A Thirty-six-Year-Old Male Triathlete with Six Months of Hip Pain
December 1, 2010
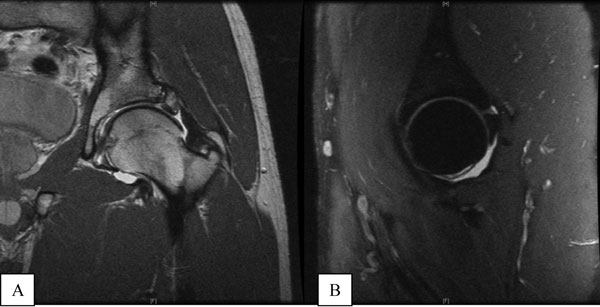
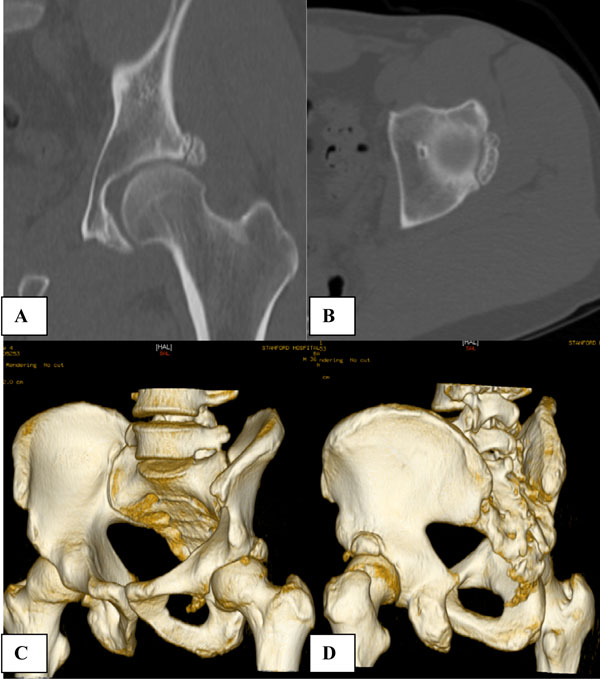
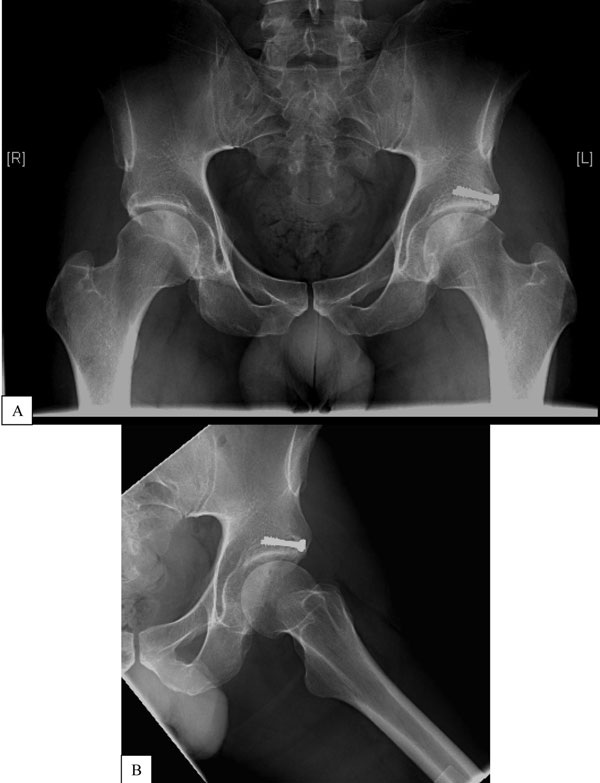
A thirty-six-year-old male surgeon and competitive triathlete presented with a six-month history of the insidious onset of dull left hip pain on the anterior aspect of the hip and in the groin. The pain was most bothersome when the hip was in hyperflexion, such as when in a tucked (aero) position while cycling. The discomfort had progressed to the point where it prevented him from engaging in triathlons, as running even two miles was too difficult due to pain. He had been evaluated by several physicians but had seen no improvement after six months of intermittent rest and physical therapy. Physical examination revealed crepitus during the labral stress test, and the results of impingement testing were negative. Hip flexion was to 140°, and extension and external rotation of the involved hip were equal to those in the asymptomatic hip. Internal rotation of the hip, with the knee in 90° of flexion, was 10° on the left and 15° on the right. The modified Harris hip score was 95. Radiographs showed osteophytosis of the femoral head and acetabular roof. There was a positive radiographic crossover or figure-of-eight sign, and the center-edge angle of Wiberg was 50° and 18° when measured lateral to and medial to the osseous fragment, respectively (Fig. 1). Magnetic resonance imaging showed a thickened capsule with anterior and posterior labral tears and an osseous protuberance at the lateral aspect of the femoral head-neck junction. The gap, which was filled with fibrous tissue and was associated with edema, demonstrated a pseudoarticulation with the adjacent acetabulum. The fragment contained labrum, articular cartilage, and bone (Fig. 2, A and B). The anterolateral osseous body measured 30 × 17 mm on a computed tomography scan (Fig. 3, A through D). A three-phase bone scan demonstrated no increased uptake.
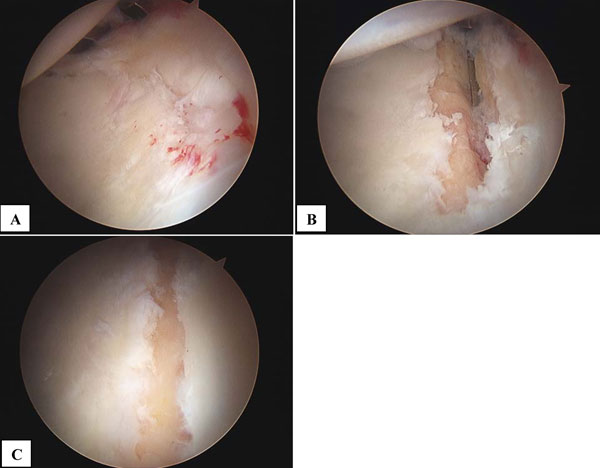
Given the patient's desire to return to competition, the negative results of the bone scan, and the failure of nonoperative treatment, we elected to perform an osteoplasty of the femoral head-neck region to address the femoroacetabular impingement and to reduce further stress to the anterolateral aspect of the acetabulum. In addition, we recommended arthroscopic reduction and internal fixation of this acetabular nonunion. After the level of anesthesia was confirmed as being adequate, the patient was positioned on the fracture table with a well-padded perineal post lateralized toward the left hip. The right hip was abducted 60°. Standard anterolateral, posterolateral, and anterior portals were established. There was partial tearing of the anterior portion of the labrum. The demarcation between the normal cartilage and the osseous fragment could be identified from the chondromalacia on the acetabular side of this pseudoarticulation and the mobility of the osseous fragment upon probing (Fig. 4, A). A probe revealed a partial anterior labral tear, which was debrided with a radiofrequency device, and some mild labral-chondral separation was noted posteriorly. A probe was inserted through the anterior portal and, with use of the anterolateral and posterolateral portals for viewing, the osseous fragment was found to be mobile. There was an area of full-thickness articular cartilage loss at the edge of the acetabulum, adjacent to the fracture fragment (which was covered with normal articular cartilage). While the procedure was viewed with use of a 70° lens through the posterolateral portal, a chondroplasty of the damaged articular cartilage of the acetabulum was performed. After chondroplasty, the area of chondral damage measured 4 mm wide and 25 mm in length (Fig. 4, B). It was believed that doing a formal acetabuloplasty of the lateral portion of the rim was not necessary because the articular cartilage and labrum were intact on this portion of the rim. Furthermore, removal of the pseudarthrosis would medialize the rim, equivalent to a 1 to 2-mm rim resection, functionally achieving a reduction in the acetabular overcoverage. Capsulotomies were performed to enlarge the anterior and anterolateral portals to help mobilize the osseous fragment and to debride the pseudarthrosis. With use of a combination of curets and the microfracture awl, the area of the pseudoarticulation was delineated and debrided of fibrous tissue. Traction was then removed. An accessory anterolateral portal was then made and a partial capsulectomy was performed. The cam lesion was clearly identified, and an osteoplasty (i.e., a cheilectomy) was performed at the femoral head-neck junction while the procedures were visualized arthroscopically with a 30° lens and with fluoroscopic assistance. Visualization from the peripheral compartment was achieved, and two guidewires for the 4.5-mm cannulated cancellous screws were then introduced percutaneously and placed through the fracture fragment and into the acetabulum unicortically. The guidewires were angled posteriorly in order to protect the external iliac vessels, but they were not angled so far as to threaten the obturator vasculature. Next, traction was reapplied to the hip to confirm that the wires did not penetrate the joint and that the fracture remained reduced. With use of arthroscopy and fluoroscopy, the reduction was confirmed to be excellent. Next, a cannulated drill was used to drill over the guidewires and two 4.5-mm partially threaded cannulated cancellous screws (24 mm and 26 mm in length) were placed unicortically, with excellent purchase, under arthroscopic visualization. The guidewires were then removed after the screws were fully seated. Arthroscopic and fluoroscopic visualization again confirmed near-anatomic reduction (Figs. 4, C and 5). Dynamic assessment of impingement was then carried out arthroscopically by moving the hip through its range of motion to confirm that there was no residual impingement. Reduction of the fracture was confirmed on postoperative radiographs, which revealed a center-edge angle of 38°. The patient was discharged on the day of surgery. Only touch-down weight-bearing was permitted for six weeks, shortly after which the patient was allowed to advance to full weight-bearing. Hip range of motion was encouraged immediately following surgery, and light strengthening exercises were progressively introduced. The patient performed light stationary cycling immediately after surgery and, at three weeks, began swimming freestyle. At three months after surgery, radiographic imaging demonstrated healing of the acetabular rim fragment without loss of fixation or reduction, and the patient was given permission to resume running. By four months after surgery, he was running six miles a day at a pace of seven minutes per mile. At the one-year follow-up, the patient was swimming three to four miles per week, biking forty to sixty miles per week, and running fifteen to twenty miles per week without hip pain. The modified Harris hip score had improved to 100. The one-year follow-up radiograph showed osseous union of the acetabular fragment with no change in hardware position or alignment (Fig. 6, A and B).
Proceed to Discussion >>Reference: Epstein NJ, Safran MR. Stress fracture of the acetabular rim: arthroscopic reduction and internal fixation. A case report. J Bone Joint Surg Am. 2009;91:1480-6.
This high-demand athlete with combined-type femoroacetabular impingement (predominantly cam type) sustained a stress fracture at the anterolateral aspect of the acetabular rim and a subsequent fibrous nonunion. The majority of previous reports of lateral acetabular osseous fragments have been in patients with dysplastic hips. While the acetabular rim is exposed to more shear stress in patients with frank hip dysplasia than in patients with a normal hip, active patients with femoroacetabular impingement and a retroverted acetabulum may also be at risk for such fractures. On the basis of the results reported in the one prior large series, such osseous fragments may occur with a prevalence of 3.6% in patients with femoroacetabular impingement. The true prevalence in patients with cam-type femoroacetabular impingement is unknown, but we agree with Martinez et al. that acetabular retroversion in a highly active patient with cam-type femoroacetabular impingement should be considered a risk factor for the development of a stress fracture of the acetabular rim, as these findings have also been identified by the senior author (M.R.S.) in seven other patients since 1996. The surgical treatment of these patients has consisted of addressing the femoroacetabular impingement and resecting or debriding the acetabular fragment. In the senior author's series of seven active patients with femoroacetabular impingement and stress fractures of the anterolateral portion of the acetabular rim, four patients underwent femoral head-neck osteochondroplasty and fragment removal, one patient underwent periacetabular osteotomy, and two patients had spontaneous fusion of the fragments after nonoperative treatment. In the case of the patient in the current case report, it was unlikely that the fragment would have fused spontaneously, considering the negative results of the bone scan. Furthermore, preoperative assessment of the anteroposterior radiographs of the pelvis demonstrated that removal of the fragment would have resulted in inadequate femoral head coverage (a center-edge angle of 18°). On the basis of the arthroscopic findings, the edge of the acetabular articular cartilage was already beginning to wear, as the hip was essentially functioning without the fragment. This finding suggests that the hip was undergoing wear due to edge-loading, similar to what would be expected to occur in a hip with biomechanical decompensation due to dysplasia. We therefore performed a femoral head-neck osteoplasty to treat the underlying femoroacetabular impingement, and the anterolateral acetabular fragment nonunion was treated with arthroscopic debridement and then reduction and internal fixation with two unicortical cannulated cancellous screws. It was thought that elimination of the impingement (by restoring the femoral head-neck offset) and internal fixation of the fragment would alleviate the symptoms, allow for osseous union without producing hip dysplasia, and possibly delay further degeneration of the hip. Following reduction, the center-edge angle measured 38° as compared with 50° preoperatively. Patients who present with cam-type femoroacetabular impingement, acetabular retroversion, and an acetabular rim fracture may be treated by several different methods, with the best option yet to be determined. Certainly, excision of the fragment, open or arthroscopically, is an option, provided that excision of the fragment does not compromise acetabular coverage of the femoral head. If the fracture is displaced and there is evidence of nonunion, or if fragment removal would compromise coverage of the femoral head, then internal fixation may be warranted. While it is not known whether internal fixation of the fragment may delay or prevent progressive degenerative change, maintaining the fragment in order to increase the hip articular contact area may be an alternative to removing the fragment if removal would compromise acetabular coverage of the femoral head. Given this patient's presentation, a periacetabular osteotomy was also an alternative. This would have addressed the femoroacetabular impingement, the femoral head coverage, and the acetabular retroversion. However, periacetabular osteotomy can be associated with substantial morbidity, including a large incision, appreciable blood loss, the need for dislocation of the hip, a lengthy postoperative hospitalization, and a potentially prolonged period of limited weight-bearing and rehabilitation. In addition, on the basis of the experience of surgeons who regularly perform this operation, it is unlikely that a periacetabular osteotomy would have resulted in this patient being able to return to his preoperative level of competition. However, had arthroscopic reduction and internal fixation failed, a periacetabular osteotomy could still have been performed. Arthroscopic intervention does have some limitations. We were able to address the femoroacetabular impingement, and, by debriding the nonunion and shortening the acetabulum, we were also able to decrease the anterolateral overcoverage as evidenced by the center-edge angle of 38°. However, arthroscopic intervention does not address the acetabular retroversion, and the question remains whether degeneration of the hip will develop over time. In our relatively short period of follow-up, this method of arthroscopic treatment has been shown to provide an alternative to open excision or, in this case, periacetabular osteotomy. It maintains adequate femoral head coverage anterolaterally, is less invasive than a periacetabular osteotomy, and does not compromise future treatment options. More comprehensive studies are needed, but the case of our patient is an example of one application of arthroscopic reduction and internal fixation. This novel method may also be useful in the management of smaller acetabular fractures and stress fractures of the acetabular rim.
Reference: Epstein NJ, Safran MR. Stress fracture of the acetabular rim: arthroscopic reduction and internal fixation. A case report. J Bone Joint Surg Am. 2009;91:1480-6.
Calcification of torn labrum
Fracture of the acetabular rim
Heterotopic bone formation
Loose body from femoral head


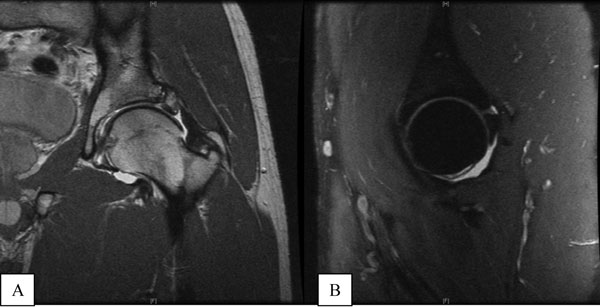
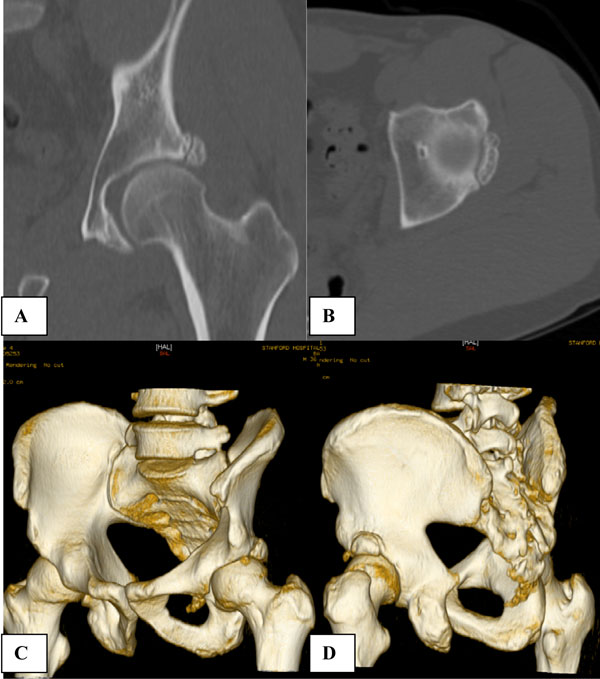
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 1
Fig. 1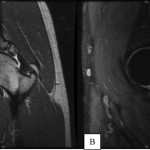 Fig. 2
Fig. 2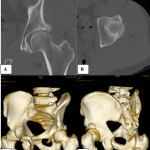 Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5
Fig. 5 Fig. 6
Fig. 6