A Twenty-six-Year-Old Man with Right Shoulder Pain
April 3, 2013
A twenty-six-year-old man presented with a one-month history of intermittent pain and a limited range of motion of the right shoulder following a stretching injury at work when he tried to grasp the handrail of a ladder before falling off of it. An anti-inflammatory agent (tiaprofenic acid) was given on the third day after the injury, and this treatment was discontinued two weeks later because pain relief had been achieved. However, the pain returned soon thereafter. The patient stated that he had no systemic symptoms, medical history of hyperuricemia, or prior episodes of acute arthritis. Except for the problems with the right, involved shoulder, the findings of the general clinical examination were unremarkable. Physical examination of the right shoulder revealed substantially decreased active ranges of motion in forward flexion (30°), extension (10°), and abduction (30°) in comparison with the ranges on the unaffected side (180° of forward flexion, 45° of extension, and 150° of abduction). The passive ranges of motion of the right shoulder were also decreased in forward flexion (75°), extension (30°), and abduction (90°). The patient had a painful arc on resisted abduction between 70° and 120°, suggestive of rotator cuff tendinitis. Internal rotation (90°) and external rotation (90°) of the right shoulder were normal. A radiograph of the right shoulder demonstrated a faint amorphous opacity above the humeral head (Fig. 1). Magnetic resonance imaging was performed with a 1.5-T magnetic resonance imaging unit (MAGNETOM Sonata; Siemens Medical Solutions, Erlangen, Germany) with use of a surface coil conforming to the curved shoulder girdle. Spin-echo T1-weighted, fast spin-echo T2-weighted, and gradient-echo T2*-weighted images were obtained in the oblique coronal plane parallel to the supraspinatus tendon. The swollen supraspinatus tendon revealed intrasubstance areas of high signal intensity on T2-weighted and T2*-weighted images with an amorphous deposit of low signal intensity on the articular side on all magnetic resonance imaging sequences, which was consistent with the suspicion of calcific tendinosis (Figs. 2-A, 2-B, and 2-C). Abnormal effusion of high signal intensity was present in the subdeltoid bursa on T2-weighted and T2*-weighted images (Figs. 2-B and 2-C). With the patient under general anesthesia, an open subacromial decompression (acromioplasty) was performed for removal of the abnormal deposit by dissection and débridement. The intraoperative findings revealed granular deposits on the articular side of the supraspinatus tendon when it was incised longitudinally (Fig. 3). Histological examination of the tissue specimen removed at surgery was carried out (Fig. 4).
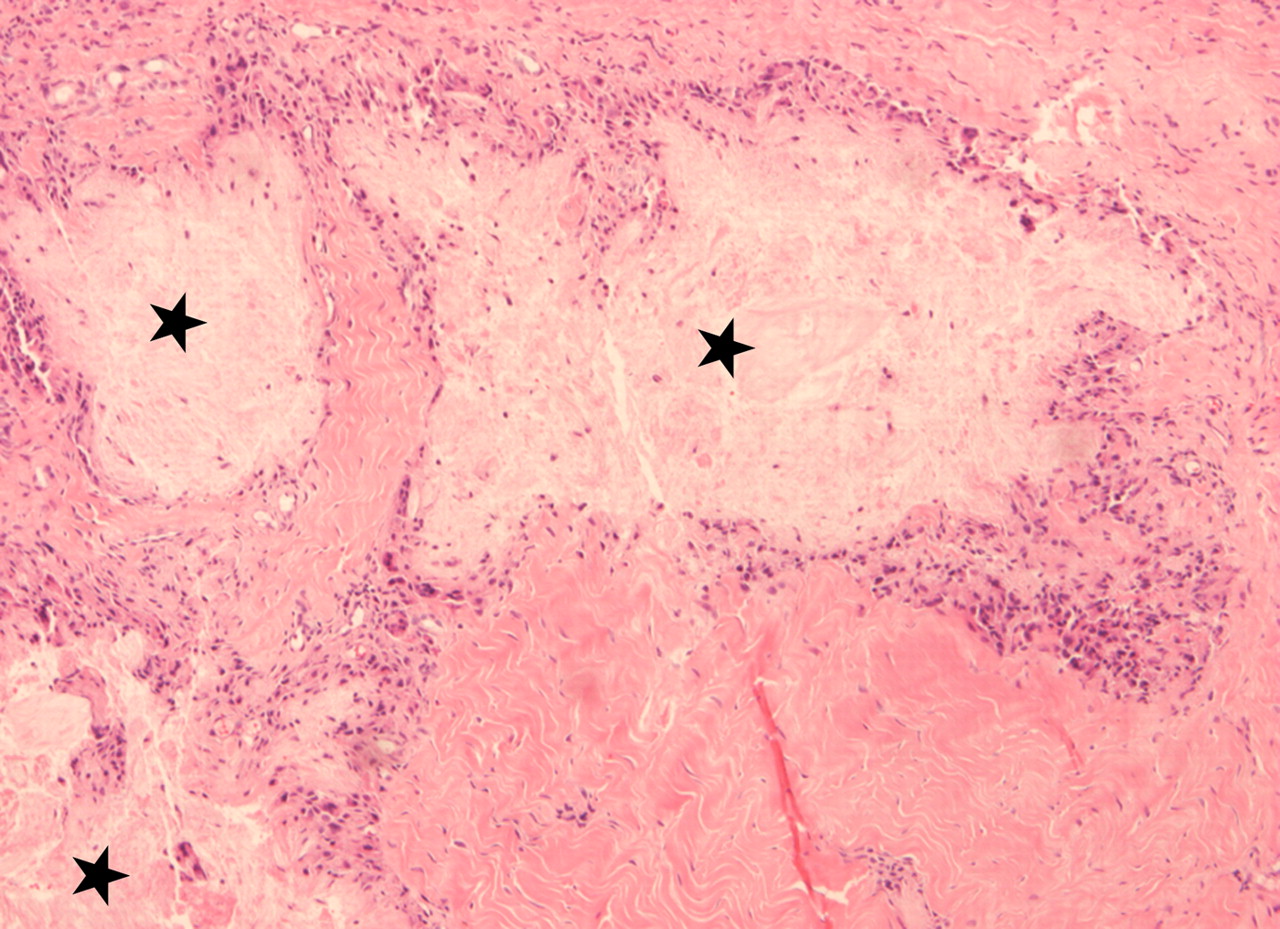
Histology demonstrated amorphous tophaceous deposits surrounded by granulomatous infiltrates consisting of multinucleated giant cells and histiocytes (Fig. 4). These intraoperative and histopathologic results confirmed the diagnosis of tophaceous gout of the rotator cuff. There were no postoperative complications. The serum level of uric acid rose to a high of 11.7 mg/dL (695.9 µmol/L) (normal, <8.3 mg/dL [<493.7 µmol/L]) after the surgery. The patient was subsequently treated with colchicine and allopurinol. At the time of the one-year follow-up after treatment, the patient had a complete pain-free range of motion of the involved shoulder.
Proceed to Discussion >>Reference: Chang CH, Lu CH, Yu CW, Wu MZ, Hsu CY, Shih TT. Tophaceous gout of the rotator cuff. A case report. J Bone Joint Surg Am. 2008 Jan;90(1):178-82.
To our knowledge, only one case of tophaceous gout involving the rotator cuff has been reported in the English-language literature. In this previous report, a forty-eight-year-old man presented with strongly positive signs of rotator cuff tendinitis, and the findings at arthroscopy revealed tophaceous deposits in both the supraspinatus and the subscapularis tendon. Magnetic resonance imaging had been performed before arthroscopy, and the description of the findings included mention of only some supraspinatus tendinitis, without demonstration of the tophaceous deposits. However, no magnetic resonance images were provided in that case report. Magnetic resonance imaging features of tophaceous gout, mainly in the peripheral joints and spine, have been described in the past. The gouty tophi have homogeneous intermediate and occasionally low signal intensity on T1-weighted images. The reported appearances of the gouty tophi on T2-weighted images have varied from homogeneous or heterogeneous high signal intensity to low signal intensity. The high signal intensity on T2-weighted images may result from the high protein content in the amorphous center, an increase in water content, or relative homogeneity of local magnetic fields within the tophus. The low signal intensity on T2-weighted images may be related to areas of calcification, mature fibrous tissue and urate crystals, immobile protons, or hemosiderin deposition in the tophus. Homogeneous intermediate signal intensity on T1-weighted images and heterogeneous intermediate-to-low signal intensity on T2-weighted images have been reported to be the most common pattern. The magnetic resonance imaging findings in the shoulder of our patient were consistent with those previously reported for other joints in the literature. Reported patterns of enhancement of the gouty tophi after intravenous administration of gadopentetate dimeglumine have varied from homogeneous enhancement to heterogeneous peripheral enhancement. The former may result from vascularized reactive tissue in the tophus, and the latter may reflect granulation tissue surrounding the tophus. However, gadolinium-enhanced magnetic resonance imaging was not performed for our patient because the routine protocol for rotator cuff tendinitis did not include contrast-enhanced studies. The imaging findings illustrated here are not pathognomonic of tophaceous gout. For example, the amorphous deposit of low signal intensity in the rotator cuff tendon on all magnetic resonance imaging sequences with hyperintense perifocal edema and subdeltoid effusion on T2 and T2*-weighted images initially observed in this case suggested the diagnosis of calcified tendinosis. It has been reported that the deposits of calcium hydroxyapatite are mainly located in the midportion of the tendon or under its acromial (bursal) surface. In the mechanical phase of calcific tendinosis, the enlarging calcium deposits may develop a subbursal or intrabursal rupture, resulting in calcific bursitis and pain. However, the tophaceous deposit seen in our patient was on the articular side of the supraspinatus tendon, which may be related to different local tissue changes and perhaps could make it distinguishable from the commonly encountered calcific tendinosis. In addition to calcific tendinosis, other conditions may have imaging findings similar to those of tophaceous gout as depicted here, and those conditions should also be considered in the differential diagnosis. They include dialysis-related amyloid arthropathy, pigmented villonodular synovitis, and other crystal-deposition arthropathies such as calcium pyrophosphate dihydrate crystal deposition disease. The clinical information, laboratory data, and characteristic imaging features may help the examiner to reach the correct diagnosis. Because of the rarity of the condition, the preoperative diagnosis of gouty tophi involving the rotator cuff is difficult, particularly in the absence of known hyperuricemia or prior episodes of acute gouty arthritis. Percutaneous aspiration and/or biopsy or surgical decompression would be necessary for diagnosis and management of some equivocal cases with shoulder symptoms. In conclusion, this rare case should remind the orthopaedic surgeon and radiologist to consider tophaceous gout in the differential diagnosis of shoulder impingement when abnormal deposits with a magnetic resonance imaging pattern mimicking calcific tendinosis are present in the rotator cuff.
Reference: Chang CH, Lu CH, Yu CW, Wu MZ, Hsu CY, Shih TT. Tophaceous gout of the rotator cuff. A case report. J Bone Joint Surg Am. 2008 Jan;90(1):178-82.
Gouty arthritis
Pseudogout
Calcific tendinitis
Rheumatoid arthritis


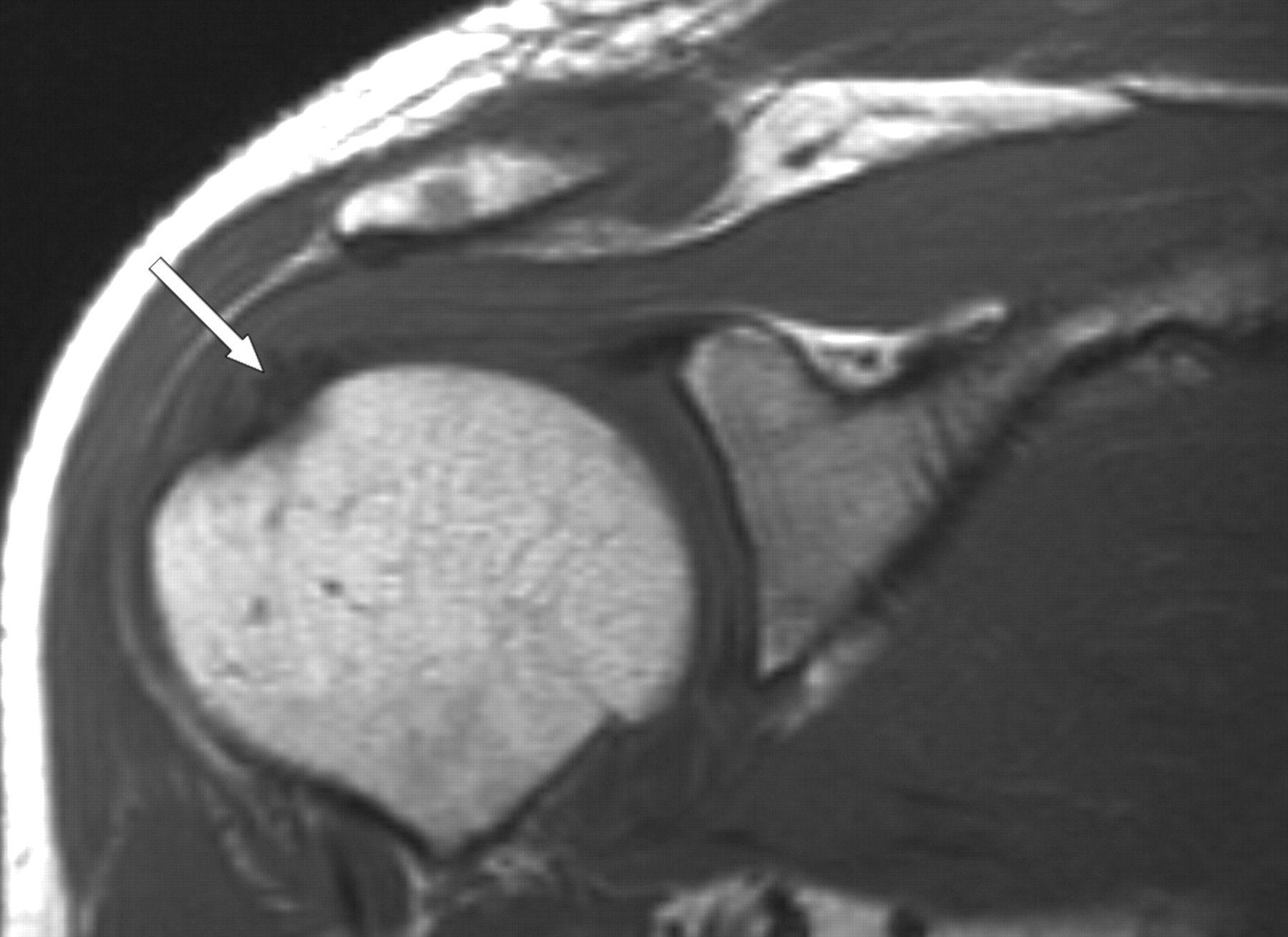
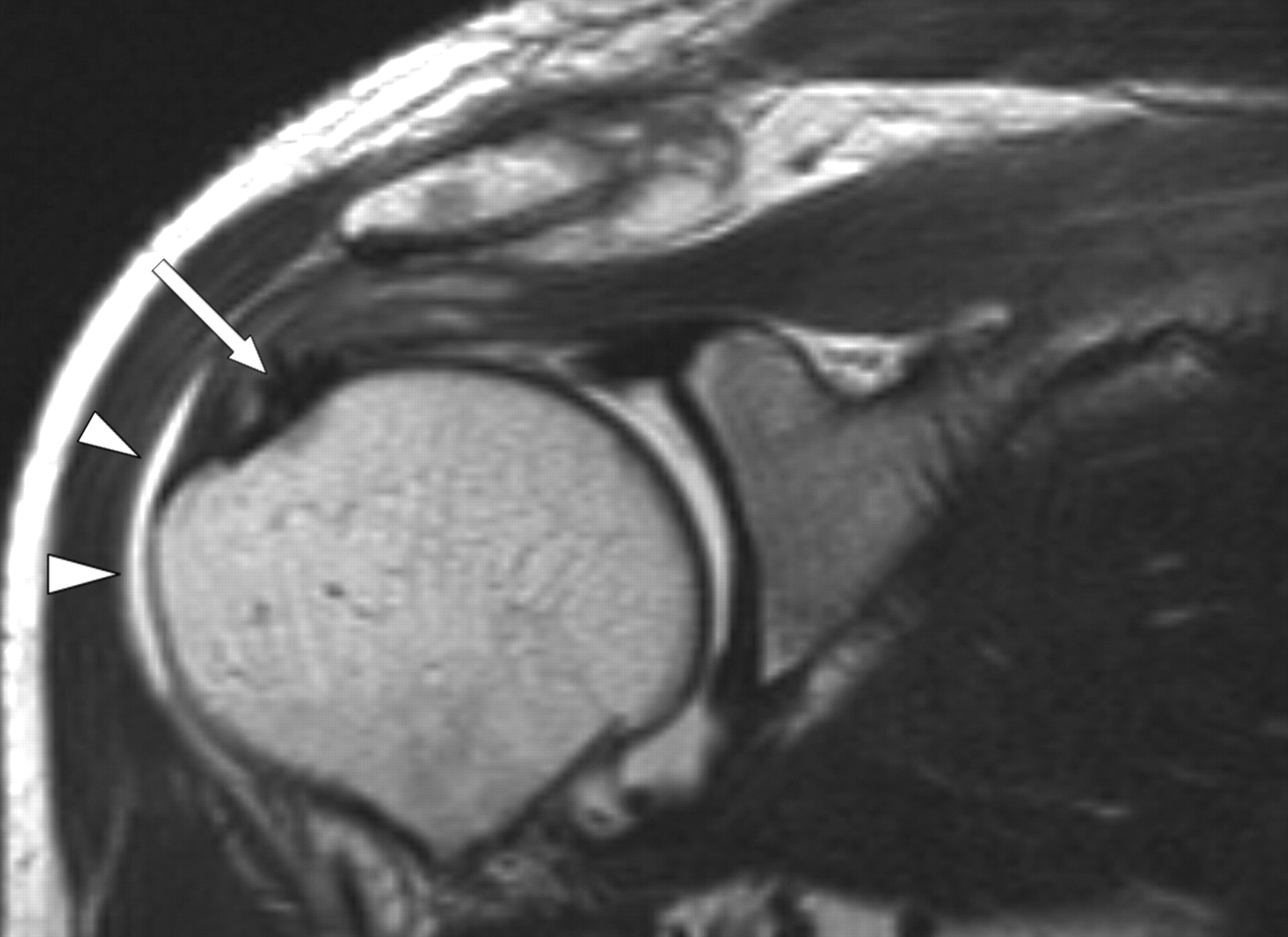
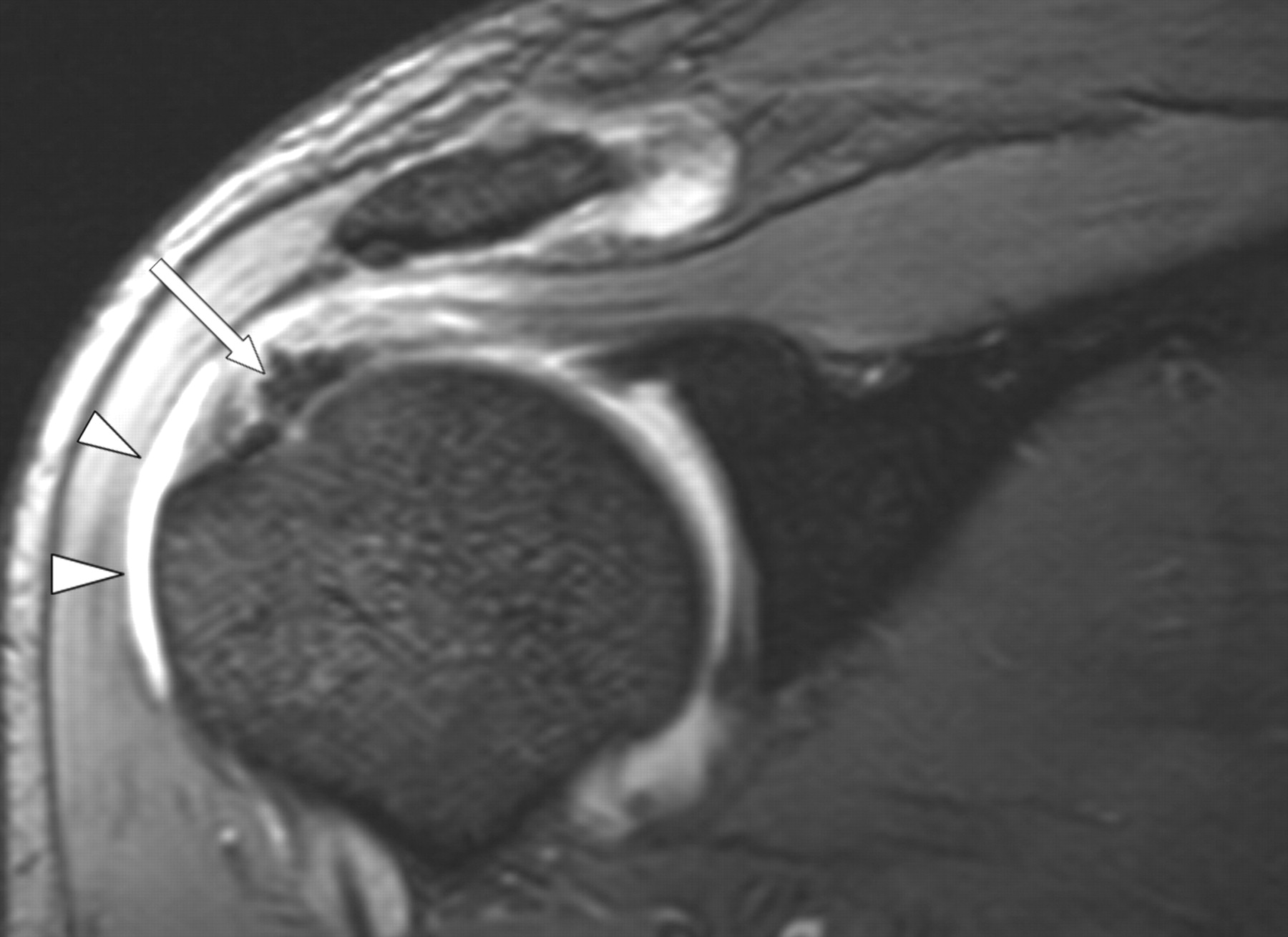
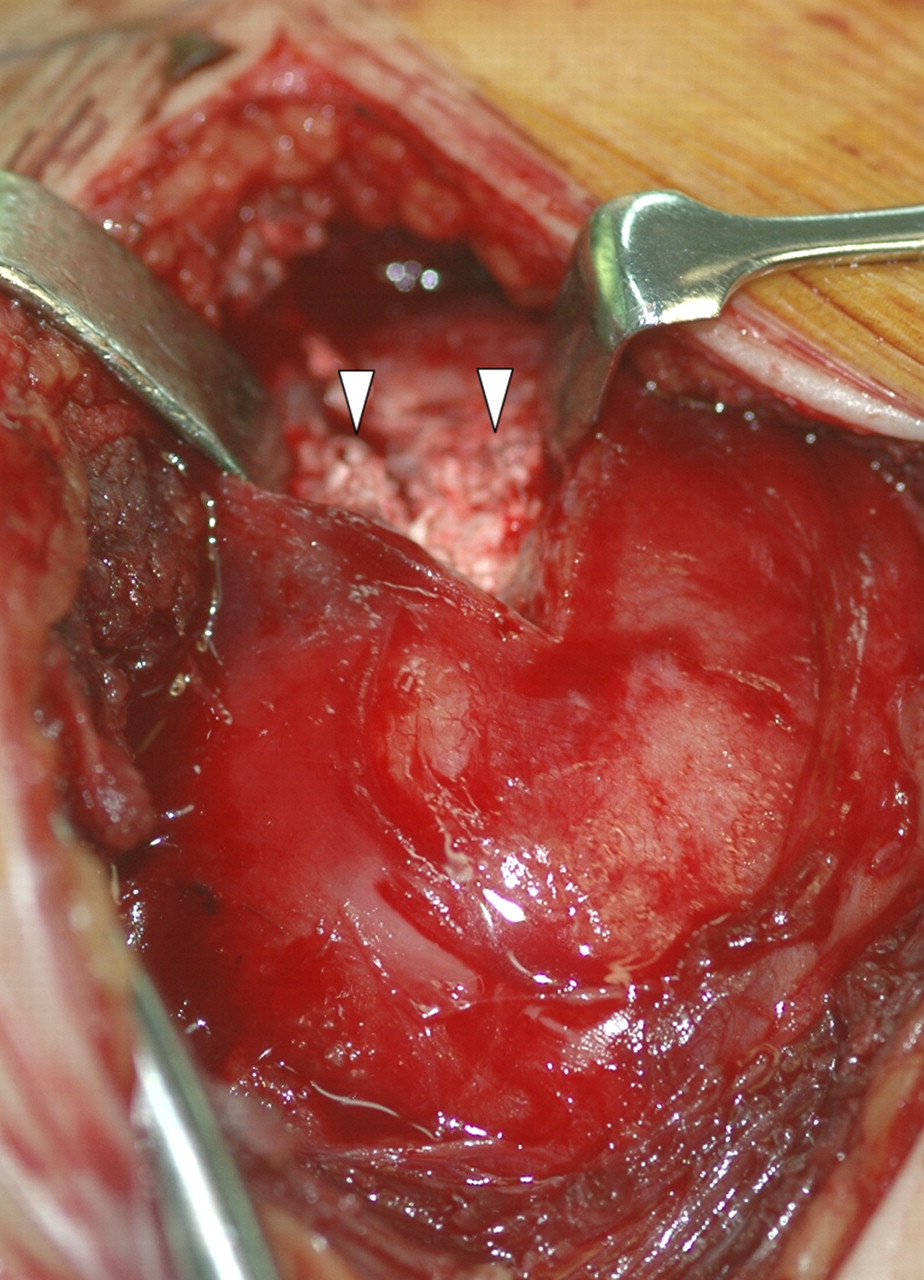
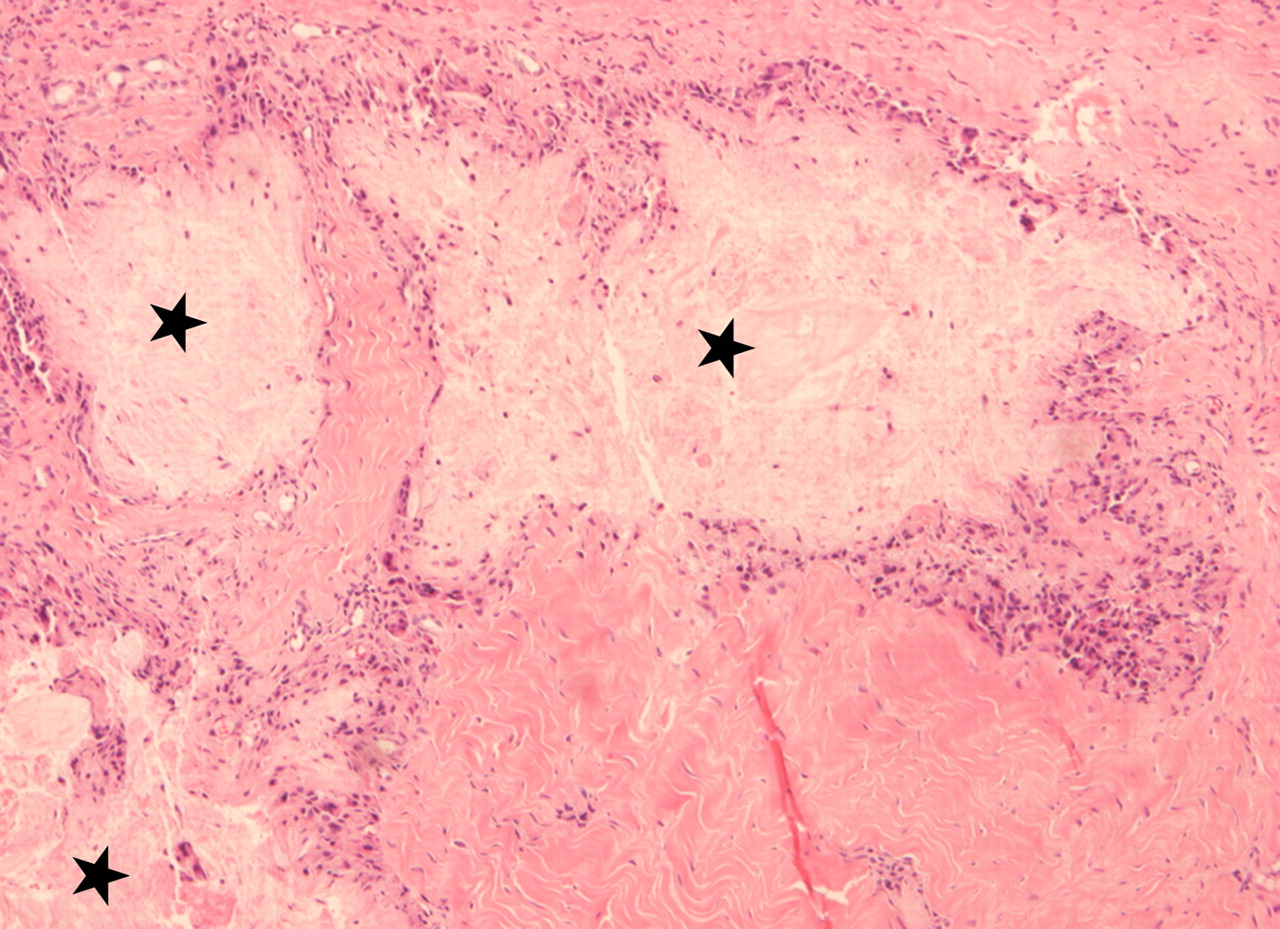
 Fig. 1
Fig. 1 Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B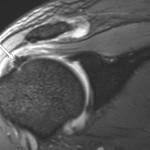 Fig. 2-C
Fig. 2-C Fig. 3
Fig. 3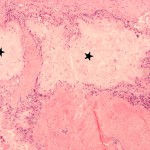 Fig. 4
Fig. 4 Fig. 4
Fig. 4