A Twenty-five-Year-Old Man with Worsening Hemoptysis
May 4, 2016
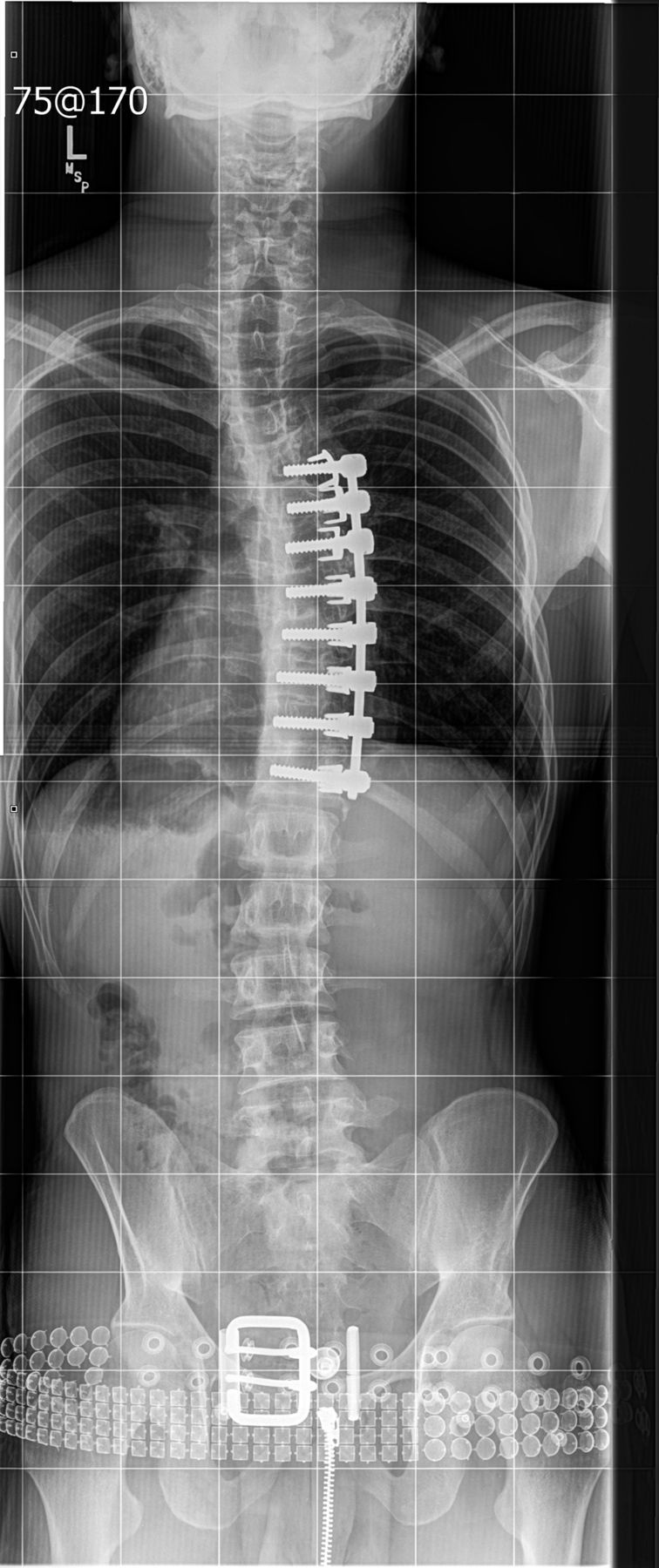
Our patient was a twenty-five-year-old man who initially had presented to a separate institution as a healthy fourteen-year-old boy with scoliotic spinal curves that had progressively worsened over eighteen months. Spinal correction and arthrodesis was performed in March 2002 with the placement of Kaneda instrumentation anteriorly on the main thoracic curve from T5 to T12 (Fig. 1). The patient progressed well into adulthood and was able to remain physically active.
Approximately three years after surgery, the patient began to note mild hemoptysis, which recurred intermittently over the ensuing seven to eight years. In July 2011, the patient presented to an outside institution with the first of two episodes of massive hemoptysis requiring hospitalization. A computed tomographic (CT) scan of the chest was obtained. A bronchoscopy identified bleeding in the right lower lobe, which required intubation to secure the airway because of massive hemoptysis. The patient underwent embolization of bronchopulmonary arteriovenous fistulae at that time. Following extubation, there was no evidence of continuing hemoptysis.
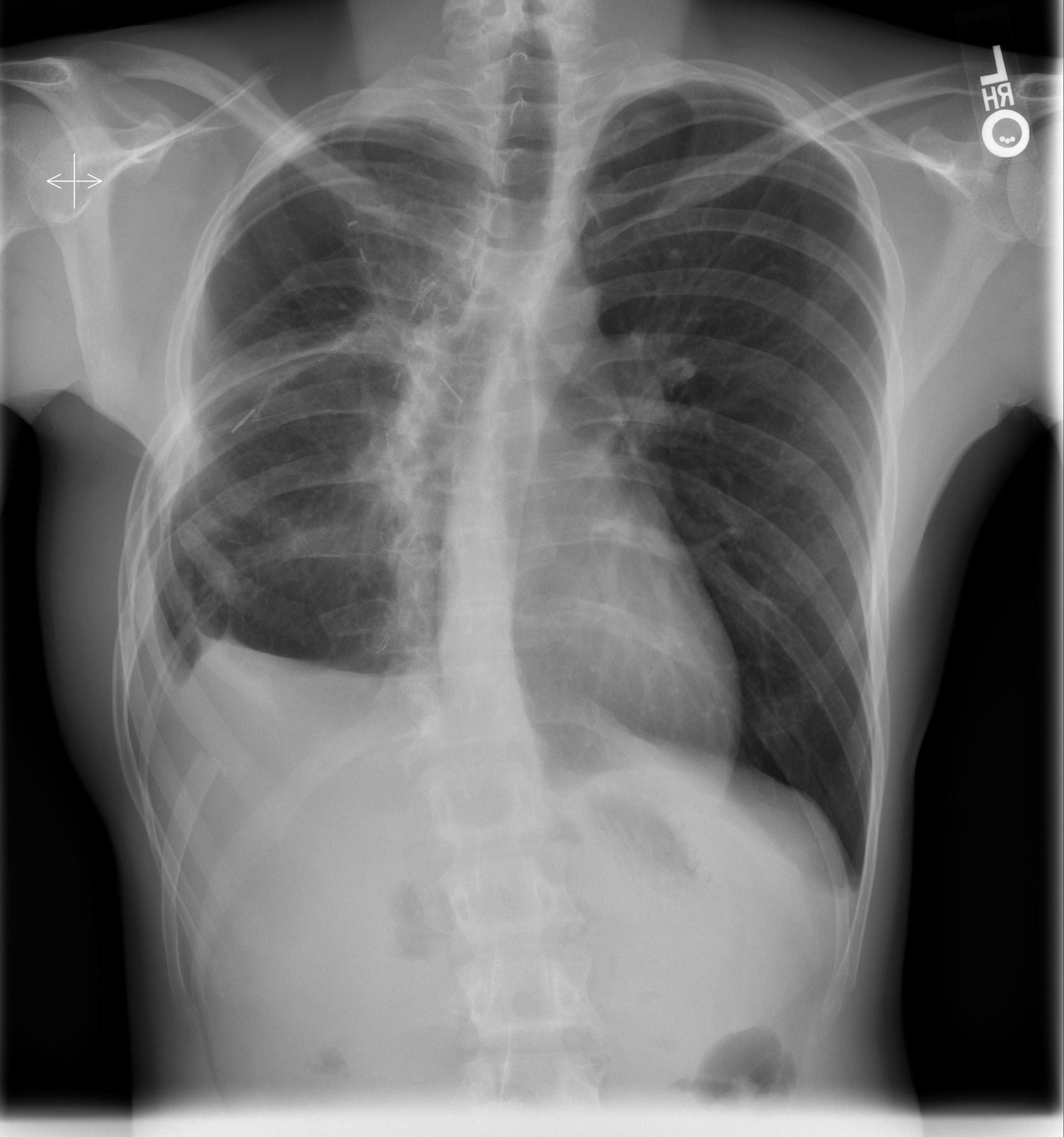
At the time of presentation to our institution in April 2012, the hemoptysis had recurred. A high-resolution CT scan of the chest, with contrast medium, was obtained (Fig. 2). There was no evidence of pulmonary embolus or arteriovenous fistulae.
The screws from T5 to T12 extended along the right perivertebral space, causing mechanical friction to the medial aspect of the right lung (Figs. 3 and 4). In addition, close examination of the radiographs showed slight proximal screw pullout. This tendency toward screw pullout at the proximal end of multilevel constructs has been previously reported in the literature and is a known propensity of anteriorly implanted instrumentation. No pseudarthrosis was present, and, given the relative frequency of this finding, we believe that proximal screw pullout was unlikely to be a contributing factor to the hemoptysis. Furthermore, adjacent atelectasis and fibrosis were noted. Subsequent embolization was performed along the medial border of the right lower lobe branch of the pulmonary artery and the bronchial arteries near the spinal instrumentation. The hemoptysis resolved again, and the patient was discharged to home.
The patient was seen for follow-up by both the thoracic surgery and orthopaedic spine surgery services. Because the anterior spinal instrumentation had eroded the lung along most of the medial border of the right lower lobe and was in proximity to a major pulmonary artery branch, and considering the history of recurrent hemoptysis, the surgical teams jointly decided to proceed with revision thoracotomy and implant removal.
In November 2012, the patient underwent repeat thoracotomy, removal of segmental anterior spinal instrumentation, and partial right lower lobectomy. The repeat right thoracotomy was initially performed through the old thoracotomy site, and resection of the sixth rib was required to provide appropriate exposure. Extensive adhesions were taken down, allowing isolation and control of the pulmonary artery. A branch of the pulmonary artery that was noted to be in intimate contact with the spinal instrumentation was isolated and controlled (Fig. 5). Adhesiolysis was then further carried out posteriorly to free the lung from the spinal implants. Figure 5 demonstrates the extensive adhesions and the intimate nature of the lung parenchyma relative to the spinal implants. Intraoperative specimens were obtained for culture.
After the implants were exposed, extraction of the rod and screws was performed, followed by removal of the staples. The most caudal staple could not safely be elevated, and it was left in situ.
Following removal of the spinal implants, the team proceeded with lung segmentectomy because of the degree of maceration to the posterior portion of the lung. A superior segmentectomy and posterior basal segmentectomy were performed. Finally, a small wedge of the upper lobe that had adhered to the implants was resected. Prior to closure, the remaining lower lobe was examined and was noted to insufflate well. A chest tube was placed, and the thoracotomy site was closed. Surgical pathological review demonstrated parenchymal fibrosis with nonspecific acute and chronic inflammatory changes and parenchymal hemorrhage. There were no definite findings indicating chronic infection or tubercular infection.
Postoperatively, the patient did well initially. However, with the development of postoperative fever, additional investigation demonstrated the development of fluid collection. Culture of specimens obtained during surgery demonstrated growth of methicillin-sensitive Staphylococcus aureus (MSSA), Neisseria, and Corynebacterium. The infectious disease service was involved, and the patient was managed with intravenous administration of micafungin, ertapenem, and vancomycin pending the results of antibiotic susceptibility testing. One week after the repeat thoracotomy, the patient was again taken to the operating theater, where he underwent right thoracotomy with decortication and removal of the remaining staple. To gain access to the most inferior staple, it was necessary to resect a portion of the tenth rib; with great effort, the remaining staple was freed and removed. Additional culture specimens were obtained, and the entire area was thoroughly debrided and copiously irrigated prior to standard closure over a chest tube and drain.
The postoperative course was uncomplicated. Culture of specimens again demonstrated growth of MSSA, and the patient was transitioned to oral minocycline prior to discharge to home. He completed six months of antibiotic treatment and returned to the orthopaedic spine, thoracic surgery, and infectious disease clinics for follow-up. There were no signs of persistent infection, no episodes of hemoptysis, and no issues other than persistent pain at the thoracotomy site. Figures 6-A and 6-B show the postoperative radiographs of the chest.
The patient was seen at twenty-six months after removal of the instrumentation because of a notable cough. He was noted to have no respiratory distress, and lung auscultation demonstrated no wheezes or rales. A chest radiograph revealed pneumonia, with no recurrence of massive hemoptysis. Scoliotic curve correction was maintained, with no progression being noted. At three months after treatment for pneumonia, the patient was seen at our hospital because of facial lacerations. The clinic note indicated that both lungs were clear to auscultation and that the patient had no chest-wall tenderness to palpation; no wheezes, crackles, or rales; and no tenderness at the thoracotomy site.
Proceed to Discussion >>Reference: Ziegler JD, Polly DW. Andrade RS. Hemoptysis Due to Anterior Scoliosis Implants: A Case Report. JBJS Case Connect. 2016 Mar 23;6(1):e20.
Anterior instrumentation for spinal arthrodesis is an established treatment for adolescent idiopathic scoliosis (AIS), with reported benefits including greater ability to affect thoracic kyphosis, correction of vertebral rotational deformity, and fusion of fewer motion segments. Posterior spine instrumentation and arthrodesis remains the standard in AIS surgery because of its consistent results and low complication rates. The reported advantages of an anterior approach have led to its rise in popularity; nonetheless, risks specific to the anterior approach include both pulmonary and cardiovascular complications.
The technically demanding nature of anterior spinal instrumentation and reports of screw penetration into vital structures such as the aorta have prompted additional investigation into the positions that such structures occupy relative to screw placement. Matsuzaki et al. reported on a patient in whom screw penetration of the thoracic aorta was noted on a CT scan six months after anterior instrumentation and described their experience with shortening the screw tip and aortic graft placement. Ohnishi et al. reported on an adult patient who had delayed aortic injury secondary to anterior instrumentation; the patient was managed with resection of the pseudoaneurysm with artificial graft placement and implant removal.
Bavare et al. reported the case of an adult patient who underwent T7 and T8 corpectomy with reconstruction using a fibular strut graft and a thoracic lateral plate and screws. The patient had early aortic laceration and was managed with primary repair and endovascular stent-grafting. Similar to our patient, their patient developed recurrent hemoptysis secondary to an arteriobronchial fistula (although much earlier). The hemoptysis was initially controlled with embolization; however, an episode of massive hemoptysis five months after the index procedure necessitated additional operative intervention, including lobectomy and implant removal.
Hemothorax, both early and late, has been reported among the rare but life-threatening complications specific to anterior scoliosis surgery. Lavigne et al. reported a case of thoracic aortic injury that presented, seven years after anterior surgical treatment of AIS, secondary to chronic erosion of the arterial wall on the prominent implant.
The case of our patient is unique in terms of both the very late nature of presentation as well as the complication of recurrent hemoptysis secondary to implant erosion of lung parenchyma. As with the pulsations of the aorta, the continuous motion of the lung against anterior spine instrumentation can result in rare but serious late complications. These serious complications further underscore the importance of meticulous surgical technique to ensure proper placement of implants and vigilance in monitoring for late iatrogenic injury. We entreat the surgical community to report their experiences with these complications in order for surgeons to understand the risks inherent to anterior instrumentation of the thoracic spine.
Reference: Ziegler JD, Polly DW. Andrade RS. Hemoptysis Due to Anterior Scoliosis Implants: A Case Report. JBJS Case Connect. 2016 Mar 23;6(1):e20.
What is the diagnosis?
Pulmonary tuberculosis
Implant encroachment on a branch of the pulmonary artery
Arteriovenous fistula of the pulmonary vein and artery
Hodgkin lymphoma
Neurofibromatosis


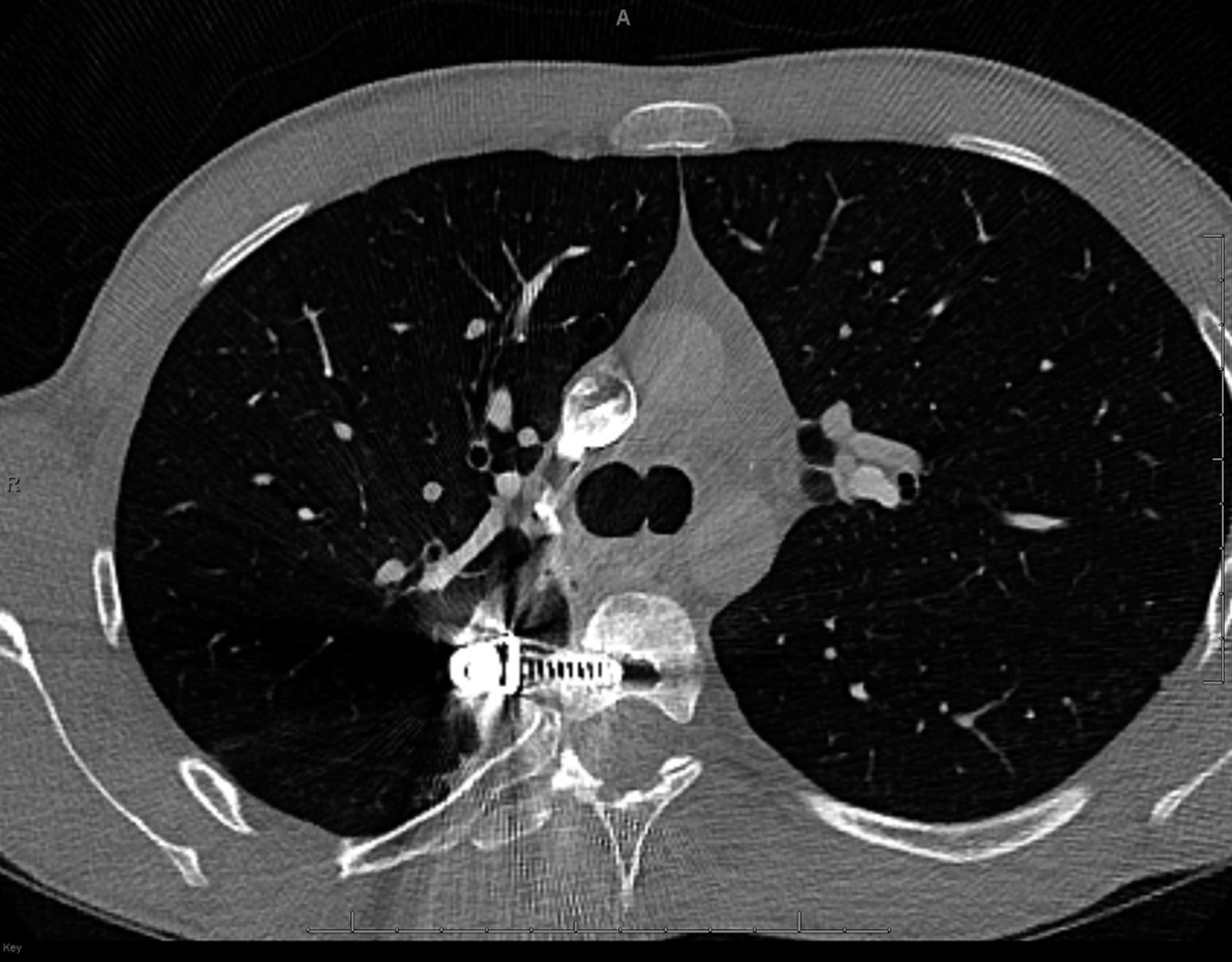
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4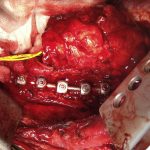 Fig. 5
Fig. 5 Fig. 6-A
Fig. 6-A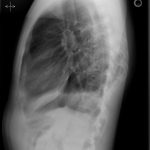 Fig. 6-B
Fig. 6-B