A Sixty-five-Year Old Man with Progressive Hip Pain
December 2, 2015
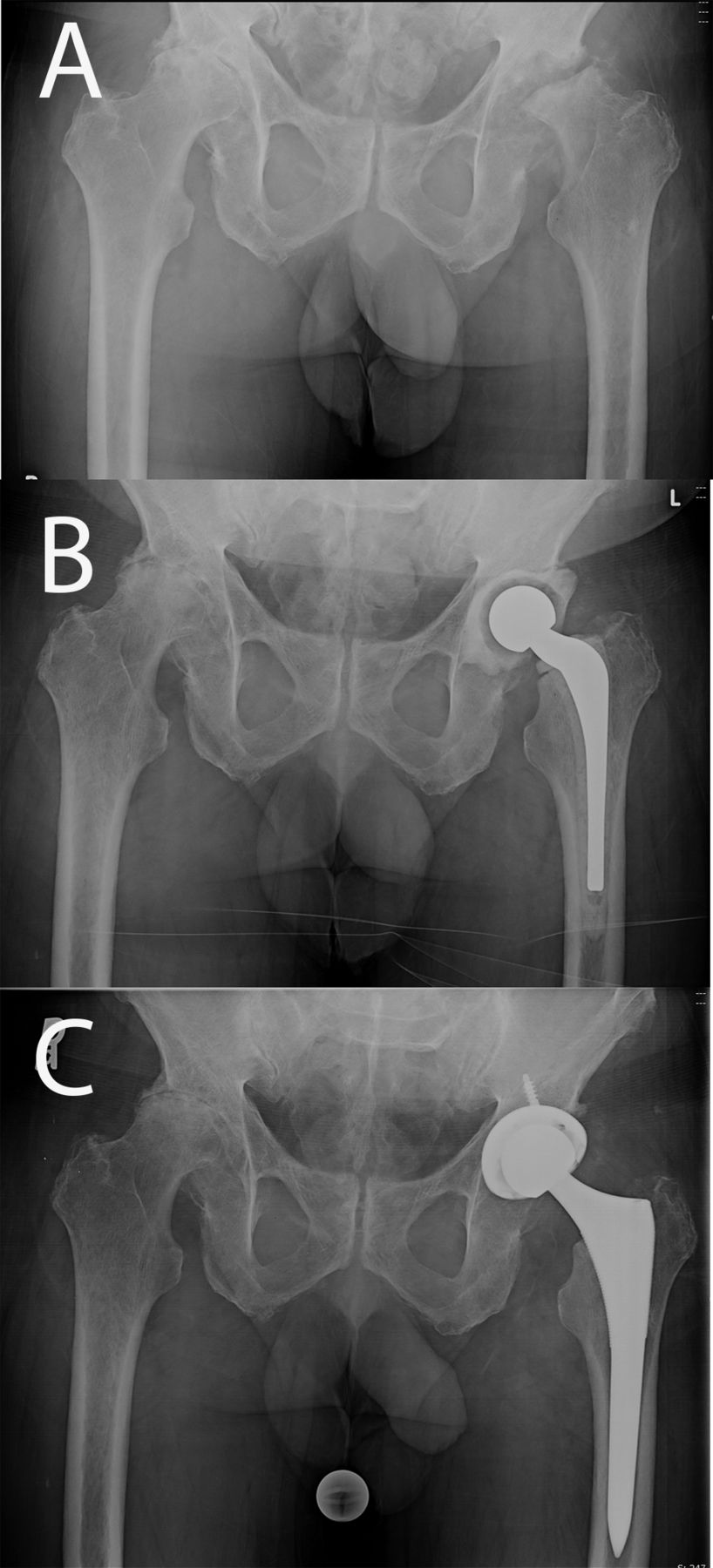
A sixty-five-year-old man presented to our clinic with a one-and-one-half-year history of progressive bilateral hip pain. The patient reported no prior trauma or surgical procedures involving the hips. He reported an increased intensity of pain in the left hip over the past eight months, which required him to walk with the aid of a cane. The medical and surgical history was remarkable for hypertension and thyroid disease. Physical examination revealed substantial pain with flexion and internal and external rotation of both hips. There was markedly more pain with movement of the left hip and the patient walked with an antalgic gait, favoring weight-bearing on the right side. A pelvic radiograph revealed bilateral hip osteonecrosis as well as arthrosis and destruction of the left femoral head (Fig. 1-A). Because of the destruction of the femoral head as noted on the radiographs, there was concern about possible infection. Therefore, in addition to routine preoperative laboratory tests, the C-reactive protein (CRP) level and erythrocyte sedimentation rate (ESR) were evaluated, both of which were unremarkable (CRP, 2.9 mg/L; ESR, 28 mm/hr). However, there was an increased index of suspicion for infection, so a hip aspiration was ordered. Because the patient lived a long distance from our institution, the hip aspiration was performed at an outside facility. The culture showed no growth, but, unfortunately, a cell count was not performed. A repeat hip aspiration was performed at our institution because of the high index of suspicion for infection and the lack of a cell count in the previous aspirate. This aspirate revealed 250 white blood cells/μL and 84% polymorphonuclear leukocytes, with no growth on culture after five days. On the basis of these findings, the patient was scheduled for a left total hip arthroplasty. Intraoperatively, there was substantial inflammatory tissue surrounding the left femoral head and acetabulum. The femoral head also appeared eburnated, and the cartilage was completely delaminated from the femoral head. Multiple frozen sections from the hip joint were sent to pathology, which revealed focal acute inflammation and >20 white blood cells per high-power field, consistent with an infection. Frozen sections from the femoral head revealed nonspecific acute and chronic inflammatory changes with >20 white blood cells per high-power field. Multiple culture specimens were obtained intraoperatively. Because of concern that the patient had an infection, a PROSTALAC (prosthesis of antibiotic-loaded acrylic cement) antibiotic spacer containing vancomycin and tobramycin was placed in the left hip (Fig. 1-B).
Postoperatively, the patient was empirically managed with intravenous vancomycin and oral levofloxacin after consultation with the infectious disease service at our institution. Two of the three tissue cultures were found to be positive for Propionibacterium acnes (P. acnes) on days 11 and 14, confirming the diagnosis of infection. Intravenous vancomycin was continued for a total of six weeks. Following completion of the course of intravenous antibiotics, reimplantation was delayed for seven months because the patient had other unrelated medical problems, including a colonic obstruction. Eight months following the placement of the antibiotic spacer, the spacer was removed and the patient underwent an uneventful total hip arthroplasty. At sixteen months, the patient reported excellent function with no pain in the hip (Fig. 1-C).
Proceed to Discussion >>Reference: Heckmann N, Sivasundaram L, Lieberman JR. Propionibacterium acnes infection in the native hip: A case report. JBJS Case Connect. 2015 Jul 08;5(3):e60.
P. acnes is a slow-growing, anaerobic, gram-positive bacillus that is part of the normal skin flora. While P. acnes is normally found as a contaminant in cultures from surgical specimens, cases of postoperative infection solely due to P. acnes have been reported in the cardiac, orthopaedic, and neurosurgical literature. Specific phylotypes of P. acnes have been found to be more prevalent in postoperative infections, suggesting that only specific variants of P. acnes are pathogenic. The pathogenesis of P. acnes may involve contamination of a surgical wound, hematogenous spread, or direct contiguous spread from a neighboring structure. The case presented here was likely the result of hematogenous or contiguous spread of the bacterium to the hip joint. It has long been known that P. acnes growth is most highly concentrated in moist environments such as the groin and axilla. As such, periprosthetic infections in the shoulder and hip have been reported extensively in the orthopaedic literature because of the high concentration of P. acnes growth in these regions. However, a mechanism for inoculation of the hip joint in the absence of surgery has not been elucidated. Deep inoculation from a superficial skin infection or an unreported traumatic event may be possible sources of infection in this case. The possibility of iatrogenic inoculation during the aspiration procedures cannot be ignored. However, the destruction of the femoral head on radiographs was observed prior to the aspirations. In addition, the worsening unilateral hip symptoms predate the first hip aspiration and the hip symptoms did not worsen substantially after either of the two aspiration procedures. Finally, P. acnes also has been reported as a cause of endocarditis, and hematogenous seeding from the heart is another possible cause of P. acnes infection in this case, although the patient had no known history of endocarditis. Because P. acnes is a common contaminant of surgical samples, there is debate as to what criteria are necessary to diagnose P. acnes as the primary cause of infection. For frozen-section analysis, Grosso et al. proposed that the perioperative finding of a total of ≥10 polymorphonuclear leukocytes in five high-power fields be used to suggest a P. acnes infection. Asseray et al. stated that growth on two or more cultures of deep samples, along with one of four other criteria (i.e., perioperative findings, local signs of infection, prior surgery, or an indwelling orthopaedic device), is sufficient for the definitive diagnosis of a P. acnes osteoarticular infection. In contrast, Do et al. suggested a more liberal set of criteria for diagnosing these types of infections, recommending one positive culture with P. acnes as well as clinical evidence of an infection as being sufficient for diagnosis. Our patient met both sets of criteria for P. acnes infection, with two positive deep-tissue cultures, >20 white blood cells per high-power field, and intraoperative inflammatory changes consistent with infection. Despite the growing body of diagnostic literature allowing clinicians to make a diagnosis of P. acnes infection intraoperatively, making this diagnosis preoperatively remains difficult. Clinical findings (e.g., point tenderness, decreased range of motion) are relatively nonspecific, particularly in patients with chronic symptomatic degenerative changes of the hip. In addition, radiographic findings may be of limited utility as patients with radiographic findings consistent with a traumatic etiology have been found to have P. acnes infections. Furthermore, cultures for P. acnes often require one to two weeks to achieve a positive result. Because of this delay, these infections are often missed on routine cultures as most institutions have standard incubation periods ranging from five to seven days. At most hospitals, the treating physician must communicate specific instructions to the microbiology laboratory to extend the incubation period. In addition, cultures often become positive long after a patient is discharged from the hospital, which can be problematic for patients with poor follow-up. Finally, the standard serum markers for infection (ESR, CRP, etc.) are often normal because of the low-virulence nature of the P. acnes bacterium. The treatment of P. acnes infection generally involves surgical debridement along with prolonged antibiotic therapy for four to six weeks. This duration takes into consideration the fact that the biofilm produced by P. acnes provides resistance against the systemically administered antibiotic. In our case, the patient received six weeks of intravenous antibiotics prior to definitive total hip arthroplasty and did not show any signs of recurrent infection at the one-year follow-up. However, the indolent nature of P. acnes growth results in a delay in recurrent infection by as much as two to four years. While P. acnes osteomyelitis has previously been reported as a post-implant complication in the arthroplasty literature, this case demonstrates that subacute P. acnes osteomyelitis can occur in the native hip of an immunocompetent adult. In patients with a high index of suspicion for infection, particularly in the setting of normal or equivocal infectious laboratory values, we recommend extending the culture incubation period for at least twenty-one days in order to avoid missing a P. acnes infection. A high index of suspicion is needed when assessing these patients as these infections are frequently missed.
Reference: Heckmann N, Sivasundaram L, Lieberman JR. Propionibacterium acnes infection in the native hip: A case report. JBJS Case Connect. 2015 Jul 08;5(3):e60.
Osteonecrosis related to hip infection of Staphylococcus epidermidis
Non-rheumatoid inflammatory arthriti
Osteonecrosis
Osteonecrosis related to hip infection of Propionibacterium acnes
Charcot arthropathy

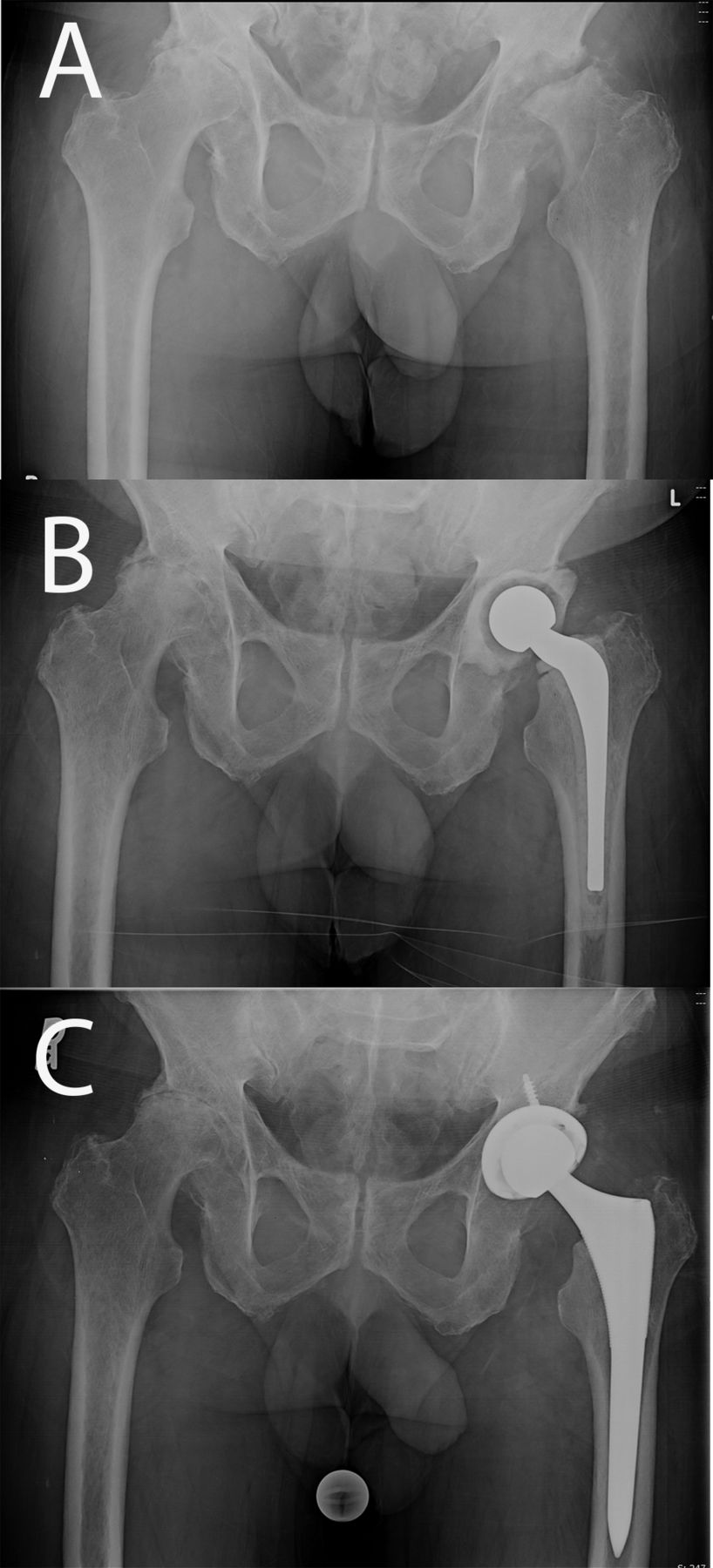
 Fig. 1
Fig. 1 Fig. 1
Fig. 1