A Sixty-nine-Year-Old Man with End-Stage Osteoarthritis
November 17, 2010
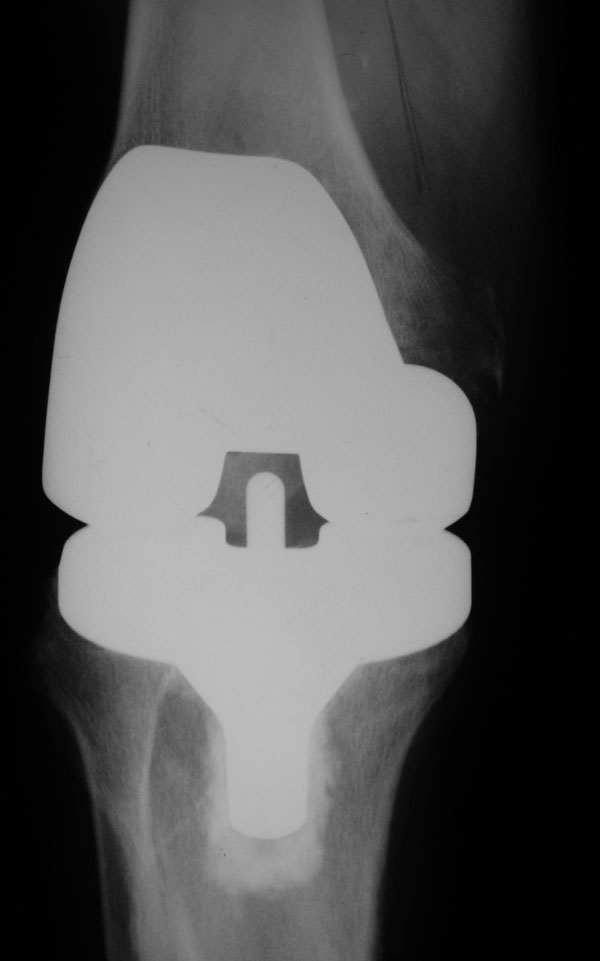
A sixty-nine-year-old man underwent a right total knee arthroplasty (TKA) with cement and with a posterior stabilized mobile-bearing prosthesis (PFC Sigma Rotating Platform; DePuy, Johnson and Johnson, Warsaw, Indiana) for end-stage osteoarthritis. A routine pathology report of a random sampling of the bone cut from the knee during surgery showed cartilage-capped bone with degenerative change, osteoarthritis, and no signs of any neoplastic process. The postoperative course was complicated by hypoxia, pulmonary embolus, atrial fibrillation, and myocardial infarction. The patient was also diagnosed as having Guillain-Barré syndrome in the month after surgery. All of these problems slowed his recovery; however, the patient reported that he was free of the pain in the right knee for several months after surgery. Nine months after surgery, the patient presented to our office for a second opinion for severe pain in the right knee. The knee had done well until three months before when the patient had a focal tender spot develop on the medial aspect of the distal end of the femur. He reported no history of trauma. By the time he presented to our office, the knee pain had become so severe that he required a wheelchair. The pain was constant and worsened with motion and with weight-bearing. Physical examination of the right knee at this time revealed a range of motion from 20° to 80°, good ligamentous stability, and no extension lag. There was diffuse tenderness to palpation localized to the medial femoral condyle with mild warmth. Serologic laboratory tests showed slight elevation of both the C-reactive protein level (11.6 mg/L; reference range, 0 to 10 mg/L) and erythrocyte sedimentation rate (28 mm/h; reference value, <20 mm/h). The white blood-cell count was slightly elevated as well at 11.6 × 109/L. To rule out infection, the knee was aspirated and 20 mL of clear fluid was obtained. A cell count of the synovial fluid showed a white blood-cell count of 17/mm3, with 12% polymorphonucleocytes. No crystals were identified, and there was no growth on either aerobic or anaerobic cultures. We did not recognize any notable findings on routine radiographs of the patient made at the time of his presentation to our office (Fig. 1). However, in hindsight, a lytic lesion can be seen in the distal end of the femur medial to the prosthesis. A bone scan from prior to presentation in our office showed slight increased uptake in the medial femoral condyle.
Three days later, the patient presented to the emergency room with back pain, chest pain, and increasing knee pain. A computed tomography scan of the chest showed a mass in the right upper lobe of the lung, and a computed tomography scan of the knee showed a destructive, lytic lesion behind the femoral prosthesis in the medial femoral condyle (Fig. 2). The patient was admitted to the intensive care unit and quickly worsened with multisystem organ failure, and he died one week into his hospital stay. On postmortem autopsy, the cause of death was found to be respiratory failure, myocardial infarction, and metastatic carcinoma. Pathologic identification of the primary tumor was cholangiocarcinoma, and additional metastatic lesions were identified in the liver and spine. At autopsy, we assisted the pathologist in the dissection of the knee and discovered a lesion in the medial aspect of the distal end of the femur (Fig. 3). Histologic examination of this lesion demonstrated metastatic cholangiocarcinoma.
Proceed to Discussion >>Reference: Fehring K, Hamilton W. Metastatic carcinoma as an unusual cause of knee pain after total knee arthroplasty. A case report. J Bone Joint Surg Am. 2009;91:693-5.
To our knowledge, this is the first report of a patient with metastatic disease as the cause of pain around a total knee replacement. Primary malignant neoplasms have been described in association with total joint arthroplasty. Cases of patients with periprosthetic non-Hodgkin lymphoma, bronchogenic carcinoma, gastric carcinoma, and squamous cell carcinoma of the lung have been reported. All of these previously reported cases have involved total hip implants. Metastatic disease is the most common destructive bone lesion in the older patient and should be considered first when a destructive bone lesion is encountered. The most common carcinomas to metastasize to bone are breast, lung, prostate, kidney, and thyroid. The most common locations to find the metastases are in the spine, pelvis, ribs, and in the upper and lower limbs proximal to the elbow and knee. Early identification of metastatic bone lesions can lead to increased patient survival with the possibility of surgical resection or radiation therapy. Multiple possible causes of a painful total knee replacement have been reported previously. Surgeons evaluating these patients should consider all of the possible causes, and the use of an algorithm is helpful to avoid overlooking potential diagnoses. In this case, the definitive diagnosis was overlooked by several experienced arthroplasty surgeons, most likely because it is rarely, if ever, found on the list of potential causes of a painful total knee replacement. It was not recognized at the time of the index surgery, either because it was not present or because the lesion was deep to the femoral bone cuts and was not visible. At the time of our initial evaluation of the patient, the severity and pattern of the pain did not fit any diagnosis particularly well. We were pursuing infection, implant loosening, andperiprosthetic stress fracture as the main diagnoses when he presented with obvious metastatic disease. In hindsight, review of the history, imaging studies, and autopsy findings made this diagnosis clear. In light of the case of our patient, we believe that metastatic disease should be added to the list of potential causes of knee pain after TKA. This diagnosis should especially be considered in a patient with a known primary malignant lesion. Even in this setting, the more common causes of pain after TKA are more likely, but the rare possibility of metastatic disease should be in the differential diagnosis. Both bone scans and computed tomography scans helped to better identify the lesion in our patient and are recommended if this diagnosis is considered. Because this patient died in such a short time frame, we were unable to offer treatment options and therefore cannot provide recommendations on potential treatment options in this scenario.
Reference: Fehring K, Hamilton W. Metastatic carcinoma as an unusual cause of knee pain after total knee arthroplasty. A case report. J Bone Joint Surg Am. 2009;91:693-5.
Stress fracture of medial femoral cortex
Subacute periprosthetic infection
Metastatic carcinoma
Osteolysis from loose TKA implant


 Fig. 1
Fig. 1 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3