An Eight-Year-Old Girl with Increasing Thigh and Groin Discomfort
May 18, 2016
An eight-year-old-girl had a seven-week history of progressively increasing right thigh and groin discomfort. She had begun to experience mild right inner-thigh discomfort after participating in a “jogathon” at school, where she ran fifteen laps around a track (6.04 km [3.75 mi]). Her pediatrician diagnosed a muscle strain and prescribed ibuprofen. Five weeks before referral, she had no longer been able to run, and the pediatrician had ordered a radiograph of the hip, which had been reported as normal. Three weeks before presentation, she had developed pain while walking, and her parents, without medical advice, had rented a wheelchair for her to use at home and at school. Subsequently, she had been seen twice at an urgent care clinic; the results of a blood test, including white blood-cell (WBC) count, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) level, had been normal. Another radiograph of the hip had been reported as normal by a radiologist. One week prior to presentation, she had begun to experience increasing right groin discomfort at night and had started to sleep with a pillow under the knee. There had been no chills, fever, cough, anorexia, weight loss, abdominal pain, or numbness and tingling of the extremity. Because of the inability to walk, the pediatrician had referred her to an orthopaedic surgeon, who subsequently obtained a radiograph of the hip and magnetic resonance imaging (MRI) of the pelvis and then referred her to our pediatric orthopaedic surgery clinic.
The patient had lived in India for six months during the previous year. Her immunizations were up to date, and the tuberculosis test was negative. Height, weight, and vital signs, including temperature, were normal for age. She did not have tenderness on palpation of the abdomen, and there was only mild tenderness to palpation over the medial aspect of the proximal part of the thigh in the adductor region. She had no lymphadenopathy. She held the right hip in approximately 20° of flexion and slight adduction. Hip flexion was not possible beyond 90° secondary to substantial discomfort; she had severe pain and resisted any attempts to extend or rotate the hip.
Laboratory studies disclosed a hemoglobin level of 10.2 g/dL (normal, 11.5 to 14.5 g/dL), a WBC count of 6.5 × 10/μL (normal, 4.5 to 13.5 × 10/μL) with a differential of 50% neutrophils and 40% lymphocytes, an ESR of 26 mm/hr (normal, 0 to 20 mm/hr), and a CRP level of 1.6 mg/dL (normal, <0.9 mg/dL).
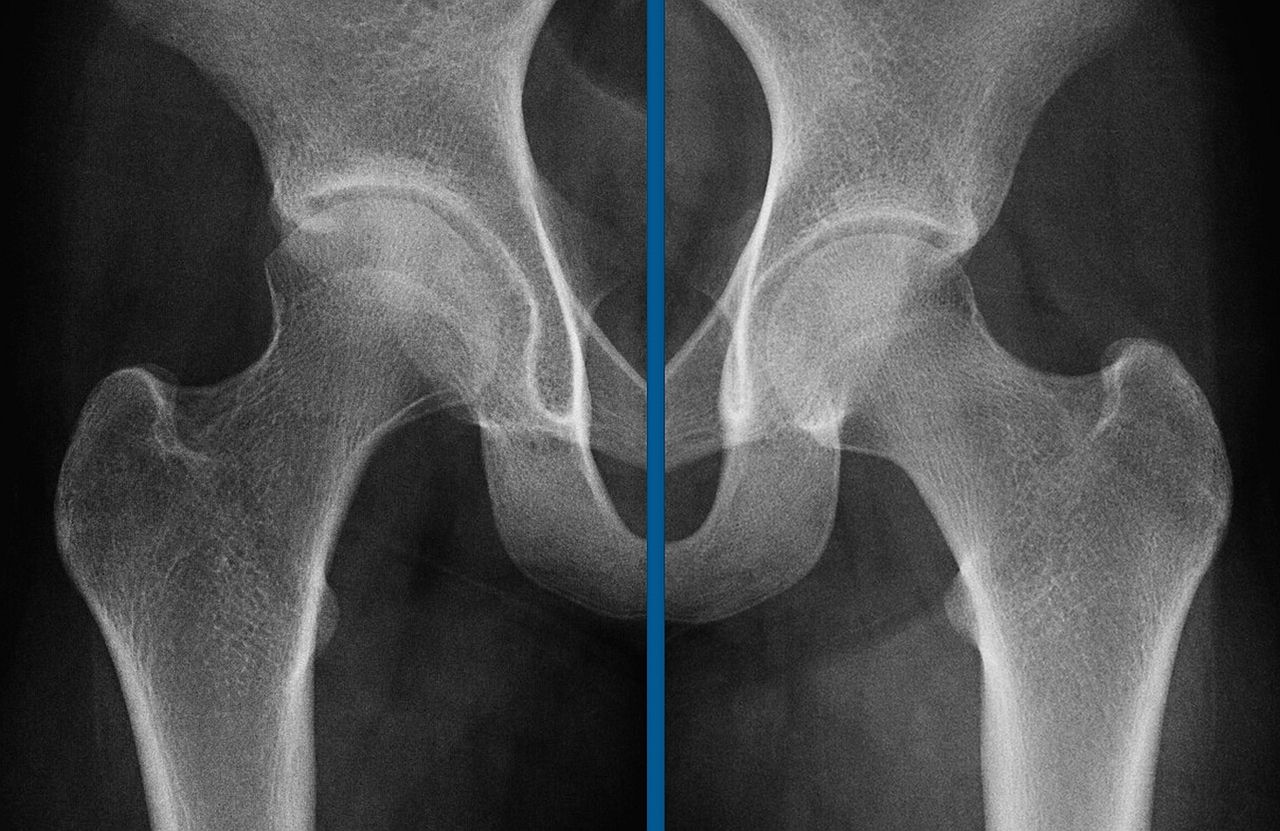
An anteroposterior radiograph of the pelvis was obtained (Fig. 1). Radiographs of the chest and thoracolumbar spine were normal. MRI was also obtained (Figs. 2-A and 2-B).
The patient was taken emergently to the operating room for ultrasound-guided aspiration of the fluid in the iliopsoas muscle. With a guidewire, an 8.5-French catheter was advanced into the fluid collection, and approximately 3,000 cm of purulent material was aspirated. Following the aspiration, the hip capsule was opened through an anterior approach, and another 500 cm of purulent material was evacuated from the joint space and the posteromedial aspect of the thigh. The hip joint space freely communicated with the posteromedial adductor space and subsequently with the retroperitoneal space along the course of the iliopsoas sheath. After irrigation, the wound was closed over a drain, and a hip spica cast was applied.
The Gram stain of the hip fluid was negative, and the joint-fluid cell count had 10.75 × 10/μL WBCs with 66% neutrophils and 18,800 red blood cells, all within the normal ranges. The patient was started on intravenous vancomycin and ceftriaxone. Multiple culture specimens from the psoas abscess and hip synovium were negative. After five days, culture of the hip fluid grew rare colonies of Staphylococcus aureus in liquid media only, which were sensitive to clindamycin, gentamicin, oxacillin, sulfamethoxazole/trimethoprim (Bactrim), and vancomycin, but were resistant to erythromycin and penicillin. The patient was transitioned to oral clindamycin and ciprofloxacin therapy that was continued for six weeks. All other culture specimens, including those tested for fungus and tuberculosis, were negative. The cast was removed after six weeks; after a brief course of physical therapy, the patient resumed normal activities.
At the five-year follow-up examination, the patient had no pain and was able to participate in normal activities. The hip had a complete, painless range of movement, and the legs were of equal length. The radiograph showed a slight loss of joint-space height, acetabular subchondral sclerosis, and a mild loss of sphericity of the femoral head compared with the uninvolved left side (Fig. 3).
Proceed to Discussion >>Reference: Gamble JG. Primary Psoas Pyomyositis Presenting as Subluxation of the Hip: A Case Report. JBJS Case Connect. 2016 Mar 23;6(1):e21.
The onset and course of the iliopsoas muscle infection that caused hip subluxation in our patient were indolent and protracted. There had been a paucity of symptoms over a period of seven weeks. She had never been febrile, the WBC count was normal, and the ESR and CRP level were elevated only slightly on presentation. Early radiographs of the hip and pelvis had been normal. Most likely, the hip area became involved three weeks before presentation when it became difficult for the patient to bear weight. Erosion into the hip capsule possibly began a week before presentation, when she began to require a pillow under the knee at night to keep the hip in flexion. At presentation, a radiograph showed subluxation of the femoral head, and MRI identified a large psoas abscess that was continuous with the hip joint.
A primary psoas abscess is defined as an abscess without another detectable focus of infection. The MRI findings of a normal pelvis, spine, and surrounding tissues (appendix, colon, jejunum, kidneys, pancreas, ureters, lymph nodes, vertebral bodies, and disc spaces) indicated that this patient had a primary psoas abscess. The etiology of a primary psoas abscess remains obscure, although hematogenous seeding and lymphatic spread are at the top of the list. Secondary abscesses can arise from appendicitis, discitis, or inflammatory bowel disease, none of which were present in this case.
Septic dislocation of the hip is rare in patients in developed countries, although it has been reported in immunocompromised patients. Before the discovery of antituberculous medication, 20% of children with spinal tuberculosis developed a psoas abscess, and many of those had involvement of the hip. It was the French physician Abeille who reported the first case of nontuberculous psoas abscess in 1854. Today, Staphylococcus species are the most common organisms isolated from psoas abscesses, although tuberculosis continues to be prevalent in developing countries.
Infection in any patient is a battle between the virulence of the organism and the defense mechanisms of the host. In developing countries, poor hygiene, poor nutritional status, inadequate dental care, skin infections, anemia, endemic malarial infections, and poor health care all work in concert to lower immune resistance and increase the rate of musculoskeletal infections in children. One study estimated that 3.8% of children in Rwanda experience musculoskeletal impairment due to infection. Although our patient had spent six months in India during the previous year, she appeared healthy and well nourished, received regular pediatric care, and had none of the risk factors for immune suppression. The fact that the organism (S. aureus) grew only in liquid culture suggested a low virulence of the microorganism. We chose ultrasound-guided percutaneous aspiration as our initial treatment to drain the abscess and to rule out loculation within the muscle, which would have required retroperitoneal exploration.
In general, early diagnosis and drainage are necessary for a favorable outcome in these cases. Song et al. reported on eleven children with psoas abscess. In one case, a seventeen-month-old girl went two weeks before diagnosis; at the two-week follow-up, the child was walking without a limp. The record for a protracted presentation may be the case of a fifty-seven-year-old man who was symptomatic for three months before diagnosis, as reported by Ash et al. When he was finally treated, the femoral head and acetabulum already had been destroyed, and the patient ultimately underwent arthroplasty.
Our patient was asymptomatic at the five-year follow-up evaluation. However, the radiograph was abnormal, with a narrowed joint space, subchondral sclerosis of the acetabulum, and loss of sphericity of the femoral head, possibly making the patient more at risk for cam-type femoroacetabular impingement in the future.
In summary, our case demonstrates that a healthy child with no obvious risk factors can develop primary psoas pyomyositis due to methicillin-sensitive S. aureus (MSSA). The psoas compartment in the retroperitoneal space can accommodate a large abscess before becoming clinically evident. MRI of the pelvis and ultrasound-guided aspiration of the abscess were helpful in the management of our patient. Although the function of the hip has been normal in the short term, the changes in the shape of the femoral head occurring after the infection, the slight loss of sphericity, and the joint-space narrowing may cause problems in the future.
Reference: Gamble JG. Primary Psoas Pyomyositis Presenting as Subluxation of the Hip: A Case Report. JBJS Case Connect. 2016 Mar 23;6(1):e21.
What is the diagnosis?
Polymyositis
Iliopsoas abscess
Ewing sarcoma of the ilium
Lymphoma of the ilium
Inflammatory arthritis of the hip

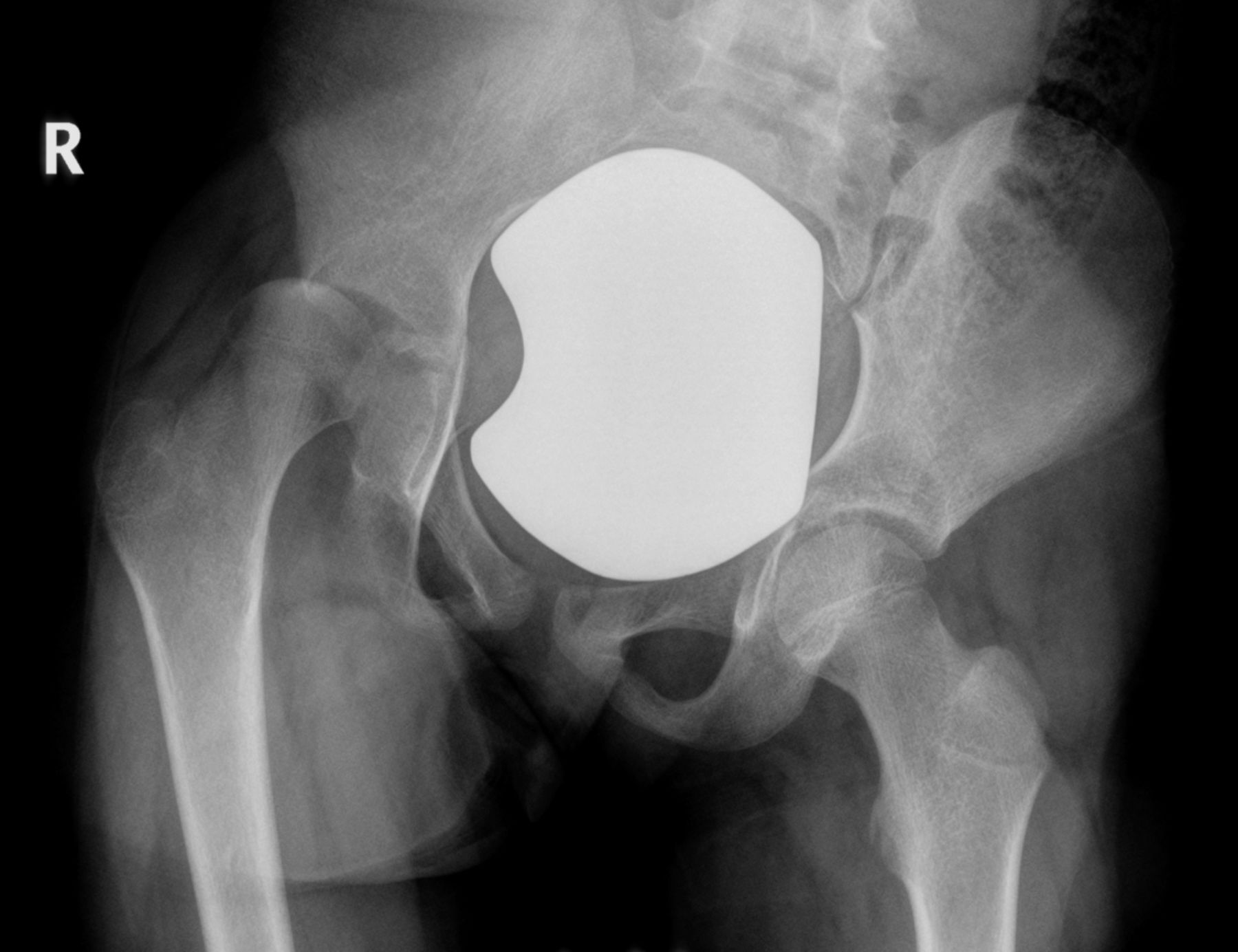

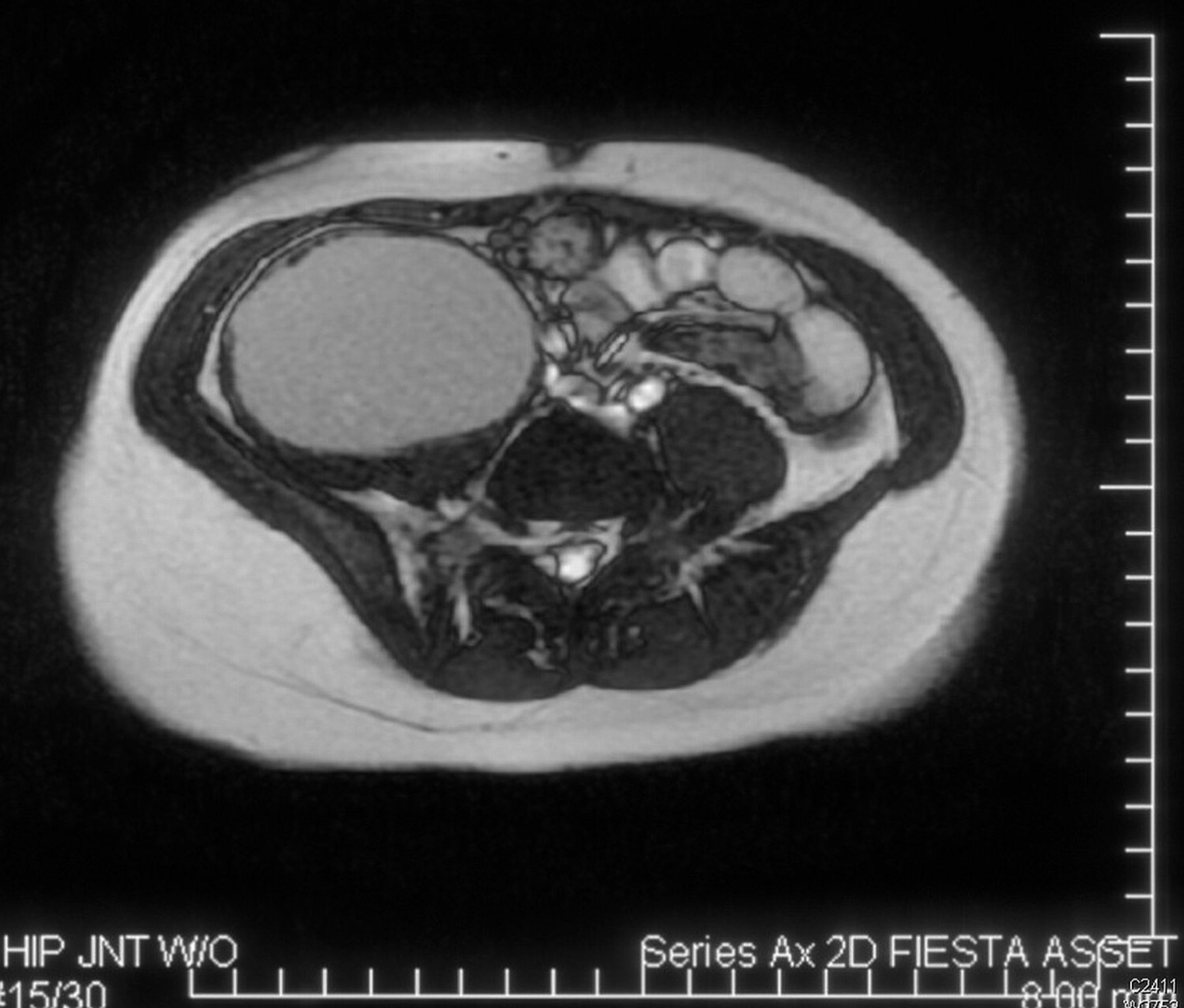
 Fig. 1
Fig. 1 Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B Fig. 3
Fig. 3