A Twenty-two-Year-Old Man with Mild Hip Pain Prior to Fracture
January 7, 2015
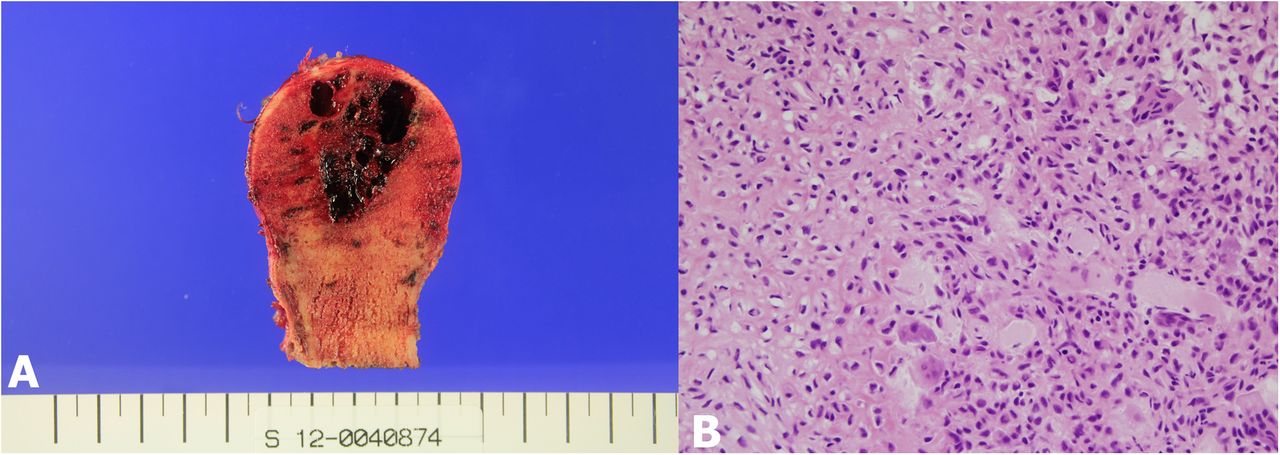
A twenty-two-year-old man was referred to our hospital for a pathologic fracture of the proximal part of the right femur. He described mild right hip pain that had persisted for over a month before the pathologic fracture had occurred. Radiographs and magnetic resonance imaging (MRI) revealed a pathologic fracture at the right femoral neck and trochanter, with an expansile trabeculated cystic mass (Figs. 1-A and 1-B). The mass appeared to be hypointense on T1-weighted imaging and hyperintense on T2-weighted imaging. In order to rule out a malignant bone tumor, an incisional biopsy was performed. Pathologic examination showed polygonal cells with vacuolated cytoplasm and round or indented nuclei. Multinucleated giant cells were dispersed evenly, and immunohistochemical staining for the S100 protein was positive (Fig. 2). We planned a tumor resection and total hip arthroplasty because the remaining bone of the proximal part of the femur was insufficient for osteosynthesis. Furthermore, the pathologic fracture could increase the risk of local recurrence. The operation was performed with the patient in the lateral position with use of a conventional posterolateral approach. The proximal part of the fracture was excised and the distal lesion was curetted. In addition, high-speed burring was used as an adjuvant treatment. After curettage, we implanted a PINNACLE Cup and Corail Stem (DePuy Orthopaedics, Warsaw, Indiana). Bone cement was employed in order to fill the void after tumor curettage and to help local tumor control. Because abductor weakness was predicted as a result of the aggressive curettage and debridement, a hip brace was applied for one month postoperatively. Weight-bearing on the right side was restricted for six weeks. Follow-up visits were scheduled for three and six weeks; three, six, and twelve months; and every three months thereafter for the first two years. Chest radiographs were also reviewed at every follow-up visit to monitor for pulmonary metastasis. The patient was followed for twelve months but was subsequently lost to follow-up. At forty-three months postoperatively, he revisited the outpatient clinic because of contralateral hip pain. A radiograph and MRI of the left hip showed a large lytic lesion with a thin sclerotic rim and internal septa located on the uppermost subchondral bone of the left femoral head (Figs. 3-A and 3-B). A bone scan and computed tomography (CT) of the chest showed no metastasis in any site and no local recurrence in the right hip.
We performed en bloc resection of the femoral head and reconstruction with a total hip arthroplasty with a ceramic-on-ceramic articulation that included a COREN cup and ID stem (Corentec, Cheonan, Korea) and a BIOLOX delta head and liner (CeramTec, Plochingen, Germany). To avoid seeding of the tumor cells, we performed the neck osteotomy at the upper margin of the lesser trochanter. The pathologic report confirmed a chondroblastoma (Figs. 4-A and 4-B). A functional evaluation was performed with the International Society of Limb Salvage (ISOLS) classification system, which includes six parameters: pain, function, emotional acceptance, use of walking supports, walking ability, and gait. Each category is rated 0 to 5, with 0 being the worst score and 5 the best score, with a maximum score of 30. A score of 24 to 30 is considered excellent, 18 to 23 is considered good, 12 to 17 is considered fair, and less than 12 points is considered poor. Fifteen months after the second surgery, the ISOLS scores were 26 for the right hip and 29 for the left hip, and the patient had returned to work (Fig. 5).
Proceed to Discussion >>Reference: Yoon B-H, Cho HS, Lee Y-K, Koo K-H. Metachronous bilateral chondroblastoma of the proximal part of the femur with a pathologic fracture: a case report. JBJS Case Connect. 2014 Oct 08;4(4):e93.
Chondroblastoma was first described as a benign tumor. This view has been supported by many reports. However, some studies have reported more aggressive lesions that have a tendency for multiple relapses and metastasis or malignant transformation of the chondroblastoma. To our knowledge, there have been no previous reports of metachronous bilateral chondroblastoma. Metastatic chondroblastomas are very rare (0.8% to 6% of chondroblastomas); they can metastasize, most commonly to the lung, neighboring or distal bones, and soft tissues. Lung metastasis can occur as a result of tumor embolization after surgical manipulation, but it usually develops following local recurrence of the primary tumor. Therefore, full staging with chest radiographs and/or CT of the chest is advisable with any locally recurrent chondroblastoma. Neither radiographs nor CT revealed metastatic lesions in our patient. The term “malignant chondroblastoma” is controversial. Some authors consider locally aggressive chondroblastomas to be malignant, even in the absence of metastasis, and they can be associated with high mortality. Neither pleomorphic cells nor mitotic figures were present on histological examination in our case, so neither lesion was diagnosed as malignant. Chondroblastomas containing foci of aneurysmal bone cyst have been reported to show a higher recurrence rate than those without such foci. In our patient, hemorrhagic cystic areas were seen; however, we are unaware of any correlation between this finding and metachronous lesions. There have been two previously reported cases of multifocal chondroblastoma, but both showed conventional histology and were considered multiple primary lesions. In one of these cases, there was an interval of seven years between recognition of the two lesions, and there were no clinical or histological features of malignant tumor. The proximal part of the femur is a common site for primary bone tumors or metastasis, and two-thirds of all long-bone pathologic fractures occur in the femur, usually involving a proximal lesion. When there is a pathologic proximal femoral fracture in a patient with a good life expectancy, an endoprosthetic replacement is a sensible option, both functionally and oncologically. Proximal femoral implants have greater survival rates than implants at other sites; implant survival rates of 77% to 94% at ten years with revision as an end point have been reported. Although there was no acetabular involvement in our patient, we performed total hip arthroplasty because we anticipated high risk for a later revision secondary to acetabular erosion. The femoral head is the third most common site for chondroblastoma. We considered performing surgical curettage with or without bone graft of our patient’s left-sided lesion, but the approach to the femoral head is complex; it is difficult to determine the optimal extent of curettage under fluoroscopic guidance. The recurrence rate of chondroblastomas of the femoral head is as high as 21%, and en bloc resection would be expected to have a low risk of local recurrence. There have been reports of the development of osteoarthritis of the hip joint secondary to femoral head collapse after curettage of lesions in the femoral head. The size of the lesion on the left side in our patient was large and very close to the articular margin. In such cases, en bloc resection with total hip arthroplasty is an alternative option that can avoid the common complications of local recurrence and can prevent the development of osteoarthritis. After full counseling with our patient regarding the lesion, we performed a tumor resection with a total hip arthroplasty. We believe that use of fourth-generation ceramic-on-ceramic implants in total hip arthroplasty should have a prolonged duration as long as there is no recurrence of the lesion.
Reference: Yoon B-H, Cho HS, Lee Y-K, Koo K-H. Metachronous bilateral chondroblastoma of the proximal part of the femur with a pathologic fracture: a case report. JBJS Case Connect. 2014 Oct 08;4(4):e93.
Dedifferentiated chondrosarcoma
Metachronous chondroblastoma
Metastatic chordoma
Metachronous aneurysmal bone cyst
Metastatic chondroblastoma

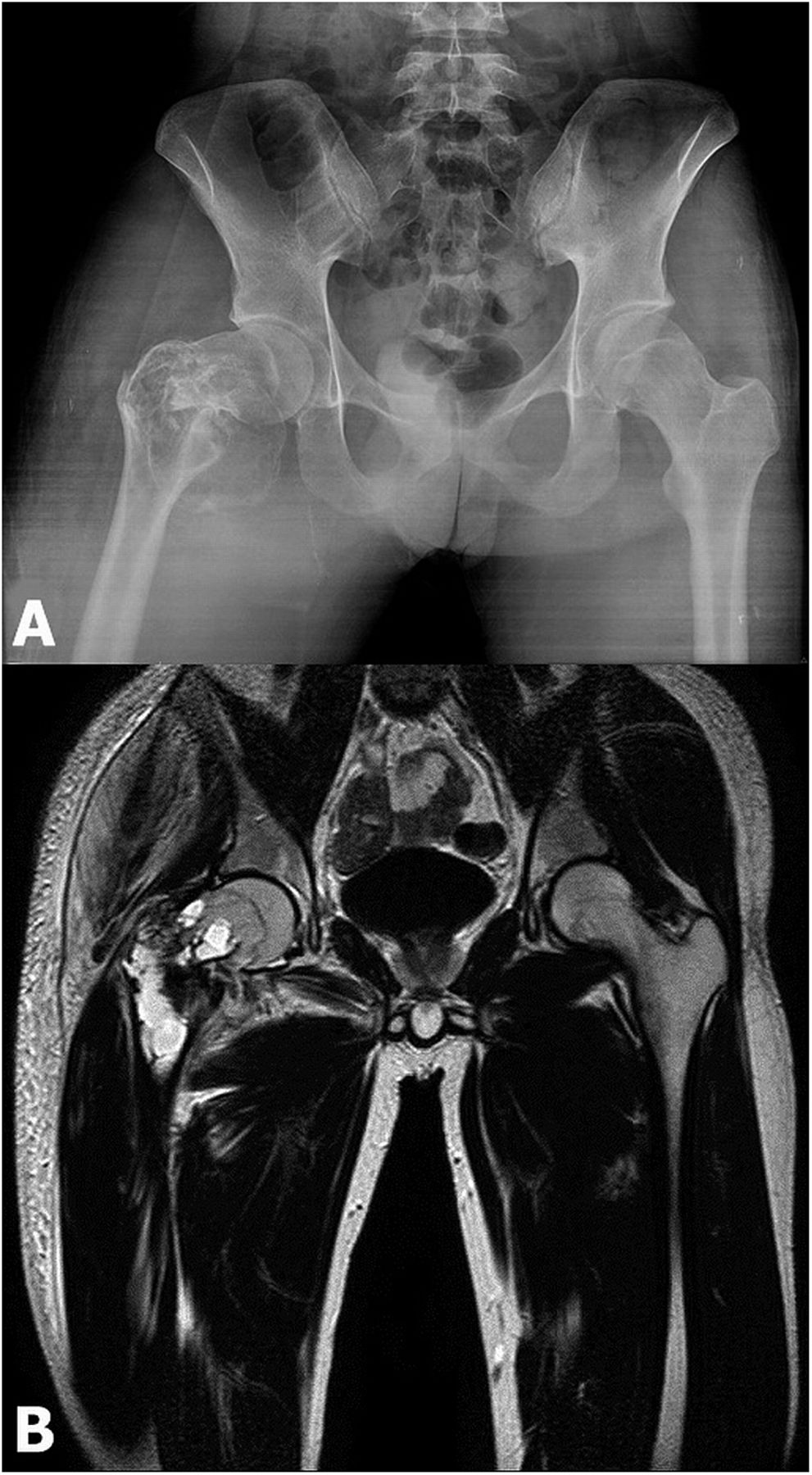
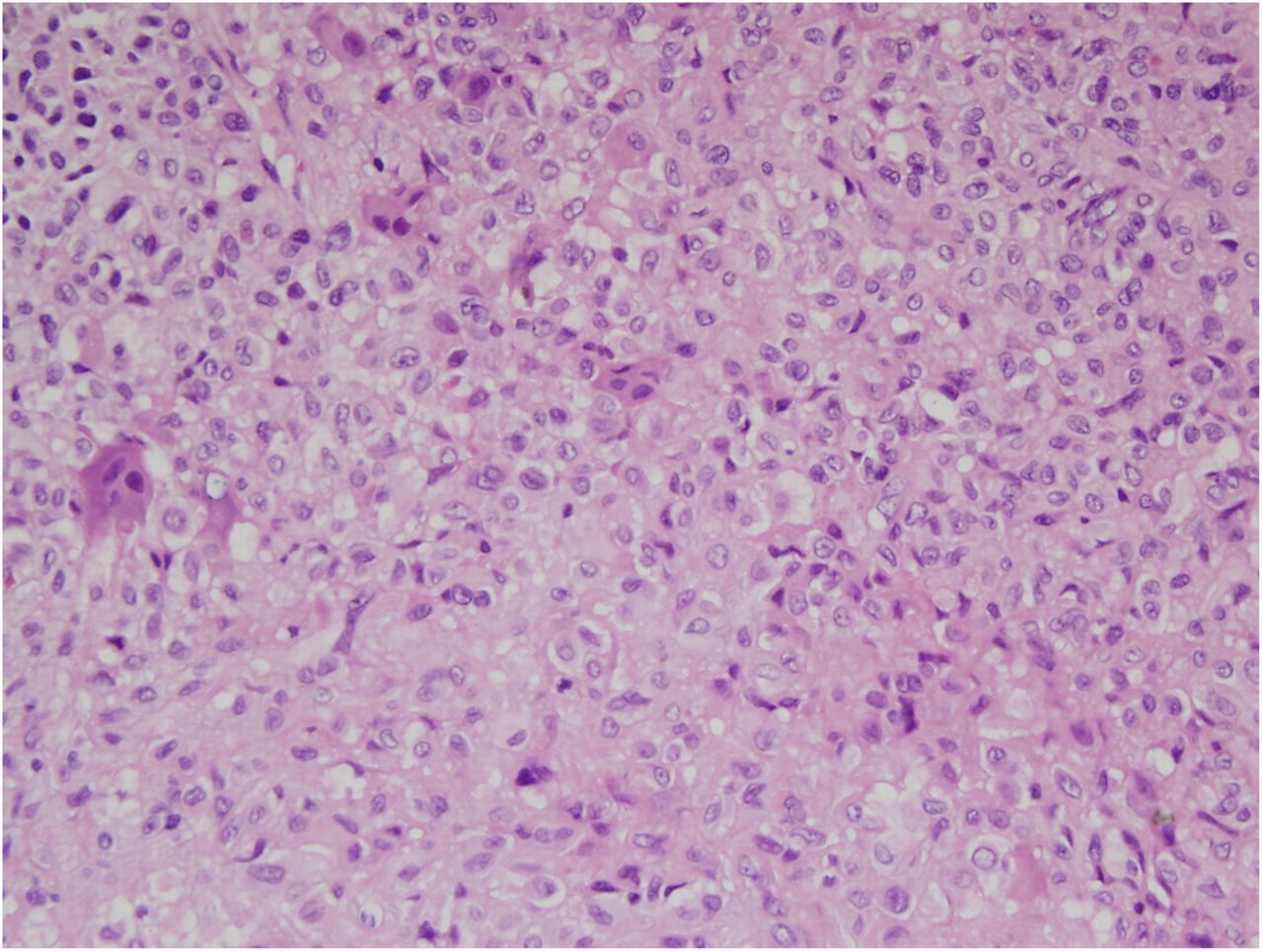
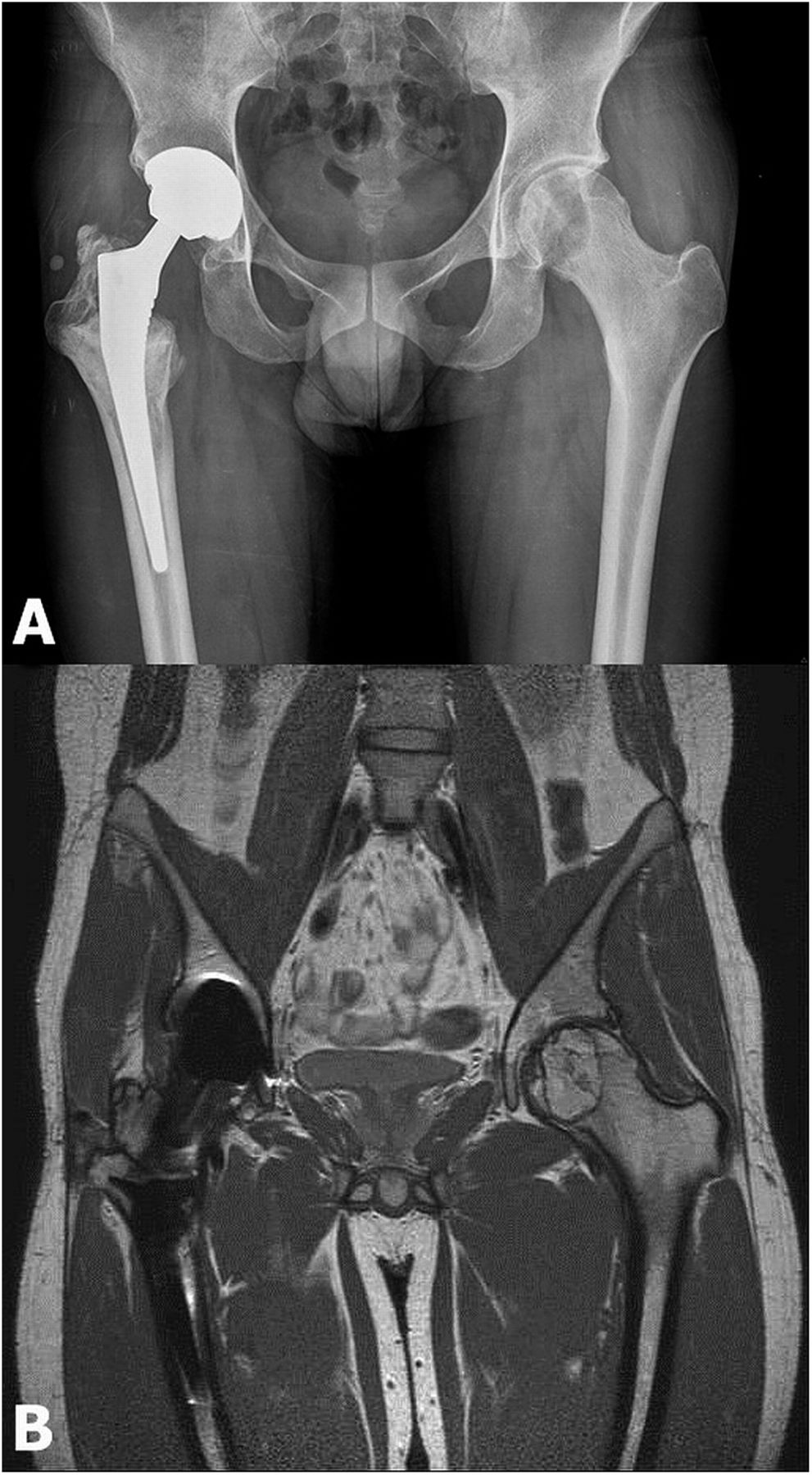
 Fig. 1
Fig. 1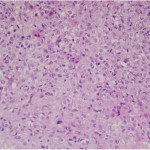 Fig. 2
Fig. 2 Fig. 3
Fig. 3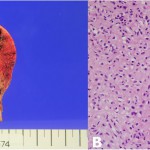 Fig. 4
Fig. 4 Fig. 5
Fig. 5