A Sixty-two-Year-Old Man with Marked Knee Pain
November 3, 2010
A sixty-two-year-old native-born Filipino man, 167 cm tall and weighing 77 kg, presented in January 2004 with symptoms of fever and a productive cough of several weeks' duration. The patient had immigrated to the United States in 1955 and had become a U.S. citizen, but he still frequently visited the Philippines. After a positive Mantoux skin test, further workup included normal chest radiographs. A diagnosis of pulmonary tuberculosis was made by sputum culture and the patient began treatment with isoniazid, rifampin, ethambutol, and moxifloxacin. Moxifloxacin had been substituted for pyrazinamide due to the patient's history of gout. Knee symptoms of mild pain and swelling began in April 2004. At that time, the patient was an independent community walker. By July 2004, knee pain and swelling had increased substantially. Serum inflammatory markers were elevated: the erythrocyte sedimentation rate was 121 mm/hr (normal, 0 to 10 mm/hr), and the C-reactive protein level was 7.32 mg/dL (73.2 mg/L) (normal, <0.75 mg/dL [7.5 mg/L]). An aspirate of synovial fluid was notable for a white blood-cell count of 7650/mm3 (7.7 × 109/L) and for the presence of monosodium urate crystals. Radiographs of the knee showed erosive arthritis involving all three compartments (Fig. 1).
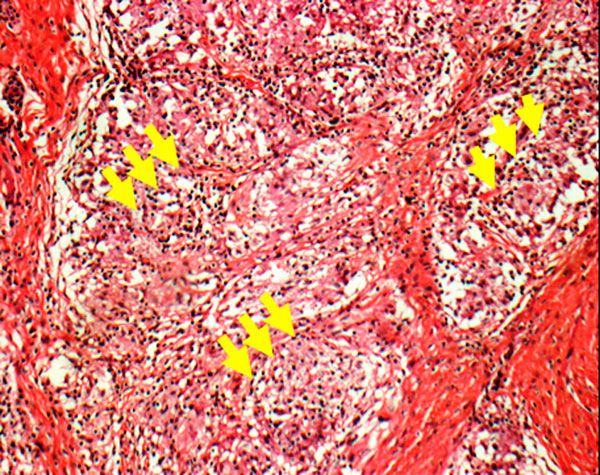
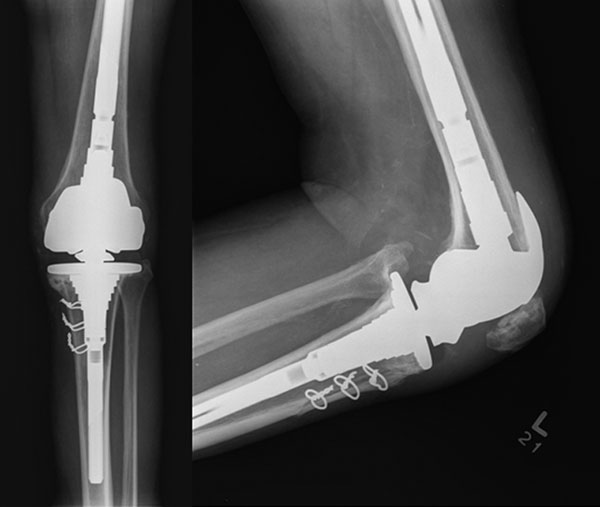
The knee was treated with an intra-articular corticosteroid injection, but the knee symptoms failed to improve. One month after the aspiration of synovial fluid, the results of culture confirmed that the knee was infected with Mycobacterium tuberculosis. With continuation of the four-drug medical therapy, the pulmonary tuberculosis resolved; however, the patient became increasingly disabled by knee pain and stiffness. By November 2004, the patient required a wheelchair for mobility outside the home. By November 2004, the left knee was swollen, warm to palpation, and painful to manipulation. The patient had a 20° flexion contracture of the knee with no extensor lag and with maximum flexion to 90°. There was varus deformity with gross knee instability with insufficiency of the cruciate and collateral ligaments. Knee radiographs showed tricompartmental joint destruction with extensive soft-tissue edema and calcification, erosion of the femoral and tibial condyles, and osteopenia (Fig. 2). Magnetic resonance imaging demonstrated complete destruction of the articular surfaces, multiple periarticular fluid collections, and hypertrophic synovitis, including a lobulated periarticular soft-tissue mass posteriorly (Fig. 3). In January 2005, the patient underwent surgical debridement of the knee through a combined posterior and anterior approach. The large granulomatous mass was excised from the popliteal fossa, and all of the infected posterior capsule, synovium, and bone was thoroughly debrided. After closure of the posterior wound, the patient was turned supine and, through a medial parapatellar arthrotomy, a complete synovectomy and osseous debridement were performed. Debridement required removal of the entire joint, including 2 to 3 cm of metaphyseal femoral and tibial bone proximal and distal to the joint line as well as 1 cm of patellar bone. An antibiotic-laden cement spacer was placed in the joint-space defect. Initially, we added isoniazid to Palacos bone cement (Zimmer, Warsaw, Indiana). However, isoniazid (in both powder and liquid forms) inhibited cement polymerization. Therefore, a cement spacer containing tobramycin (2.4 g of tobramycin per 40 g of bone cement) and vancomycin (2 g of vancomycin per 40 g of bone cement) was placed. The wound was closed over drains and the leg was placed in a cylinder cast. Histopathologic analysis of multiple biopsy specimens from the knee confirmed extensive chronic granulomatous synovitis with palisading histiocytes and central necrosis consistent with chronic mycobacterial infection (Fig. 4). The synovial tissue also revealed rare tophaceous deposits. Special stains failed to reveal any acid-fast bacilli, and multiple acid-fast tissue cultures were negative. Postoperatively, the patient was treated with an additional twelve months of isoniazid, rifampin, and moxifloxacin. While the spacer remained in situ, the patient was kept non-weight-bearing to minimize the risk of additional bone loss and spacer migration. After a discussion of the risks and benefits of both arthrodesis and arthroplasty, he opted for a total knee arthroplasty. Sixteen months after the resection arthroplasty, the serum inflammatory markers had returned to normal and a culture of the synovial fluid was negative for Mycobacterium tuberculosis. Although a repeat magnetic resonance imaging scan of the knee demonstrated a focal area of inflammation at the lateral aspect of the femur, a computed tomography-guided biopsy of tissue from this area revealed no residual tuberculosis infection. In April 2006, seventeen months after the resection arthroplasty, the patient underwent total knee arthroplasty. Exposure required an osteotomy of the tibial tubercle. Press-fit metaphyseal sleeves, intramedullary stem extensions, and a rotating hinge prosthesis (S-ROM; DePuy, Warsaw, Indiana) were utilized. A V-Y lengthening of the quadriceps tendon was performed to relax the contracted extensor mechanism and to allow for increased range of motion. Postoperatively, the patient was permitted to bear weight as tolerated and the knee was immobilized in extension for two weeks. Thereafter, passive knee flexion was advanced incrementally. Active knee extension with activity as tolerated was permitted after six weeks. Two years after the total knee arthroplasty, the patient remained free of systemic and local infection and had a well-functioning prosthesis. The range of motion was 0° to 90° with no extensor lag. The Knee Society score was 93, which reflected a deduction of 7 points as a result of limited motion. The functional score was 90, which reflected unlimited walking tolerance without need of assistive devices and a deduction of 10 points for climbing or descending stairs with the assistance of a rail. Radiographs confirmed a well-fixed and well-positioned stemmed prosthesis and no evidence of recurrent tuberculosis (Fig. 5).
Proceed to Discussion >>Reference: Leclere LE, Sechriest VF II, Holley KG, Tsukayama DT. Tuberculous arthritis of the knee treated with two-stage total knee arthroplasty. A case report. J Bone Joint Surg Am. 2009;91:186-91.
Although cases of successful primary total knee arthroplasty for tuberculous arthritis have been reported by orthopaedists in China, Greece, Finland, Korea, Czechoslovakia, and the United Kingdom, the case of our patient represents the first such report from the United States of which we are aware. The majority of previously reported cases described the use of prolonged medical therapy for eradication of joint disease prior to arthroplasty. However, Kim described medical management combined with the use of limited surgical intervention prior to total knee arthroplasty in eight of nineteen knees, and Su et al. described the supplementation of medical therapy with arthroscopy prior to arthroplasty in twelve of sixteen knees. Additionally, it has been reported that knees that became infected with tuberculosis after total knee arthroplasty were successfully treated with resection arthroplasty and later reimplantation of a total knee prosthesis. While most reports describe the use of cruciate-substituting components, there are some reports of the use of hinged prostheses. In our patient, successful eradication of the infection required a combined and complementary medical and surgical approach. After the pulmonary infection was fully treated, a magnetic resonance imaging scan confirmed that anterior and posterior exposures would be needed to achieve a thorough debridement of the knee. After débridement had been accomplished, the cement spacer provided structural support to the limb and sustained local delivery of a high concentration of antibiotic to the bone and soft tissues. Postoperatively, the patient continued to receive a multidrug therapy as well as close clinical surveillance. Advanced imaging (magnetic resonance imaging) and diagnostic techniques (computed tomography-guided biopsy) were extremely helpful in making the decision to proceed with arthroplasty. The second-stage arthroplasty was technically challenging. Adequate exposure and mobilization of the extensor mechanism required an osteotomy of the tibial tubercle and a V-Y quadricepsplasty. To reestablish the joint line and set the component rotation, we referenced the femoral epicondylar axis. Finally, the severity of bone loss and collateral ligamentous insufficiency required an implant system with maximum flexibility in terms of augmentation, fixation, modularity, and constraint. This case also illustrates an important pitfall: how the presence of gout may delay the timely diagnosis of a septic joint. The presence of monosodium urate crystals in the synovial fluid of our patient confounded the initial clinical picture, delaying clinical recognition of tuberculous arthritis and resulting in treatment with intra-articular corticosteroids, which possibly accelerated the infection and joint destruction. Similar cases have been reported in which accelerated joint destruction resulted from intra-articular corticosteroid treatment of arthritis in patients with unrecognized tuberculosis. Lastly, this case experience as well as subsequent experimental work at our institution has confirmed that polymethylmethacrylate combined with even trace amounts of isoniazid (as little as 0.25 g) remains in a doughy state and therefore offers no structural support as a static spacer (unpublished data). Interestingly, aminoglycoside antibiotics have demonstrated therapeutic efficacy against many different strains of Mycobacterium tuberculosis in vitro. In the case of our patient, however, it is difficult to quantify the contribution of the local delivery of aminoglycosides from the cement spacer to sterilization of the joint. This case may not be representative of how all patients with chronic tuberculous arthritis of the knee will respond to such treatment. Optimal medical management and surgical management were required to achieve joint sterility prior to the performance of total knee arthroplasty. Perioperatively, a multidisciplinary approach was crucial to optimizing the outcome. Because individuals with a history of musculoskeletal tuberculosis will always remain at high risk for reactivation of local and/or systemic disease, a postoperative plan that includes medical as well as orthopaedic surveillance is most prudent following total knee arthroplasty.
Reference: Leclere LE, Sechriest VF II, Holley KG, Tsukayama DT. Tuberculous arthritis of the knee treated with two-stage total knee arthroplasty. A case report. J Bone Joint Surg Am. 2009;91:186-91.
Gouty arthritis of the knee
Tuberculosis of the knee
Osteoarthritis of the knee
Chronic low-grade bacterial infection of the knee


 Fig. 1
Fig. 1 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5
Fig. 5