A Seventy-eight-Year-Old Woman with Pain, Swelling, and Lesion on the Left Leg
June 17, 2015
In August 2012, a seventy-eight-year-old white woman presented to the Department of Orthopaedic Oncology at our institution seeking consultation regarding a lesion in the left tibia. She had undergone successful total knee arthroplasty five years earlier for osteoarthritis of the left knee. She was in her normal state of health with a well-functioning left knee replacement before developing knee pain and swelling in April of the same year. Initial evaluation at an outside facility had led to a suspicion of multifocal bursitis. The pain and swelling progressed over the next four months and she was eventually referred to our Department of Orthopaedic Oncology following concern about a destructive lesion in the proximal part of the tibia. She reported that she had no constitutional symptoms and her medical history was limited to hypertension and dyslipidemia. Physical examination demonstrated left-knee tenderness and infrapatellar swelling. The extensor mechanism was intact with a range of motion from 0° to 100°. Radiographic evaluation revealed permeative destruction of the proximal part of the tibia surrounding the tibial component of the knee prosthesis (Fig. 1). Magnetic resonance imaging (MRI) demonstrated a tibial mass with extension into the soft tissue, although full evaluation was limited by prosthesis-related artifact. Percutaneous needle biopsy was performed for further evaluation of the mass (Fig. 2).
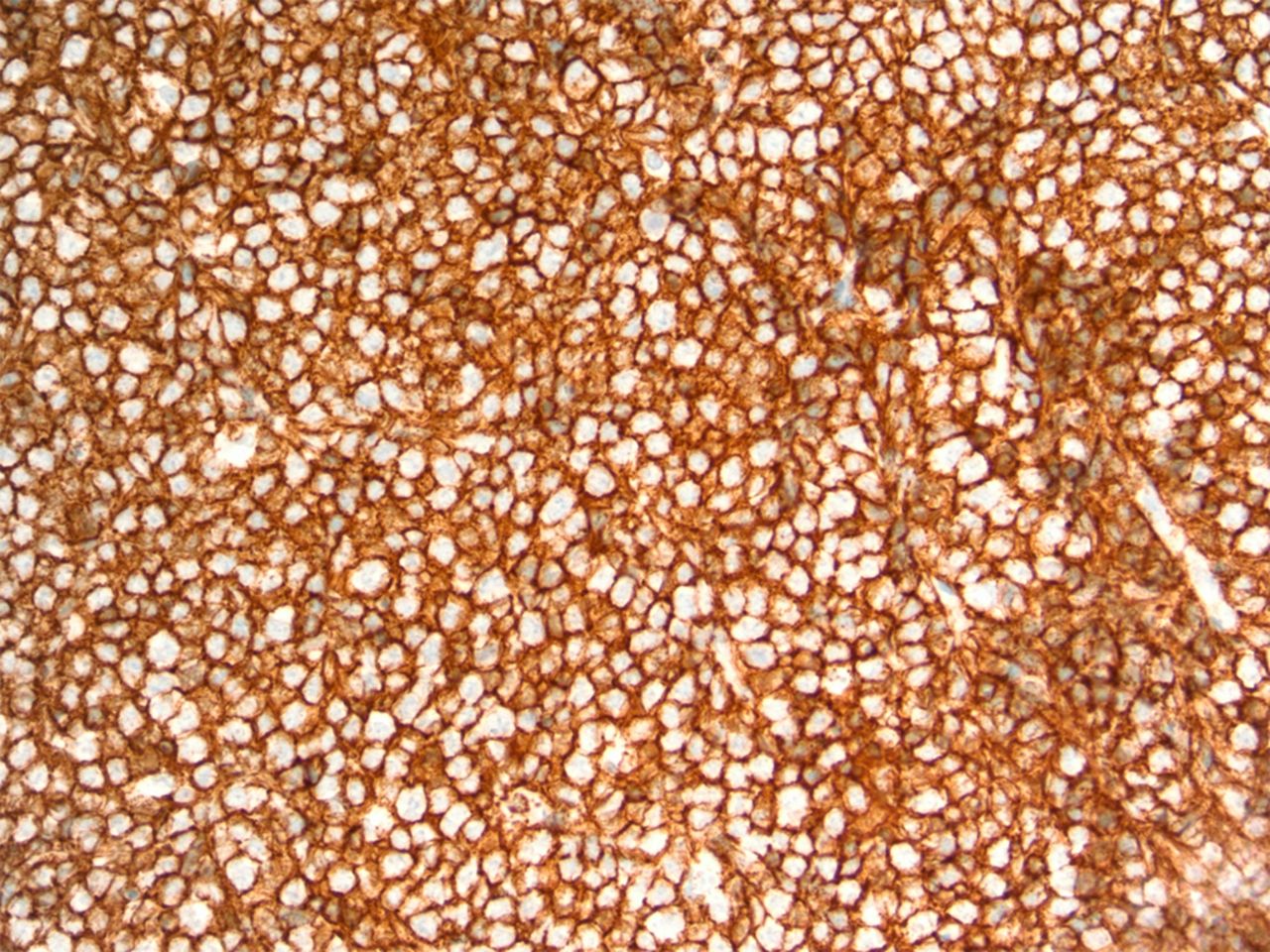
Immunohistochemical staining was positive for CD20 (Fig. 3), CD10, BCL2, and BCL6. Staining for CD3, p53, MUM-1, and EBER was negative. Ki-67 expression was 80% consistent with a rapid proliferative index. Cytogenetic testing was positive for MYC gene rearrangement via fluorescent in situ hybridization (FISH). The final diagnosis was diffuse large B-cell lymphoma, germinal-center subtype, with BCL2 overexpression and C-MYC rearrangement. There were no indications for surgical intervention at this time so the patient was referred to a local hematology/oncology practice for staging and chemotherapy. Computed tomography (CT) revealed no evidence of regional or systemic lymphadenopathy, suggesting limited disease. Iliac crest biopsy was negative for bone marrow involvement. Complete staging was consistent with primary lymphoma of bone, Ann Arbor stage 1AE. The patient completed six cycles of R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone) therapy followed by consolidative radiation therapy to the knee. Restaging studies, including whole-body positron emission tomography (PET), were negative for residual disease, indicating complete remission. In February 2013, the patient presented again to the Department of Orthopaedic Oncology with recurrent pain in the knee. Physical examination demonstrated deformity of the knee and unsteady gait. Radiographic evaluation revealed a fracture of the proximal part of the tibia with varus angulation. Restaging studies were negative for disease recurrence. The patient elected to undergo a complex knee reconstruction with a modular oncology prosthesis. Following medical clearance, the patient was scheduled for knee reconstruction in April 2013; however, on the day of the operation, she had preoperative hypotension and the surgery was aborted. Subsequent medical evaluation led to the detection of severe vascular disease requiring surgical reconstruction. In light of the patient’s age and newfound vascular pathology, knee reconstruction was discouraged. By this time, the fracture had fully united in varus (Fig. 4) and she was fitted for a knee-ankle-foot orthotic to aid with walking. At the time of the writing of this report, the lymphoma remained in remission, although the patient continued to experience modest pain in the knee. She was able to walk with the assistance of a walker but has been largely restricted to household ambulation.
Proceed to Discussion >>Reference: Ibrahim I, Haughom BD, Fillingham YA, Brown N, Gitelis S. Primary lymphoma of bone complicating total knee arthroplasty: an unexpected mode of prosthesis failure: a case report. JBJS Case Connect. 2015 Apr 22;5(2):e34.
Hematopoietic malignancies arising at the sites of orthopaedic implants have been infrequently reported in the literature, with a MEDLINE/PubMed search revealing just over a dozen cases involving bone or soft tissue and only three cases of bone lymphoma occurring alongside a total knee replacement. The mean duration from the total knee arthroplasty to the presentation of the lymphoma was 7.3 years (range, two weeks to sixteen years), and the average age at diagnosis was 73.3 years (range, sixty-six to seventy-eight years). Biopsy results were consistent with diffuse large B-cell lymphoma in all cases. The carcinogenic potential of implant devices has long been an area of concern for orthopaedic surgeons. Regular wear of implant materials results in the broad dispersal of metal, polyethylene, and methacrylate particles throughout the body. These particles have been shown to promote genomic instability through DNA and chromosomal injury. Patients undergoing revision arthroplasty have also been shown to have higher rates of lymphocyte aneuploidy and chromosomal translocations than they had at the time of the primary joint replacement. Genomic instability secondary to implant debris confers a theoretical hazard of malignancy in patients treated with surgical implants, with this risk perhaps being most substantial with joint prostheses because continuous bearing-surface wear liberates massive amounts of particulate and soluble debris. The early works of Oppenheimer et al. and Heath et al. have established the carcinogenic potential of implant materials in rat models. Later studies have also suggested a link between metallic implant materials and hematologic malignancies, including lymphoma. Memoli et al. studied the carcinogenic potential of several implant materials in rats and observed a significant increase in the prevalence of osseous lymphomas and, to a lesser degree, sarcomas following exposure to various metallic alloys. In a study of the rates of malignancy following total hip arthroplasty, Gillespie et al. observed a small increase in the overall prevalence of tumors of lymphatic and hematopoietic origin. Nonetheless, epidemiological studies have failed to demonstrate a significant increase in the prevalence of malignancy, including lymphoma, in patients treated with surgical implants. Joint replacement surgery has revolutionized the care of patients with osteoarthritis of the hip or knee. Modern arthroplasty techniques are very effective, with high rates of patient satisfaction and excellent prosthetic longevity. Rates of joint replacement surgery have been on the rise in the United States. A discharge survey conducted by the Centers for Disease Control and Prevention (http://www.cdc.gov/nchs/fastats/inpatient-surgery.htm) showed that, together, the total numbers of primary total knee and total hip arthroplasties exceeded one million in 2010. By 2030, the demand for total hip arthroplasty and total knee arthroplasty is predicted to increase by 673% and 174%, respectively. Mechanisms of failure following total knee arthroplasty are well described, with osteolysis being the most common reason for revision five years after primary total knee arthroplasty. Wear debris, once again, is believed to incite foreign body reactions and inflammatory cascades leading to bone resorption and radiolucency. Osteolytic changes may be discovered incidentally in patients during early radiographic follow-up, but patients typically present with pain, swelling, and acute synovitis. The rate of osteolysis may depend on a number of factors, including patient age, sex, host response, and activity level. Progressive bone resorption and loss of fixation may eventually lead to component loosening and periprosthetic fracture. Primary lymphoma of bone occurring at the site of a total knee arthroplasty may be difficult to differentiate from symptomatic osteolysis, especially early in the disease course. In addition, the rarity of primary lymphoma of bone and the unproven carcinogenicity of orthopaedic implants lead to low suspicion for malignancy in such patients. Timely recognition of periprosthetic lymphoma, however, is imperative for early oncological care and surgical stabilization, which may be necessary to prevent catastrophic implant failure. For this reason, periprosthetic lymphoma should be included in the differential diagnosis for any patient presenting with knee pain, a knee mass, or lytic destruction of the proximal part of the tibia or distal part of the femur following knee arthroplasty. Recognition of a bone lymphoma may be challenging because of the indolent nature of this neoplasm. Patients often present with mild symptoms, and radiographs may show little or no bone destruction. When dealing with a patient with inexplicable symptoms, it is important to be vigilant. Frequent clinical and radiographic follow-up is necessary, and ultimately the diagnosis will become clear. Clinical indications of lymphoma may include lymph node enlargement and “B symptoms” (fever, night sweats, or unintentional weight loss), although systemic symptoms are less common with primary lymphoma of bone. Once bone destruction is evident, advanced imaging and laboratory testing (including analysis of inflammatory markers) should be performed, and the diagnosis of a bone neoplasm will be evident. A useful tool for evaluating a patient with skeletal pain is a technetium bone scan. This will show bone turnover even when the radiograph does not show destruction. The same approach should be applied to a patient with an orthopaedic implant. The patient should be followed closely and carefully until the diagnosis is made. When ordering an MRI for a patient with an orthopaedic implant, consultation with a radiologist may be necessary to minimize metallic artifact and maximize test sensitivity. In conclusion, primary lymphoma of bone is a rare musculoskeletal malignancy that may arise in the vicinity of metallic implants. While some studies have suggested a relationship between metallic alloys and genomic instability, true carcinogenesis remains questionable. Implant-associated lymphomas pose a unique problem for orthopaedic physicians because of diagnostic challenges and the unique implications of disease and treatment-related complications. Periprosthetic primary lymphoma of bone simulates symptomatic osteolysis from implant wear and should be included in the differential diagnosis of a patient presenting with knee pain, a knee mass, or lytic destruction after knee arthroplasty.
Reference: Ibrahim I, Haughom BD, Fillingham YA, Brown N, Gitelis S. Primary lymphoma of bone complicating total knee arthroplasty: an unexpected mode of prosthesis failure: a case report. JBJS Case Connect. 2015 Apr 22;5(2):e34.
Ewing sarcoma
Chronic Staphylococcus aureus infection
Polyethylene wear debris-initiated osteoclastic mass
Lymphoma of bone
Chondrosarcoma


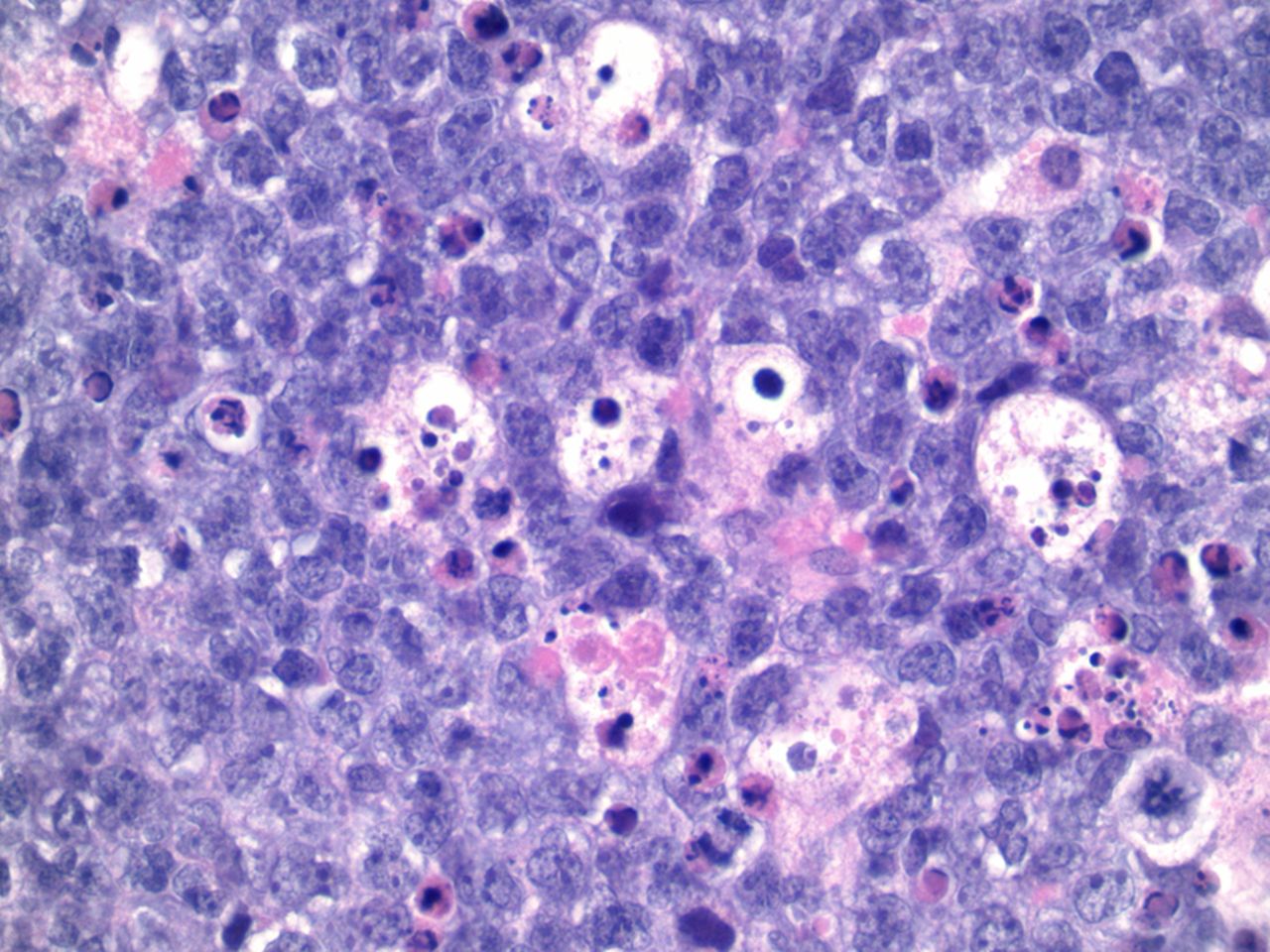
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4