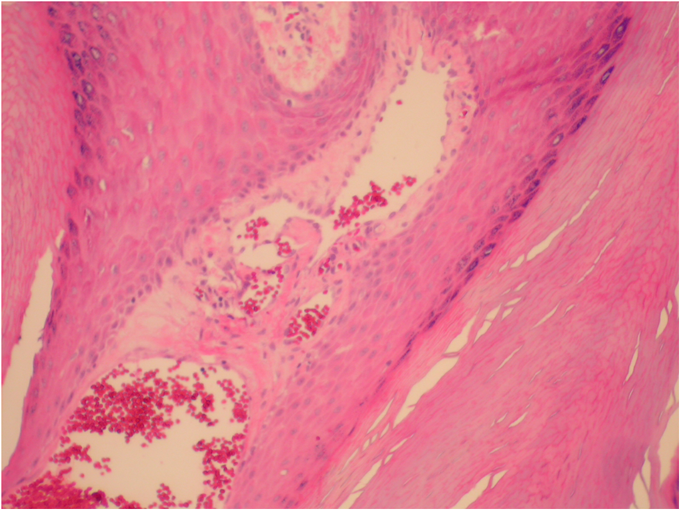

 Fig. 1
Fig. 1 Fig. 2-A
Fig. 2-A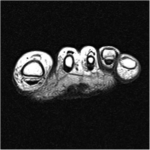 Fig. 2-B
Fig. 2-B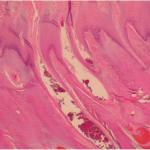 Fig. 3-A
Fig. 3-A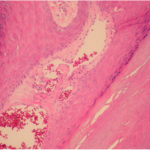 Fig. 3-B
Fig. 3-B Fig. 4
Fig. 4