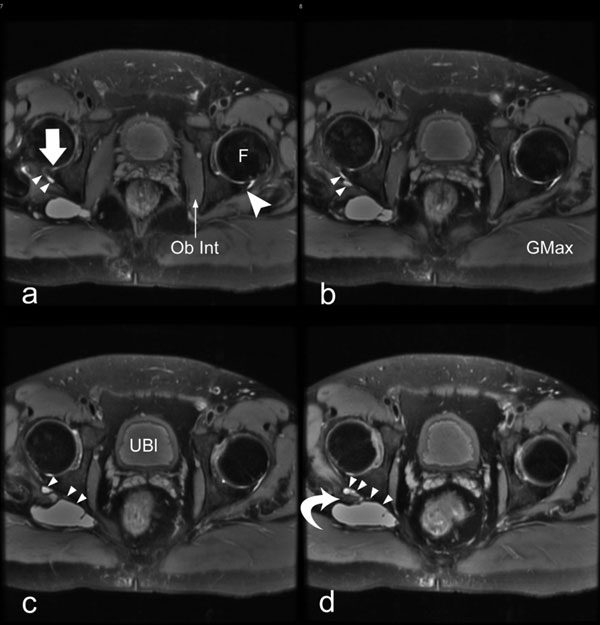
A thirty-eight-year-old man presented with a four-year history of gradually worsening pain in the lower back, radiation of the pain down both lower limbs, and intermittent paresthesias. These symptoms began following an automobile accident. He was otherwise in good health. After having undergone several years of conservative treatment that included anti-inflammatory medication and physiotherapy, the patient was referred to the spinal team at our institution. A clinical diagnosis of sciatica was made, and a magnetic resonance imaging scan of the lumbar and sacral spine was acquired. The magnetic resonance imaging scan of the lumbar spine showed a posterior-central prolapse of the disc between L4 and L5, with narrowing of the thecal sac on the left side. The sacroiliac joints and the disc between L3 and L4 as well as the disc between L5 and S1 were normal. The patient was given an epidural injection of steroid medication, which temporarily relieved the pain in the back and left lower limb but did not relieve the pain that radiated down the right lower limb. A repeat magnetic resonance imaging (MRI) scan of the lumbar spine and sacroiliac joints was acquired twelve months later. Although the newer scan showed no further changes in the spine, it did reveal a possible lesion just posterior to the right acetabulum. This lesion could not be evaluated in detail because it was at the edge of the field of view. The patient was then referred for evaluation of the hip. He had deep gluteal pain that radiated down the right lower limb, which made walking very painful. On physical examination, the patient had a positive straight-leg-raising test at 25° to 30°, no pain on abduction, and normal motor, sensory, and reflex function in the lower limb. A more detailed MRI scan of the pelvis was acquired (Fig 1).
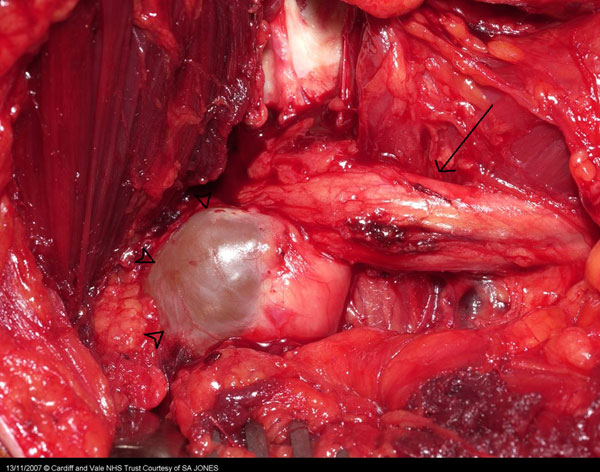
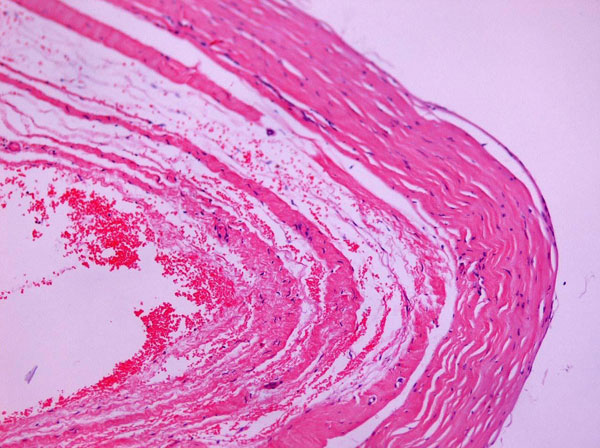
The MRI confirmed the presence of a 5.8 × 2.2 × 3.8-cm multilobulated mass deep to the right gluteus maximus muscle and inferior to the piriformis muscle. The mass had internal lobularity and septations, with the tail proceeding anteriorly to the region of the posterior aspect of the right labrum (Fig. 1). The sciatic nerve was seen to cross the anterior aspect of the lesion. We concluded that this multilobulated, cystic structure was most likely a posterior paralabral cyst and the cause of the sciatica. No obvious damage to the labrum was seen on the scan. We recommended to the patient that he undergo excision of the cyst. A posterior approach to the hip was used, but the insertions of the short external rotators were preserved. The large cystic lesion was found and was noted to be compressing the right sciatic nerve. The lesion was aspirated, and 15 mL of straw-colored fluid was removed. The sciatic nerve was identified proximally and distally, and the cyst was carefully dissected from it (Fig. 2). A benign, fibrous-walled cyst, largely devoid of lining epithelium, was identified on histological examination of the specimen (Fig. 3). Postoperatively, the patient noted improvement in pain almost immediately. By one week after the operation, there was little pain at the surgical site, no symptoms or signs of sciatica, a full range of hip movement, and no neurological deficit. At the six-week follow-up, the patient's symptoms had completely resolved.
Proceed to Discussion >>Reference: Jones HG, Sarasin SM, Jones SA, Mullaney P. Acetabular paralabral cyst as a rare cause of sciatica. A case report. J Bone Joint Surg Am. 2009;91:2696-9.
To our knowledge, there have been only two reported cases of large acetabular paralabral cysts causing sciatica and none reported in the English-language orthopaedic surgical literature. Synovial cystic lesions are commonly found in large joints, such as the shoulder, knee, and hip. Such lesions, when occurring in the hip and shoulder joints, are often associated with labral tears and are known as labral or paralabral cysts according to their anatomical relationship with the joint. In the hip, tears of the labrum can cause loss of congruity between the femoral head and the acetabulum, thus leading to increased intra-articular pressure. This elevated pressure can force synovial fluid into the acetabulum or the surrounding soft tissues, causing a paralabral cyst. These cysts can produce joint instability and pain. There have been many reports of juxta-articular cysts causing compression of adjacent neurovascular structures. Glenoid paralabral cysts of the shoulder have been reported to be associated with compression of the axillary and suprascapular nerves, elbow or wrist ganglia have been associated with radial nerve compression or ulnar nerve compression in the cubital tunnel, and large paralabral cysts, which are much less common than other cysts and occur around the hip joint, have been associated with compression of the vascular and neurological structures, such as the femoral vein and artery and the sciatic nerve. Sciatica is a common condition, affecting as many as 40% of adults at some time in their lives. It is usually caused by prolapse of the lumbar disc between L5 and S1. However, compression of the sciatic nerve along any part of its route may cause symptoms, and other causes of sciatica should be considered. Nondiscogenic sciatica can be categorized as either intrapelvic or extrapelvic. Reports of intrapelvic causes include tumors, aneurysms, endometriosis, and anorectal abscesses. Extrapelvic causes (distal to the sciatic notch) include aneurysms or pseudoaneurysms of the gluteal artery, tumors, gluteal abscess, avulsion fracture of the ischial tuberosity, and paralabral cysts. There has also been a reported case of sciatic neuropathy secondary to migration of a trochanteric wire following a total hip arthroplasty. Cystic lesions that occur about joints are either ganglial or synovial in nature. Ganglial cysts are typically lined with connective tissue and contain mucinous fluid, while synovial cysts are lined with synovial cells, contain fluid, and may communicate with the joint. Synovial cysts that involve the hip are usually associated with the iliopsoas bursa, the largest bursa about the hip and one that communicates with the hip joint in approximately 14% of patients. These cysts rarely cause hip pain but may be associated with disease in which there is a component of hip instability, such as osteoarthritis, developmental dysplasia of the hip, or a trauma-induced condition. Labral tears are also associated with conditions in which there is loss of joint stability. The cyst is thought to form as the result of elevated intra-articular pressure. Although no labral tear was seen in our patient at the time of surgery, we propose that the cyst in our patient resulted from the hip trauma sustained during the motor-vehicle accident a few months before the onset of symptoms. In patients who have a paralabral cyst that is causing only hip pain, remote trauma seems to be strongly correlated. There have been numerous reports of paralabral cysts associated with symptoms of pain and "clicking" in the hip; however, it is very rare for these synovial cysts to become large enough to impinge on adjacent neurovascular structures. Although it is commonly diagnosed, sciatica may have more obscure causes. Greater awareness of the less common etiologies, especially in a patient with a history of trauma or a diagnosis such as developmental dysplasia of the hip or osteoarthritis, may more quickly lead to the appropriate diagnosis.
Reference: Jones HG, Sarasin SM, Jones SA, Mullaney P. Acetabular paralabral cyst as a rare cause of sciatica. A case report. J Bone Joint Surg Am. 2009;91:2696-9.
Nerve sheath tumor
Torn acetabular labrum with displaced fragment
Acetabular paralabral cyst
Intramuscular hemangioma
Lipoma

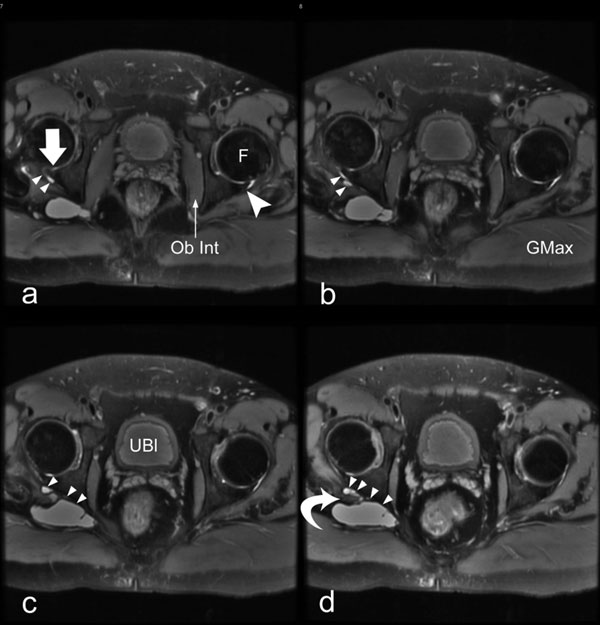
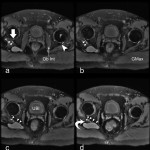 Fig. 1
Fig. 1 Fig. 1
Fig. 1 Fig. 2
Fig. 2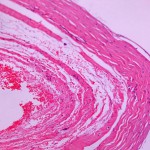 Fig. 3
Fig. 3