Pain in the Knee of a Fourteen-Year-Old Boy Following a Direct Blow to the Suprapatellar Area
October 20, 2010
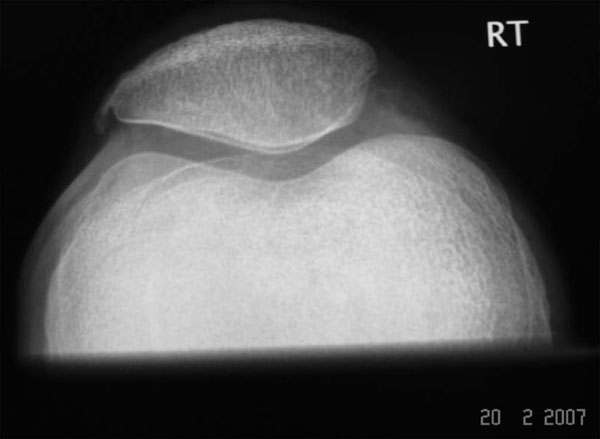
A fourteen-year-old boy presented to our institution after sustaining a direct blow to the suprapatellar area of the right knee. The injury occurred as a result of the knee striking a concrete block while the patient was swinging on a rope. Following the injury, the boy was unable to walk and could not move the right knee. Examination revealed bruising of the anterior aspect of the knee and an unusual shape of the patella. The patient could neither perform a straight leg raise nor flex the knee. Radiographs of the knee are presented in Figures 1-A and 1-B.
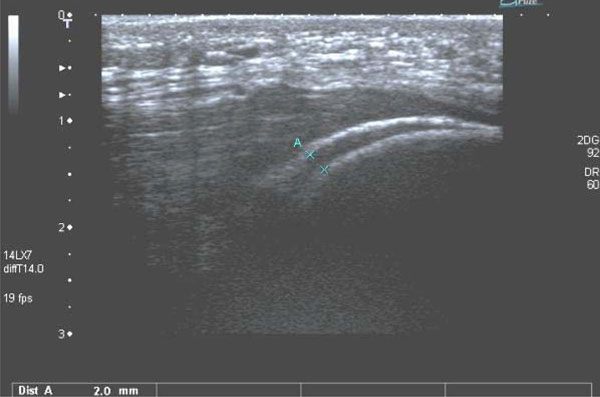
Radiographs revealed an intra-articular dislocation of the patella (Figs. 1-A and 1-B). In the lateral projection (Fig. 1-B), the patella was seen to be lying in a transverse position, with the articular surface facing in a distal direction. With the patient under intravenous morphine sedation, the patella was relocated in the emergency department by an orthopaedic surgeon. The patient was placed in the supine position, and the hip was flexed to approximately 60° to relax the quadriceps muscle. An assistant maintained the hip in flexion while manipulation of the patella was performed. The knee was extended and the prominent patella was gripped between the thumb and fingers and gently levered out of the joint while the knee was flexed and extended through an arc of 10° to 15° of motion. The restoration of normal patellar contour and patellofemoral relationship was noted clinically following the reduction. Radiographs made after the reduction revealed relocation of the patella in the correct anatomical position (Fig. 2-A) and a small hemarthrosis (Fig. 2-B). The patient could not perform a straight-leg raise following relocation of the patella even with an extension knee splint in place. Further review of the radiographs revealed a sleeve fracture of the superior pole of the patella with a possible indentation in the quadriceps tendon (Fig. 2-B). Rupture of the quadriceps tendon was suspected. An ultrasound scan of the knee (Fig. 3) was performed, which confirmed the presence of a sleeve fracture of the superior pole of the patella and showed that the quadriceps tendon was intact. The fracture line was noted to be aligned with the superior pole of the patella, with a fracture gap of 2 mm. As the fracture gap was only 2 mm, we elected to manage the injury nonoperatively with immobilization of the knee in a knee splint in extension. Radiographs made four weeks following the injury revealed a thin rim of callus, suggesting early union of the fracture. Knee immobilization was discontinued at four weeks, at which time active flexion and extension exercises of the knee were initiated. By ten weeks after the injury, the patient had regained full knee movement without any quadriceps weakness. Radiographs (Figs. 4-A and 4-B) revealed fracture union without a double patella sign (i.e., a radiographic indication of the presence of a widely separated sleeve fracture that, during the healing process, formed extra new bone resembling a patella; a knee with this type of healed fracture appears radiographically as if it has two patellas).
Proceed to Discussion >>Reference: Maripuri SN, Mehta H, Mohanty K. Sleeve fracture of the superior pole of the patella with an intra-articular dislocation. A case report. J Bone Joint Surg Am. 2008;90:385-9.
Indirect injury to a flexed knee seems to be the most common mechanism of injury in sleeve fractures of the inferior patellar pole. We believe that sleeve fractures of the superior patellar pole result from direct injury to the suprapatellar area. We hypothesize that if the force continues after the creation of a sleeve fracture, the patella is pushed down, resulting in an intra-articular dislocation. When they occur simultaneously, a rare avulsion fracture of the superior patellar pole and an intra-articular dislocation of the patella represent two elements along the same continuum of injury. In the case of our patient, after performing the closed reduction, we assessed the patella with anteroposterior and lateral radiographs, and we confirmed the satisfactory relocation of the patella as indicated by a normal patellofemoral relationship, an absence of patellar tilt, and an absence of patella alta. There was no radiographic evidence of osteochondral fragments or loose bodies in the joint. After the sleeve fracture of the superior patellar pole was identified on plain radiographs, the diagnosis was confirmed with ultrasound examination. A high index of suspicion and prompt diagnosis are the keys to successful treatment of this injury. Ultrasound helps to confirm the integrity of the quadriceps and reduction of the sleeve fracture. Magnetic resonance imaging has been shown to be helpful in determining the extent of cartilaginous injury. If the gap between the sleeve fracture and the superior pole is ≤2 mm, nonoperative treatment is an option. Open reduction and internal fixation is recommended when the fracture gap is >2 mm. The patellar fracture gap can easily be seen and accurately measured with the use of ultrasound. Trikha et al. documented that ultrasound findings were well correlated with operative findings. Although several authors have reported that magnetic resonance imaging is superior to other imaging modalities in identifying bone bruises, osteochondral fragments, and internal derangements of the knee, it is not clear when magnetic resonance imaging is indicated. Shea et al. obtain magnetic resonance imaging scans for immature athletes early in the evaluation of patellar dislocation, but they do not routinely obtain magnetic resonance imaging scans for nonathletes unless there are concerns about osteochondral injury or intra-articular fragments, and the patients are advised that future knee dysfunction may warrant further imaging evaluation. In all cases, regular follow-up examinations seem mandatory to identify these problems. The diagnosis of a sleeve fracture of the superior patellar pole could be missed for several reasons: (1) With this fracture, patella alta is not seen as it is with sleeve fractures of the inferior pole; (2) The small size of the fracture fragment can be overlooked on plain radiographs; and (3) The fracture may not be seen on plain radiographs at all, as the sleeve may only consist of periosteum and cartilage. Kumar and Knight suggested that the anterior tilt of the patella is a characteristic feature in sleeve fractures of the superior pole. This sign was noted in both of the previously reported patients but was absent in our patient, highlighting the fact that the absence of this sign cannot rule out a fracture of the superior patellar pole. When a fracture of the superior patellar pole is clinically suspected, we recommend the use of ultrasound or magnetic resonance imaging scans to help identify or rule out the injury. Most of the reported patellar sleeve fractures and intra-articular patellar dislocations have been managed surgically. Bishay used open reduction and figure-of-eight sutures to repair a sleeve fracture of the superior pole, followed by five weeks of plaster immobilization. Kumar and Knight used Ethibond sutures placed through the quadriceps and attached to bone anchors in the patella. Although patellar sleeve fractures with a displacement of ≤2 mm have been treated nonoperatively in an extension splint in the past, the results of treatment were reported to be unsatisfactory. Five of the previously reported intra-articular patellar dislocations were relocated nonoperatively. The nonoperative relocation methods described in the literature involve the use of immense force, but the method we describe is simple and does not require great force. However, we recommend this manipulation, which is done with the patient under conscious sedation, only if good relaxation and pain relief are achieved. The same procedure can be performed with the patient under general anesthesia. The most important step in the reduction is maintaining hip flexion, as this relaxes the quadriceps and allows the patella to be mobilized. The case of our patient is unique in that we managed the intra-articular dislocation and the subsequently detected patellar sleeve fracture nonoperatively with a successful outcome. Awareness of this rare combination of injuries will help in the early diagnosis and appropriate treatment of this condition.
Reference: Maripuri SN, Mehta H, Mohanty K. Sleeve fracture of the superior pole of the patella with an intra-articular dislocation. A case report. J Bone Joint Surg Am. 2008;90:385-9.
Sleeve fracture of the inferior pole of the patella with patellar dislocation
Patellar dislocation with associated medial retinacular tear
Sleeve fracture of the superior pole of the patella with an intra-articular patellar dislocation
Quadriceps muscle rupture with inferior patellar displacement



 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B Fig. 3
Fig. 3 Fig. 4-A
Fig. 4-A Fig. 4-B
Fig. 4-B