A Thirty-seven-Year-Old Man with Left Elbow Contracture
April 17, 2013
A thirty-seven-year-old man presented with limitation of motion of the left, nondominant elbow. He reported that pain and limited elbow motion had developed after he played a game of squash five years previously. There was no history of elbow trauma or infection. The pain had decreased with time, but limitation of elbow motion had continued to increase and had resulted in a fixed flexion deformity of 90° two years before the patient presented to us. Physical examination revealed no decrease in the range of supination and pronation of the left forearm when compared with that of the right. The patient had no ulnar nerve symptoms; sensibility in the ulnar nerve distribution was normal, and there was no intrinsic atrophy or clawing of the hand. Radiographs of the affected elbow showed cortical hyperostosis of the proximal part of the ulna and speckled calcification of the distal insertion of the triceps (Fig. 1). A computed tomographic scan revealed nodularity of the periosteal bone formation on a short segment of bone (Fig. 2). Magnetic resonance imaging demonstrated low signal intensity in all sequences (a classic sign of bone changes) and synovial inflammation without joint destruction or muscle atrophy (Fig. 3). Because splinting and physical therapy had proven to be ineffective and because the patient had severe limitation of functional use of the extremity, we recommended surgical release of the contracture. The procedure was performed through a medial approach to the elbow. The ulnar nerve was identified and mobilized. There were no adhesions along the ulnar nerve. With care taken to preserve the anterior oblique bundle of the medial collateral ligament, we resected all medial fibrotic, contracted capsuloligamentous structures. At this point, passive range of motion of the elbow was from 20° of flexion to 110° of flexion. The dissection was extended posteriorly through the interval between the triceps and the posterior aspect of the humerus. Contracted fibrous tissue was removed along with the calcification in the area of the triceps insertion. There was synovial thickening in the olecranon fossa, but the osseous contour was intact. We obtained 140° of elbow flexion without further release of the triceps fascia or muscle. Because extension was still limited, an anterior release was performed. The flexor-pronator muscle mass was found to be contracted, therefore necessitating release of the common origin of these muscles by Z-plasty. To achieve full extension, the brachialis muscle was elevated from the anterior aspect of the humerus and the anterior part of the elbow capsule was resected under direct visualization. After hemostasis was obtained, the flexor-pronator muscle was repaired in a lengthened position and the ulnar nerve was transposed subcutaneously. The wound was closed over suction drains, and the elbow was immobilized in an extended position. The hyperostotic cortical lesion of the proximal part of the ulna was partially excised for tissue diagnosis during the operation and the histologic photomicrograph is shown below (Fig. 4).
Histologic examination revealed dense bone. Together with the imaging findings, the histologic picture was consistent with the diagnosis of melorheostosis. Three days postoperatively, the elbow was mobilized with use of a continuous-passive-motion machine. The anterior cubital area developed a large bulla, which stabilized and resolved. The patient was discharged seven days postoperatively with a passive range of motion from 20° of flexion to 100° of flexion. Under the supervision of a therapist, gentle range of motion was encouraged for the next six weeks. An extension splint was worn at night during this time. Two years postoperatively, the range of motion was 20° of flexion to 135° of flexion and there was no sign of recurrence of the contracture (Fig. 5).
Proceed to Discussion >>Reference: Gong HS, Lee KH, Oh JH, Chung JH, Baek GH, Chung MS. Successful elbow contracture release secondary to melorheostosis. A case report. J Bone Joint Surg Am. 2008 May;90(5):1106-11.
Melorheostosis involving the upper extremity is not as common as that involving the lower extremity. Most reported cases involving the upper extremity are focused on the hand or on the sclerotomal distribution pattern. This report describes the case of a patient who had melorheostosis with isolated involvement of the proximal part of the ulna and an associated fixed 90° elbow contracture. Following contracture release, there was substantial improvement in the arc of elbow motion. The diagnosis of our patient was made on the basis of radiographic findings that showed hyperostosis along one side of the ulnar cortex. The nodularity of periosteal bone formation visualized on the three-dimensional computed tomography scan was unlike the structured laminated bone that is seen with myositis ossificans. Freyschmidt reviewed twenty-three cases of melorheostosis and described different radiographic patterns besides the classic one, which has been compared to dripping or flowing candle wax on the surface of the bone. The most frequent radiographic pattern described by Freyschmidt was “osteoma-like,” wherein the hyperostosis is located on the endosteal surface. Our patient had both endosteal hyperostosis on the posterior inner cortex of the ulna and nodular periosteal bone formation. A periosteal pattern of hyperostosis oriented in the long axis of the bone (as seen in our patient) is usually seen in adults, whereas an endosteal pattern of hyperostosis marked by streakiness of the long bones and spotting of the small bones prevails in children. The biopsy specimen obtained from our patient revealed dense benign bone that was consistent with melorheostosis and did not show features of myositis ossificans or parosteal osteosarcoma, both of which should be considered in the differential diagnosis. Although bone scintigraphy was not acquired in the case of our patient, it may be useful in confirming the diagnosis when other tests are equivocal or for the purpose of ruling out other types of asymptomatic sclerosing dysplasia, such as pyknodysostosis, osteopoikilosis, and osteopathia striata. The magnetic resonance imaging scan did not demonstrate ligamentous or capsular calcification in our patient; however, it was effective in demonstrating a normal elbow joint and no atrophy of the muscles preoperatively. Judkiewicz et al. reported that intra-articular extension of melorheostosis occurred in 35% of patients and that this finding may be associated with mineralization of the articular cartilage or with mechanical cartilage damage. It is also recognized that the longer that intervention is delayed, the more contracted the muscles become, and that the articular cartilage may also degenerate. Surgical treatment for this condition includes tendon lengthening, excision of fibrous and osseous tissue, fasciotomy, capsulotomy, sympathectomy, corrective osteotomy, Ilizarov lengthening, arthrodesis, implant arthroplasty, and even amputation of severely affected limbs with vascular ischemia. We were unable to find published reports of successful elbow contracture release in association with this condition. As the understanding of elbow anatomy and exposures improves, the results of the surgical treatment of heterotopic bone about the elbow are improving. We used the medial approach to release the ulnar nerve in our patient because, when flexion is limited to 90° prior to elbow release, ulnar neuritis frequently develops as patients regain flexion, which may limit further flexion following release of an elbow contracture. The medial approach is also helpful in addressing any fibrous contracture of the posterior oblique ligament of the medial collateral ligament; this approach was helpful in addressing the contracture found close to the hyperostotic lesion in our patient. It is notable that proximal release of the flexor-pronator muscle facilitated the approach to the anterior capsule and Z-plasty was effective in overcoming the long-standing muscle contracture. Recurrence is a major concern following contracture release in patients with melorheostosis. Younge et al. noted that the soft-tissue contractures and periarticular fibrotic changes seen in patients with melorheostosis resemble those seen in patients with arthrogryposis multiplex congenita, in which the contractures are rigid and do not stretch with growth, thus causing recurrence of deformities. Only one of sixteen soft-tissue releases in their series was successful. Campbell et al. also reported that deformity recurred in five of eight joints. However, similar to the good result reported in the case of our patient, positive results have been reported anecdotally in adult patients who underwent surgical debulking of the hyperostotic cortex or who had total resection of the lesion.
Reference: Gong HS, Lee KH, Oh JH, Chung JH, Baek GH, Chung MS. Successful elbow contracture release secondary to melorheostosis. A case report. J Bone Joint Surg Am. 2008 May;90(5):1106-11.
Osteopoikilosis
Osteopathia striata
Fibrodysplasia ossificans progressive
Melorheostosis
Osteopetrosis


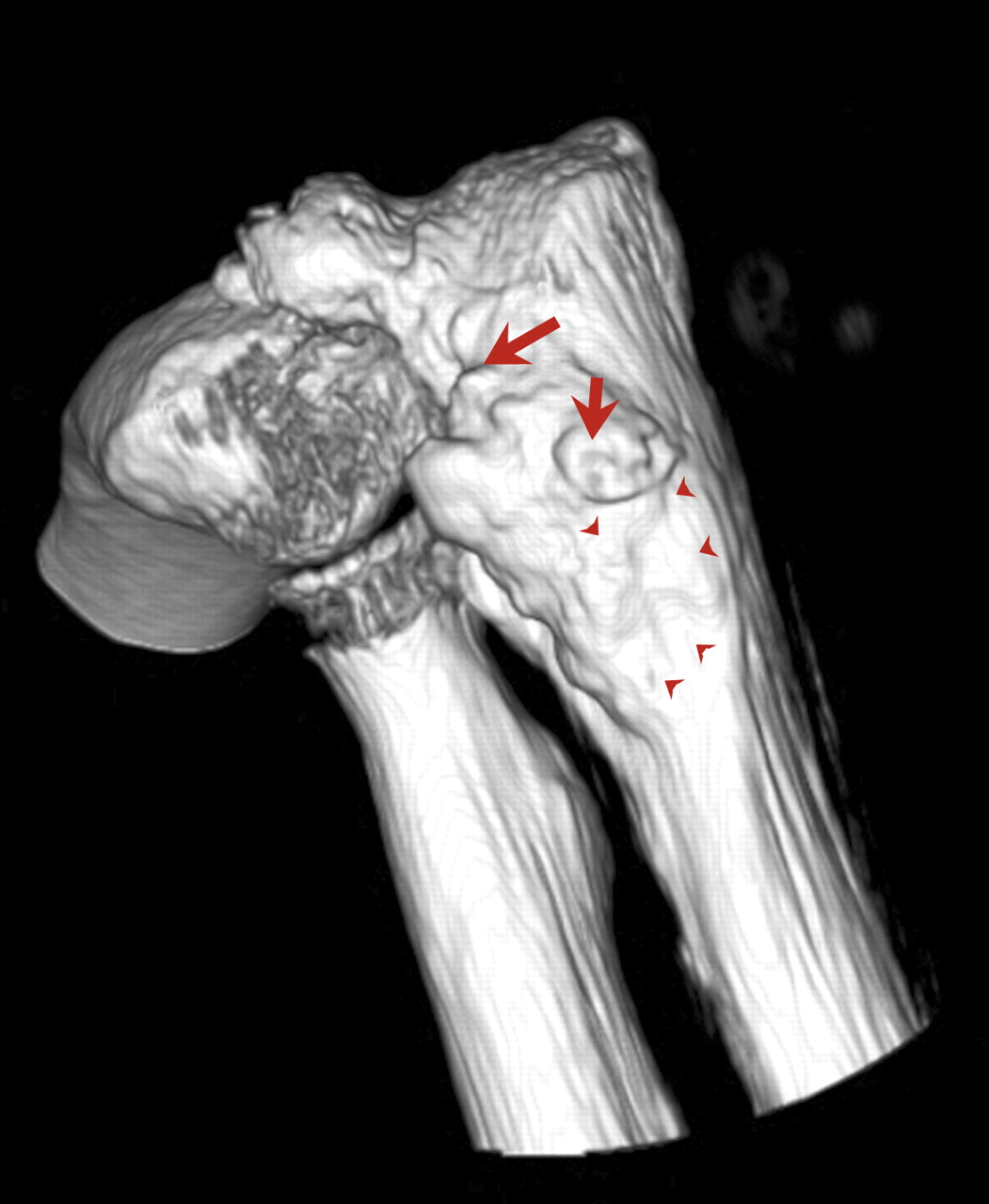

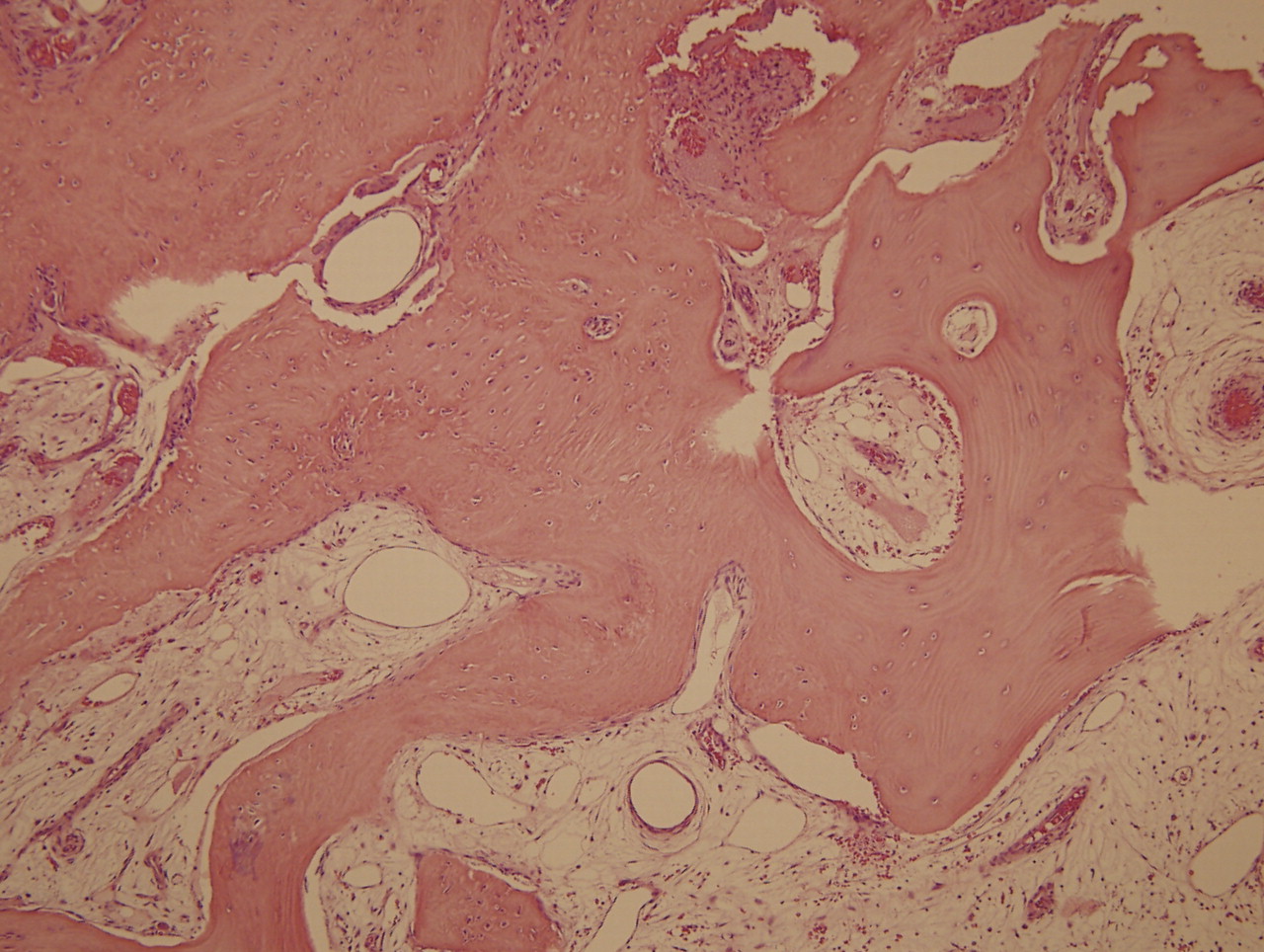
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5
Fig. 5