An Eighty-one-Year-Old Man Unable to Extend the Ring Finger of the Right Hand
June 3, 2015
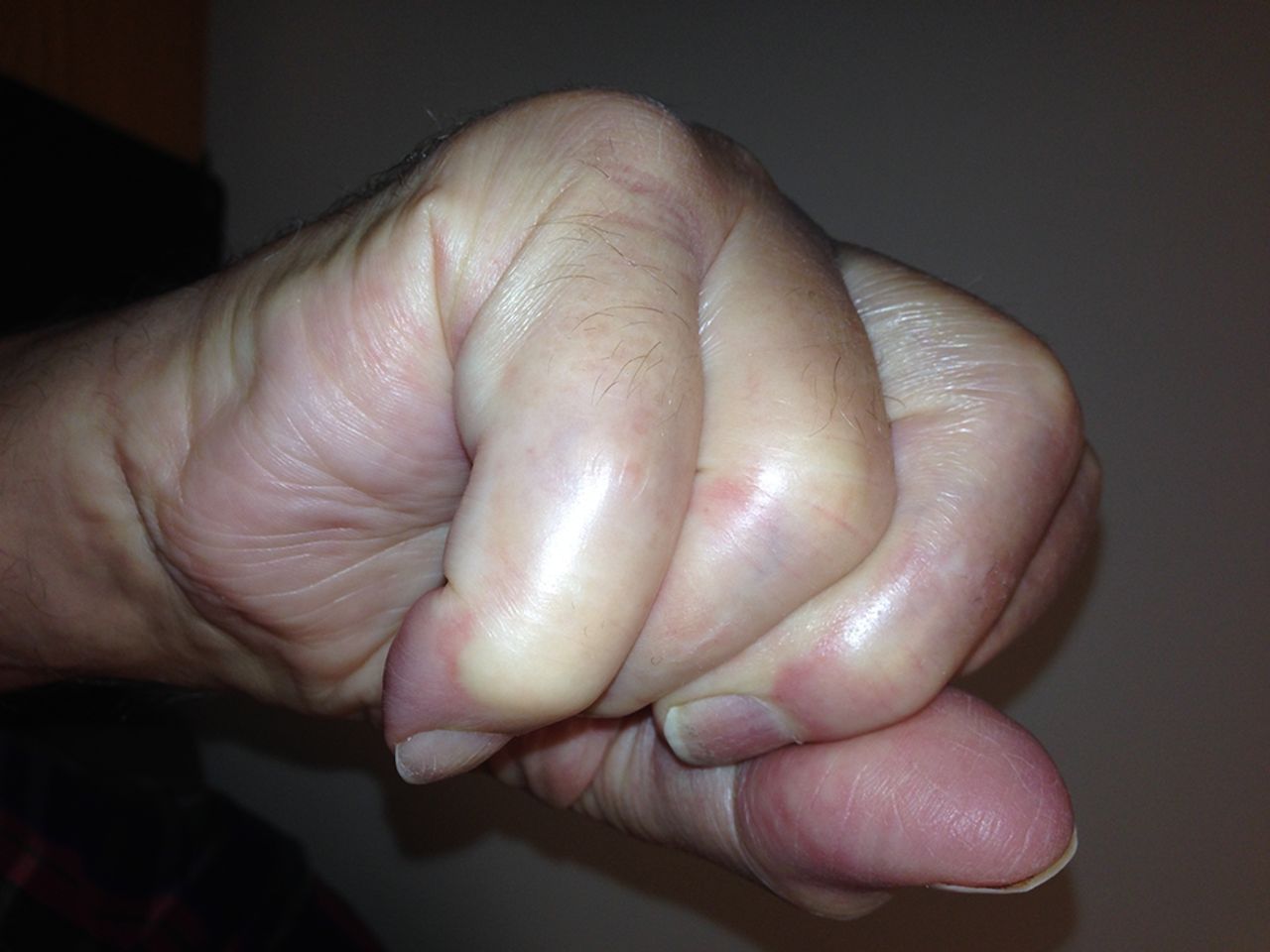
An eighty-one-year-old man presented with the sudden inability to extend the metacarpophalangeal joint of the ring finger of the dominant right hand. He had first noticed this finding three months prior to presentation. He denied any history of a traumatic event prior to the problem. He had begun taking an antibiotic for an ear infection but otherwise was taking no significant medications other than over-the-counter preparations. There was no pain in the affected digit either before or after the loss of extension ability. He described no other joint pain or other musculoskeletal difficulties. He had no history of gout, rheumatoid arthritis, or inflammatory conditions. On physical examination, there was an extension deficit of the metacarpophalangeal joint of the right ring finger. The patient was unable to actively extend the metacarpophalangeal joint or hold it up against gravity. The joint postured in 40° to 50° of flexion (Figs. 1-A and 1-B). The flexor digitorum superficialis and flexor digitorum profundus tendons were both intact in the affected finger and in the remaining fingers bilaterally. He had no other joint pain or sensory deficits, and no posterior interosseous nerve deficit was noted. Imaging revealed arthritic changes at the interphalangeal joints and joint space narrowing at the metacarpophalangeal joint (Fig. 2-A). A lateral radiograph demonstrated prominence of the ulnar head and asymptomatic osteophytes in the region of the ulnar head (Fig. 2-B). Clinically, these did not interfere with forearm rotation. The patient was taken to the operating room, and a small amount of tenosynovium with fluid in the affected finger was noted. A biopsy of the affected tissue was sent for culture. The patient underwent debridement and suturing of the affected area. The fourth extensor compartment was incised and inspected. No osseous protrusions or any synovitis that may have caused tendon erosion were identified. Since the extensor digiti minimi was intact, there was no indication to open the fifth extensor compartment. Intraoperatively, it also was noted that the patient had a congenitally absent extensor digitorum communis (EDC) to the small finger.
In the operating room, a rupture of the EDC tendon of the ring finger just distal to the extensor retinaculum was found (Fig. 3). A small amount of tenosynovium with fluid was noted at the site of the tendon rupture. A biopsy of the tissue was sent for culture. The ruptured EDC tendon was debrided, and it was sutured as a side-to-side transfer to the EDC tendon of the long finger. On synovial assessment, no acid-fast bacilli were isolated at seven weeks, there was no bacterial growth with aerobic and anaerobic cultures, and no fungus was isolated. Surgical pathology showed nonspecific chronic synovitis of the synovium, and the extensor tendon biopsy specimen showed degenerative changes. Postoperatively, there was correction of the extension deficit. Given the clinical findings and history, this most likely represents a case of ciprofloxacin-induced tendon rupture in the extensor tendons of the right hand. Six months postoperatively, the incision was healing in a benign fashion. The hand was fully sensate and well perfused. The metacarpophalangeal extension of the ring finger demonstrated an 18° extension lag, with flexion of the metacarpophalangeal joint to 83°. The flexion distance between the tip of the finger and the distal palmar crease was approximately 1 cm (Figs. 4-A and 4-B). The patient had no other tendon deficits and no evidence of tenosynovitis. There was an extension lag in the ring and small fingers (as Figs. 4-A and 4-B); however, these tendons were functioning and intact as he was able to hold the joints in extension against gravity.
Proceed to Discussion >>Reference: DeWolf MC, Warhold LG. Ciprofloxacin-induced extensor tendon rupture in the hand: a case report. JBJS Case Connect. 2015 Apr 08;5(2):e30.
Fluoroquinolone-induced tendinopathy is a rare, albeit important, clinical condition. Awareness of this condition has grown with an increase in case reports and a black-box warning by the U.S. Food and Drug Administration for prescription of this class of medication in special populations. It is imperative for orthopaedic surgeons to be familiar with this condition because these patients may first present to the surgeon. Kim provided an excellent clinical review of the topic of fluoroquinolone-induced tendon rupture with topics relevant to the clinician; a brief summary of these topics is provided here. The importance of this issue is likely to grow given the wide use of fluoroquinolones to provide broad-spectrum coverage to many pathogens, including gram-negative pathogens. Additionally, fluoroquinolones have high oral bioavailability and excellent tissue penetration. They are commonly used for respiratory, urogenital, gastrointestinal, joint, and bone infections. Ciprofloxacin has been shown to be the antibiotic that causes this condition in over 90% of fluoroquinolone-induced tendinopathies; however, other fluoroquinolones, including norfloxacin, pefloxacin, ofloxacin, and levofloxacin, are associated with tendon rupture. Patients with tendinopathy may present with bruising, immobility of the joint, or even a “snap” or a “pop.” Evaluation includes a careful history and physical examination. In addition, imaging may be useful. Ultrasound provides an inexpensive way to confirm that a tendon has been ruptured and also whether it is a partial or complete rupture. On ultrasound, there will be hypoechoic areas and increased tendon thickness, as well as gaps at the site of rupture, hyperemic torn tendon ends, or fluid collection. Magnetic resonance imaging is another modality that may be utilized, although it is less available and more expensive than ultrasound. The differential diagnosis includes gout flares versus infection; the history, the physical examination, routine laboratory work, and imaging will help sort out the cause of the problem. For tendinopathy, the mainstays of treatment include rest, physical therapy, and discontinuation of the offending medication. Specific treatments depend on the site of the tendinopathy. Because of the risk of rupture, patients should be advised to see a physician if they develop redness, pain, swelling, or stiffness. Likewise, physicians should be adept at recognizing these symptoms as a potential impending rupture and initiate the treatment described above. Tendon rupture is usually addressed by an orthopaedic surgeon. The risk factors associated with fluoroquinolone-induced tendon disorders include age older than sixty years, corticosteroid use, history of musculoskeletal disorders, and chronic diseases such as diabetes mellitus and renal failure. Tendinopathy typically occurs shortly after administration of fluoroquinolone, with a median time of six days. Likewise, half of tendon ruptures have been shown to occur within one week. The incidence of tendon injury is between 0.08% and 0.20%. The pathophysiology for rupture has been described by several sources. One theory is the direct toxic effect of oxidative stress from fluoroquinolones. In vitro studies have shown that ciprofloxacin can cause decreases in cell proliferation, collagen synthesis, and proteoglycan synthesis in fibroblasts, with a concomitant increase in matrix-degrading proteolytic activity. This imbalance of protease activity and inhibition of cell proliferation and synthesis have been hypothesized to contribute to the tendinopathies seen with fluoroquinolone use. Burkhardt et al. showed that there is necrosis of chondrocytes followed by disruption of extracellular matrix and formation of fissures, as well as depletion of collagen from the cartilage within forty-eight hours of dosing dogs with difloxacin, a fluoroquinolone. Tendon ruptures can result from a variety of causes, including the presence of osteophytes, synovial proliferation, and fluoroquinolone use. We were not able to definitively prove that the tendon rupture in our patient was the direct result of fluoroquinolone use; however, we postulate that ciprofloxacin played a substantial role for several reasons. First, as previously discussed, fluoroquinolones have been shown to be associated with tendon rupture. Second, intraoperative findings did not identify an anatomic defect such as synovial proliferation or osteophytes in the area of the tendon rupture. Finally, our patient had no history of gout, rheumatoid arthritis, or inflammatory conditions. In summary, this individual did not have any other risk factors, and the timing of the rupture relative to the initiation of fluoroquinolone therapy is consistent with other reports of fluoroquinolone-induced tendon rupture; therefore, we believe that fluoroquinolone use was the most likely cause of the tendon rupture.
Reference: DeWolf MC, Warhold LG. Ciprofloxacin-induced extensor tendon rupture in the hand: a case report. JBJS Case Connect. 2015 Apr 08;5(2):e30.
Gout
Ciprofloxacin-associated tendon rupture
Rheumatoid arthritis
Atypical mycobacterial infection
Reiter syndrome





 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B Fig. 3
Fig. 3 Fig. 4-A
Fig. 4-A Fig. 4-B
Fig. 4-B