Fifteen-Year-Old Girl with Serious Wound Infection After Polytrauma
March 2, 2011
A fifteen-year-old, otherwise healthy girl was transferred from a rural community hospital after ejection from a motor vehicle traveling at a high speed. Major injuries included a ruptured spleen, liver laceration, bladder rupture, pneumothorax, pulmonary contusions, pelvic fractures, and bilateral femoral fractures (Fig. 1-A). A laparotomy and splenectomy were performed at the initial treatment facility prior to transfer to the regional trauma center, where the patient arrived in hypovolemic shock. After resuscitation, she underwent a repeat laparotomy and external fixation of both femora. Pelvic external fixation and preperitoneal pelvic packing were done as a part of our institutional protocol for the treatment of hemodynamically unstable pelvic fractures. The patient was then transferred to the interventional radiology suite for distal hepatic artery embolization and investigation of absent distal lower-extremity pulses, which had been initially palpable in the emergency department. The left internal iliac artery was found to be ruptured, and, after embolization, pulses returned to both lower extremities. The left femoral fracture was open (Gustilo-Anderson Grade 2), with a 4-cm wound on the left thigh and minimal soil contamination. This laceration was debrided in three separate procedures to achieve a stable-appearing wound, and it was closed primarily after the third debridement. Fourteen-hole submuscular plates were chosen over intramedullary nailing to fix both femoral fractures on the ninth hospital day (Fig. 1-B), in order to reduce the theoretical risk of further pulmonary insult given the known pulmonary injuries. During the same procedure, rotational instability of the pelvic fracture (Young-Burgess classification APC-II) was confirmed by fluoroscopy, and a six-hole pelvic reconstruction plate was applied to the pubic symphysis. Forty-eight hours after plate fixation of the left femur, the patient was returned to the operating room for exploration of excessive bleeding from previous external fixator sites and from the surgical incision on the left thigh. Laboratory studies showed no evidence of coagulopathy. Intraoperatively, no obvious vessel bleeding was noted and all tissue appeared to be viable on inspection; cultures showed mixed bacterial flora. The patient required no further operative intervention from the twelfth to the eighteenth hospital day, during which time she was hemodynamically stable and afebrile and had a downward-trending white blood-cell count. Drainage from the left lower-extremity wound gradually decreased until the nineteenth hospital day, when increased drainage, blackened areas of skin necrosis, and large bullae were noted on the thigh. The left lower extremity suddenly became cool with absent distal pulses, and the white blood-cell count fell to 0.3 × 109/L. Because of concern that she had a necrotizing infection, the patient was taken emergently to the operating room for wound exploration and debridement. A foul-smelling necrotizing infection with nonviable muscle and subcutaneous tissue surrounding the original fracture site was found intraoperatively. The hardware was removed and a guillotine amputation through the proximal part of the left thigh was performed at the level of the lesser trochanter, where viable bleeding tissue was encountered. The superficial femoral artery was noted to have a large thrombus.
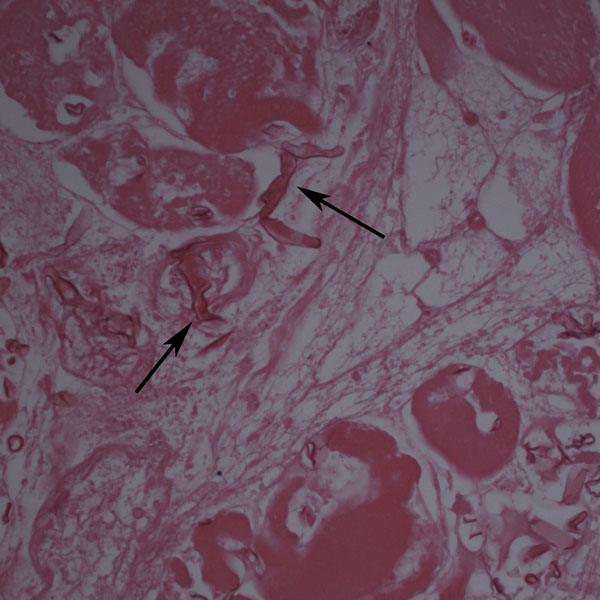
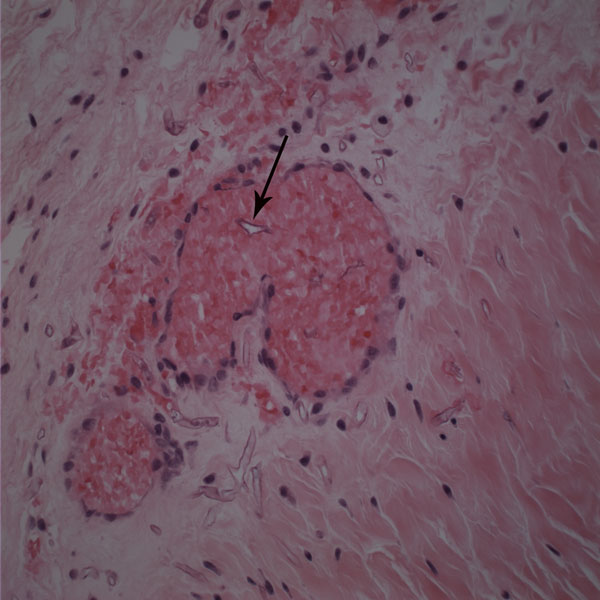
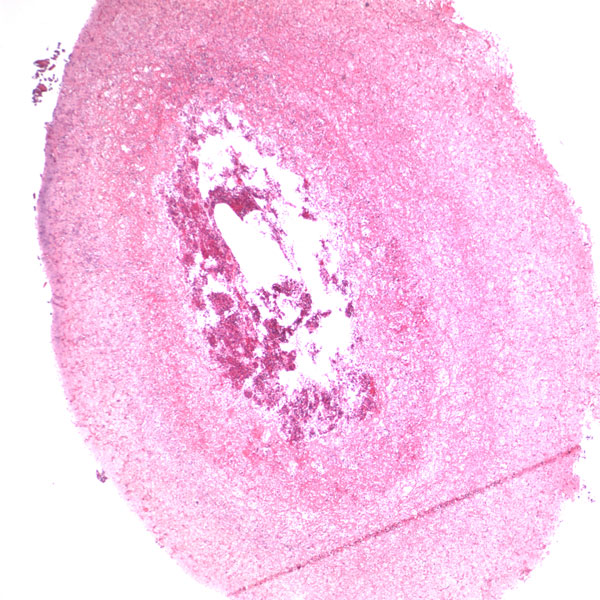
Histological examination revealed extensive necrosis of skeletal muscle with an invasive fungal infection morphologically consistent with zygomycosis (Fig. 2). Multiple vascular thromboses and fibrinoid necrosis of vessel walls secondary to fungal infection were consistent with angioinvasive disease (Figs. 3 and 4). Amphotericin-B lipid complex was administered at an initial dose of 5 mg/kg/day, and this was increased to 7.5 mg/kg/day on the second day. Specimens were submitted to the microbiology laboratory, and a white rapidly-growing zygomycetous fungus grew on culture. Cultures of bone specimens were negative for acute bacterial or fungal osteomyelitis. A left hip disarticulation was performed on the twentieth hospital day, when surgical margins from the previous amputation were reported to be positive for fungus. Foul-smelling necrotic tissue was again found intraoperatively, with progression proximally from the level of the previous guillotine amputation. The white blood-cell count fell to 0.1 × 109/L on this day. On histologic examination, the surgical margins from this procedure were again found to be positive for hyphae consistent with a zygomycete. Posaconazole was obtained on a compassionate-use basis and added to the amphotericin-B regimen at a dose of 200 mg through a nasogastric tube every six hours. The infection progressed farther proximally, and the patient underwent a hemipelvectomy with medial visceral rotation on the twenty-third hospital day. The surgical margins from this procedure were again positive for zygomycetous hyphae. The patient's respiratory status became compromised by the development of acute respiratory distress syndrome, multiorgan failure developed, and a profound neutropenia compromised the immunologic status. During the last eight days of the hospital course, the white blood-cell count remained between 0.1 and 0.3 × 109/L. On the twenty-fourth hospital day, the patient was requiring progressive vasopressor support, with a worsening cardiovascular status, acidosis, and increasing ventilatory need. She died after withdrawal of the cardiovascular support at the family's request, on the twenty-fifth hospital day. Postmortem speciation of this Zygomycetes infection confirmed the diagnosis as a variant of Rhizopus microsporus. Lack of sporulation of the isolate precluded identification by traditional methods, so the sample was forwarded to a reference laboratory for DNA sequencing. Techniques for DNA sequencing utilized the internal transcribed spacer (ITS) and D1/D2 sequences to search the National Center for Biotechnology Information (NCBI) nucleotide database with use of the NCBI BLASTN (basic local alignment search tool nucleotide) program. The results showed the greatest percent identity to Rhizopus microsporus variant chinensis (ITS identity = 98%, D1/D2 identity = 99%); however, Rhizopus microsporus variant oligosporus (98% by ITS) and Rhizopus microsporus variant microsporus (99% by D1/D2) showed a similar level of identity.
Proceed to Discussion >>Reference: Koonce RC, Price CS, Sutton DA, Wickes BL, Montero PN. Lower-extremity zygomycosis in a patient with traumatic injuries. A case report. J Bone Joint Surg Am. 2009;91:686-92.
Zygomycosis, also called mucormycosis, is an aggressive fungal infection found rarely in patients who have sustained traumatic injuries. Traumatic contact with an extremity may introduce the fungi through the mucocutaneous barrier, and progression of the infection can be fatal if vascular invasion, tissue infarction, and necrosis occur. Zygomycosis is usually found in immunocompromised individuals, but trauma may introduce and potentiate infection in patients without preexisting risk factors. Although it is a rare complication of trauma, identification of the infection is important because the overall mortality rate from documented cutaneous zygomycosis inoculation has been reported to be as high as 31%. Successful treatment depends primarily on early diagnosis and surgical debridement and secondarily on administration of appropriate antifungal medications. Zygomycosis is the third leading cause of invasive fungal infection after candidiasis and aspergillosis. Caused by a subset of ubiquitous molds within the class Zygomycetes, these fungi are found readily in soil, vegetation, and decaying matter. Some authors have called it the most aggressive and fatal of all fungal infections. Its estimated incidence is 1.7 cases per 1,000,000 inhabitants per year, and several reports suggest its overall incidence is on the rise due to HIV/AIDS, the use of anticancer drugs, and the widespread use of immunosuppressive medications. The fungal class Zygomycetes is divided into two orders: Mucorales and Entomophthorales. Entomophthorales infection typically presents as a nonfatal, chronic subcutaneous infection without angioinvasion. Genera from the order Mucorales are capable of causing a fulminant angioinvasive infection with high rates of morbidity and mortality. This type of infection is termed either mucormycosis or zygomycosis. The discussion regarding which term is correct to describe this group of disease is complex and has historical and contemporary roots; one term has not been generally agreed on. Fungi in the order Mucorales enter the human host through inhalation, percutaneous inoculation, or ingestion. The most commonly affected locations include the sinuses, lungs, skin, brain, gastrointestinal tract, and heart. Cutaneous zygomycosis is the third most common presentation overall (accounting for 19% of all documented cases) and the most common clinical presentation in patients who have sustained traumatic injury. Bone and joint infection are rare. Following traumatic inoculation by contaminated soil, members of the order Mucorales invade deep tissue and are met by phagocytes. In the healthy host, phagocytes typically kill fungal spores. Healthy individuals are often colonized and avoid invasion, but patients with neutropenia or phagocyte dysfunction are at risk if this first-line defense fails. If spores avoid phagocytosis, vessel invasion follows with adherence to endothelial cells. Invasion of vessels leads to ischemia and thrombosis and may progress to a necrotizing infection. Hematological spread and septic thromboembolism result in disseminated disease and multiorgan involvement. Immunocompromised patients are at higher risk for invasion. Specific predisposing conditions reported in the literature include malignant tumors, diabetes, iron therapy, renal failure, organ transplantation, metabolic acidosis, neutropenia, trauma, and burns. Trauma itself has been shown to cause an immunocompromised state. In addition to the development of severe systemic inflammatory responses such as acute respiratory distress syndrome, disseminated intravascular coagulation, and systemic inflammatory response syndrome, the dysfunction of immune cells renders a traumatically injured patient more susceptible to local bacterial and fungal infection. Both cell-mediated and humoral immune mechanisms are substantially affected by the injury and secondary insults such as surgery. Our severely injured patient was immunocompromised for several reasons, and there were several potential sources of bacterial and fungal infection in addition to initial traumatic fungal inoculation. Ventilator dependence, multiple central lines, implanted hardware, and open injuries were all potential sources, and systemic neutropenia rendered her unable to stave off infections. The initial presentation of zygomycosis infections is nonspecific and has many forms, including erythema, pustules, blisters, nodules, necrotic ulcerations, ecthyma gangrenosum-like lesions, and necrotizing cellulitis. Superficial and deep forms of infection have been recognized. The superficial form, caused by minor trauma, is less common, is generally painless, and presents with milder symptoms. The deep or gangrenous form may include large zones of blackened tissue or a cotton-like growth with necrotic foul-smelling tissue. Zygomycosis is most easily diagnosed by identifying its characteristic morphologic features on biopsy. Histopathologic examination demonstrates sparsely septate, broad, thick-walled, ribbon-like hyphae, often branching at right angles from the main trunk (Fig. 2) with angioinvasion and surrounding tissue infarction (Fig. 3) in permanent or frozen-tissue sections. Vessels may be occluded by mycotic thrombi (Fig. 4). Swabs or fluid specimens are usually inadequate, and tissue specimens into which extensive bleeding has occurred are the best samples for culture. Species identification is achieved by means of recovery of the etiologic agent in culture and examination of the isolate's histologic features. Isolates that fail to sporulate, as in our case, preclude identification by this method. A more recent alternative to morphologic identification is molecular sequencing of the isolate. The two most common regions for species identification are the ITS region and the D1/D2 region, both of which are informative and can be amplified from unknown fungi with use of universal primer pairs. Using DNA sequencing technologies, we were able to confirm the identity of the fungus as a zygomycete most consistent with Rhizopus microsporus, but only postmortem. While species identification may confirm the diagnosis, it is often of academic interest only since treatment decisions are based on clinical and histopathologic findings. In the future, species-specific medical therapies may be available. The infection in our patient presented on the nineteenth day in the hospital, when large skin bullae, a pulseless extremity, and necrotic blackened tissue were noted. Overt clinical presentation of a necrotizing infection preceded pathologic identification and fungal cultures. Excessive bleeding from the surgical site on the left thigh without an obvious source or coagulopathy was present on the eleventh hospital day, and this may have represented the early stages of angioinvasion. This case emphasizes the challenge of identifying the disease before extensive angioinvasion and necrosis occur, and the importance of a high level of clinical suspicion. Treatment of an invasive zygomycosis begins with early and aggressive surgical debridement of all necrotic tissue. Minimal surgical debridement has been performed successfully in patients with superficial zygomycosis, but wide or radical excision should be carried out for deeper, necrotizing infections. The current literature offers no reliable guidelines regarding how much surrounding tissue to debride. Some authors have recommended assessing the macroscopic appearance of the soft tissues, and performing debridement until viable bleeding tissue is encountered. This was not a reliable indicator of the extent of the disease in our patient, as surgical margins were consistently positive for Zygomycetes. This was likely due to local hematogenous spread after angioinvasion. The challenge in achieving successful surgical treatment is determining the location and extent of angioinvasion. Once angioinvasion occurs in a major vessel to a limb, adequate debridement of the vessel may result in a dysvascular limb, necessitating amputation. The literature contains recommendations for the use of frozen-section analysis for the diagnosis of acute invasive fungal rhinosinusitis, with a reported diagnostic sensitivity of 0.84 and specificity of 1 when compared with permanent sections as the gold standard. Although there is no reported evidence to support this practice when amputation is being considered in an extremity, frozen-section evaluation of tissue samples from the proposed amputation site may be useful. Medical treatment of zygomycosis is second to surgical debridement in order of importance. Several commonly prescribed antifungal agents, (e.g., voriconazole, caspofungin, and fluconazole) are not effective against the Zygomycetes. High-dose amphotericin B (either liposomal amphotericin B or amphotericin-B lipid complex) has been the preferred antifungal treatment, but its use is limited by its many known toxicities and questionable efficacy against the zygomycetes. Common adverse reactions include hypokalemia, renal impairment, and infusion-related intolerance reactions. Posaconazole is a newer triazole antifungal agent that has been shown to be effective in several patients who did not respond to amphotericin B. Its clinical efficacy is supported by in vitro antifungal susceptibility data as well as animal models. It has a favorable pharmacokinetic and adverse-effect profile, but it has only recently become available in the United States as a Food and Drug Administration-approved agent for a limited spectrum of fungal infections, and only as an oral suspension. Current recommendations support the use of posaconazole in combination with amphotericin B, but more studies are needed before posaconazole can be recommended as the primary medical therapy. There are currently no data to support use of antifungal agents empirically for patients with soil-contaminated wounds, given the toxicity of these agents. It is not clear that the benefits of this broad treatment outweigh the risks, and thus positive histologic findings or cultures should precede antifungal administration.
Reference: Koonce RC, Price CS, Sutton DA, Wickes BL, Montero PN. Lower-extremity zygomycosis in a patient with traumatic injuries. A case report. J Bone Joint Surg Am. 2009;91:686-92.
Streptococcal necrotizing fasciitis
Zygomycosis or mucormycosis
Methicillin-resistant Staphylococcus aureus infection
Clostridial infection



 Fig. 1-A
Fig. 1-A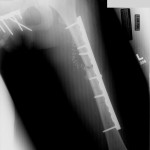 Fig. 1-B
Fig. 1-B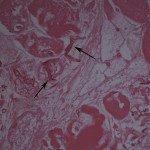 Fig. 2
Fig. 2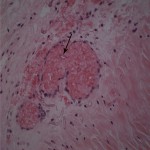 Fig. 3
Fig. 3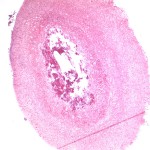 Fig. 4
Fig. 4