A Thirty-seven-Year-Old Woman with a Chronic Wound on the Left Ring Finger
February 18, 2015
A thirty-seven-year-old woman presented with a chronic wound over the dorsum of the left ring finger. She related the initial symptoms to a laceration from a kitchen knife that had occurred more than seven months previously. The wound initially had been slow to heal and had been erythematous, and tender nodules eventually had developed dorsally. After initial dermatologic evaluation, the patient was treated with oral ciprofloxacin for four weeks without resolution. Subsequently, two local excisional biopsies of the cutaneous nodules were performed without success and with recurrence of the lesion. Microbiologic analysis of the biopsy specimens isolated a bacterial species with broad antimicrobial resistance to cefoxitin, cefmetazole, ciprofloxacin, doxycycline, erythromycin, and sulfamethoxazole. However, the pathogen was susceptible in vitro to clarithromycin. Consultation with an infectious disease specialist was obtained, and the patient was treated with clarithromycin for eight weeks. Despite this treatment, there was no resolution of the lesion. As a result, a surgical consultation was recommended. Upon evaluation in the hand surgery clinic, the patient was found to have diffuse cutaneous changes over the dorsal aspect of the left ring finger at the level of the proximal phalanx (Fig. 1-A). Wide excision of the lesion with irrigation and debridement of the local structures was recommended. Under general anesthesia, the lesion was excised with a wide margin along healthy tissue planes through the skin and subdermal tissue circumferentially (Fig. 1-B). The depth of the tissue excision was carried down to the epitenon of the extensor mechanism, with the goal of a complete en bloc lesion excision. The excised tissue was sent to the laboratory for histologic analysis and microbiologic cultures. Under loupe magnification, evaluation of the underlying structures demonstrated no involvement of the extensor mechanism or any remaining pathologic tissue at the skin margins. The dorsal defect measured approximately 10 × 18 mm and was covered with a synthetic skin graft (Integra LifeSciences, Plainsboro, New Jersey). Gentle active assisted range of motion of the digit was initiated under the supervision of a hand therapist on postoperative day three.
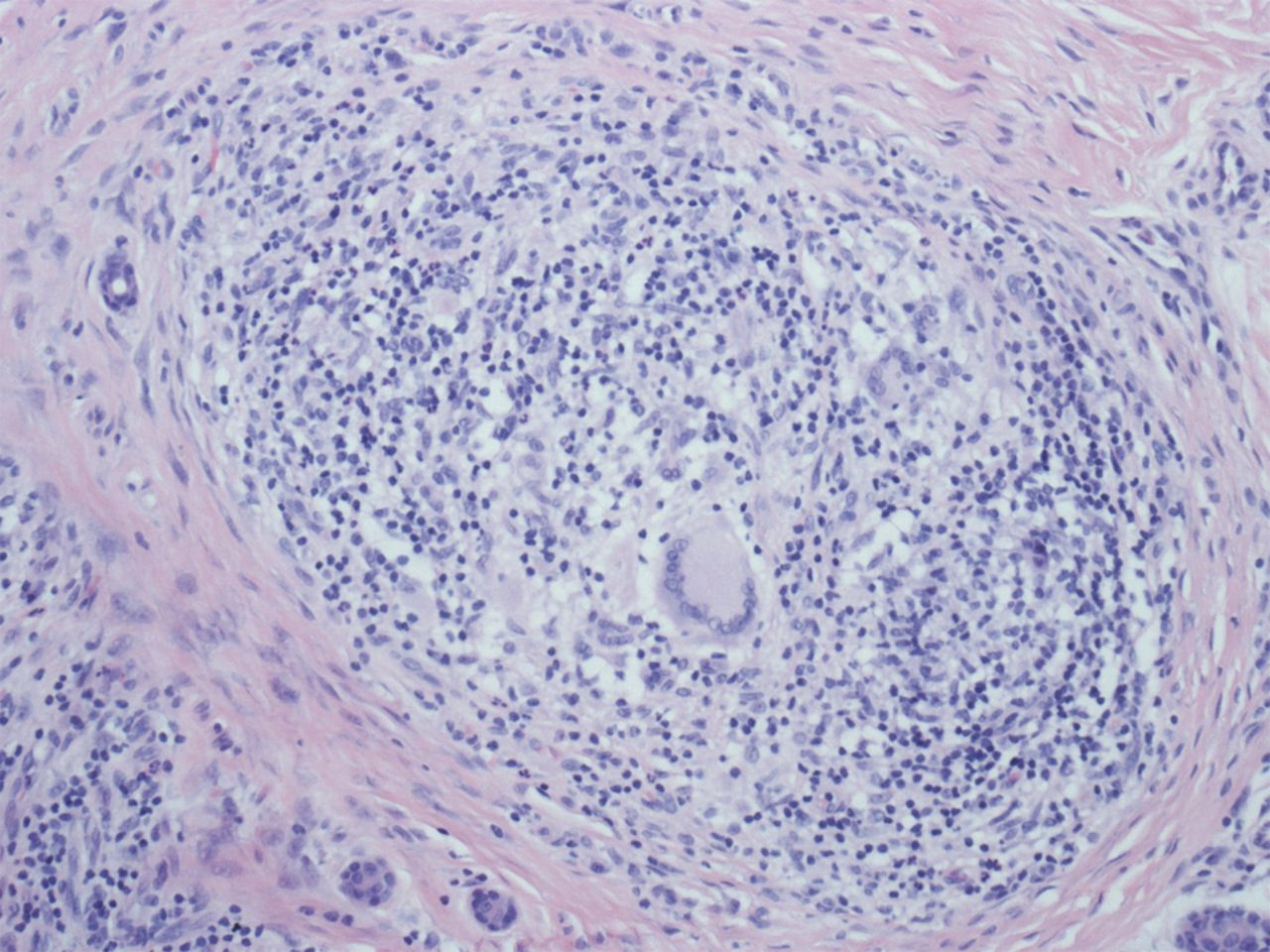
Histologic examination demonstrated granulomatous tissue consistent with a chronic Mycobacterium chelonae (M. chelonae) infection, and postirrigation and debridement cultures of the dorsal defect were negative (Fig. 2). Following three weeks of therapy, the patient returned to the operating room for repeat irrigation and debridement, removal of the synthetic graft, and coverage with a full-thickness skin graft (FTSG) harvested from the medial brachium. Active assisted range of motion was resumed immediately. Six weeks after placement of the FTSG, the patient demonstrated full digital range of motion, maturation of the skin graft, and no evidence of recurrent infection (Fig. 3). Based on the recommendations of the infectious disease specialist, the clarithromycin regimen was discontinued at three months after the initial debridement. Six months postoperatively, the patient reported no activity limitations, demonstrated full and nontender digital motion, and exhibited no evidence of recurrent infection.
Proceed to Discussion >>Reference: Wang ML, Vosbikian MM, Abboudi J, Beredjiklian PK. Treatment of a chronic multidrug-resistant cutaneous mycobacterium chelonae infection of the hand with wide debridement and skin-grafting: a case report. JBJS Case Connect. 2014 Nov 12;4(4):e102.
M. chelonae is a rapidly growing and nontuberculous Mycobacterium species that is associated with local environmental trauma and nosocomial infections. Ubiquitous to most local environments, M. chelonae has been isolated from soil, dust, and local water supplies. Previous studies investigating the exposure of patients with neutropenia to certain waterborne pathogens analyzed tap water samples obtained from the households of those patients and documented a 58.5% presence of M. chelonae in concentrations of 1 to 1000 colony-forming units (CFU)/500 mL. Other reports also have documented that nontuberculous Mycobacterium species can remain viable and proliferate in municipal water supplies as well as in distilled water and are resistant to chlorine and common disinfectants. A recent report of an M. chelonae outbreak that was associated with tattoo parlors identified the mixture of the ink with distilled water as the source of the infection, suggesting that a mycobacterium contaminant may remain viable in unopened stock bottles of tattoo ink. Our patient described accidentally cutting the dorsum of the nondominant ring finger with a kitchen knife at the sink, ultimately resulting in inadvertent inoculation. Studies have reported the emergence of M. chelonae strains resistant to multiple antibiotics (including clarithromycin) resulting in chronic disseminated cutaneous lesions with broad antimicrobial resistance. Prior works have suggested a link between biofilm formation and the virulence of rapidly growing Mycobacterium species such as M. chelonae. In our patient, the antibiotic resistance of this infectious organism necessitated a unique set of treatment considerations. Typically, infectious conditions that require surgical intervention rely on a two-pronged strategy to eradicate the infection, consisting of surgical debridement followed by antibiotic treatment. The goal of the surgical treatment is to decompress and debride areas sequestered from the bloodstream, such as joint spaces and tendon sheaths, in an effort to diminish the infectious load. The regimen of antibiotic therapy supplements this process via the eradication of residual bacterial load within the tissue. Previous reports on M. chelonae-associated hand infections have documented the involvement of the flexor sheath and the subsequent development of pyogenic flexor tenosynovitis. Mateo et al. described successful treatment with antibiotic therapy alone, suggesting that early diagnosis and medical treatment might obviate the need for surgical intervention. While such cases appear to exist in the literature on an individual basis, atypical mycobacterial infections of the flexor sheath are generally associated with a penetrating injury and respond to prompt surgical irrigation and debridement followed by parenteral antibiotic treatment. At present, documentation of the successful treatment of a chronic multidrug-resistant cutaneous M. chelonae infection of the hand remains sparse. We identified only one other case of cutaneous M. chelonae infection in the upper extremity involving the forearm and wrist, which was treated with in situ debridement. In this case report, we describe the successful treatment of a cutaneous M. chelonae lesion with wide debridement and the staged utilization of synthetic tissue-grafting, followed by full-thickness skin-grafting. With our patient, general anesthesia was selected to minimize the risk of local dissemination and hematological seeding, a possibility that could occur through the use of local anesthesia or regional blocks. Additionally, the finger lesion was excised with a wide excisional margin along uninvolved tissue planes. This technique permits complete en bloc excision and results in the creation of a margin of healthy soft tissue, minimizing the disturbance of the lesion and microdissemination of the infection. The coverage of the defect was staged with a synthetic skin graft, allowing surveillance of potential recurrence at the margins of the surgical site. We used a synthetic skin graft for the advantage of temporary soft-tissue coverage as well as immediate digital range of motion. In our patient, the synthetic graft was maintained for three weeks, allowing the formation of a neodermal layer over the dorsal aspect of the extensor mechanism, permitting preparation for definitive coverage. During this time period, intraoperative cultures and histological analysis were finalized for preoperative planning of the second stage. In the event of positive cultures after the initial surgery, repeat debridement and reapplication of a synthetic graft could have been performed until the cultures were negative. At the time of definitive soft-tissue coverage, the donor skin was harvested prior to working on the defect in order to minimize cross-contamination of the infection with the donor site. A medial brachial FTSG was used rather than a split-thickness skin graft because there was ample appropriately pigmented tissue of the correct depth from a well-vascularized area that afforded a simple harvest with minimal cosmetic effect. In addition, this tissue offered elasticity and durability and was more supple against tension and shear (dorsal apparatus, zone 4), allowing earlier aggressive digital motion under the direct supervision of a certified hand therapist.
Reference: Wang ML, Vosbikian MM, Abboudi J, Beredjiklian PK. Treatment of a chronic multidrug-resistant cutaneous mycobacterium chelonae infection of the hand with wide debridement and skin-grafting: a case report. JBJS Case Connect. 2014 Nov 12;4(4):e102.
Chronic Mycobacterium chelonae infection
Cutaneous lymphoma
Cutaneous myeloma
Cutaneous tuberculosis
Malignant basal cell carcinoma



 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 2
Fig. 2 Fig. 3
Fig. 3