A Twenty-nine-Year-Old Woman with a Twisting Injury to the Right Knee
November 18, 2015
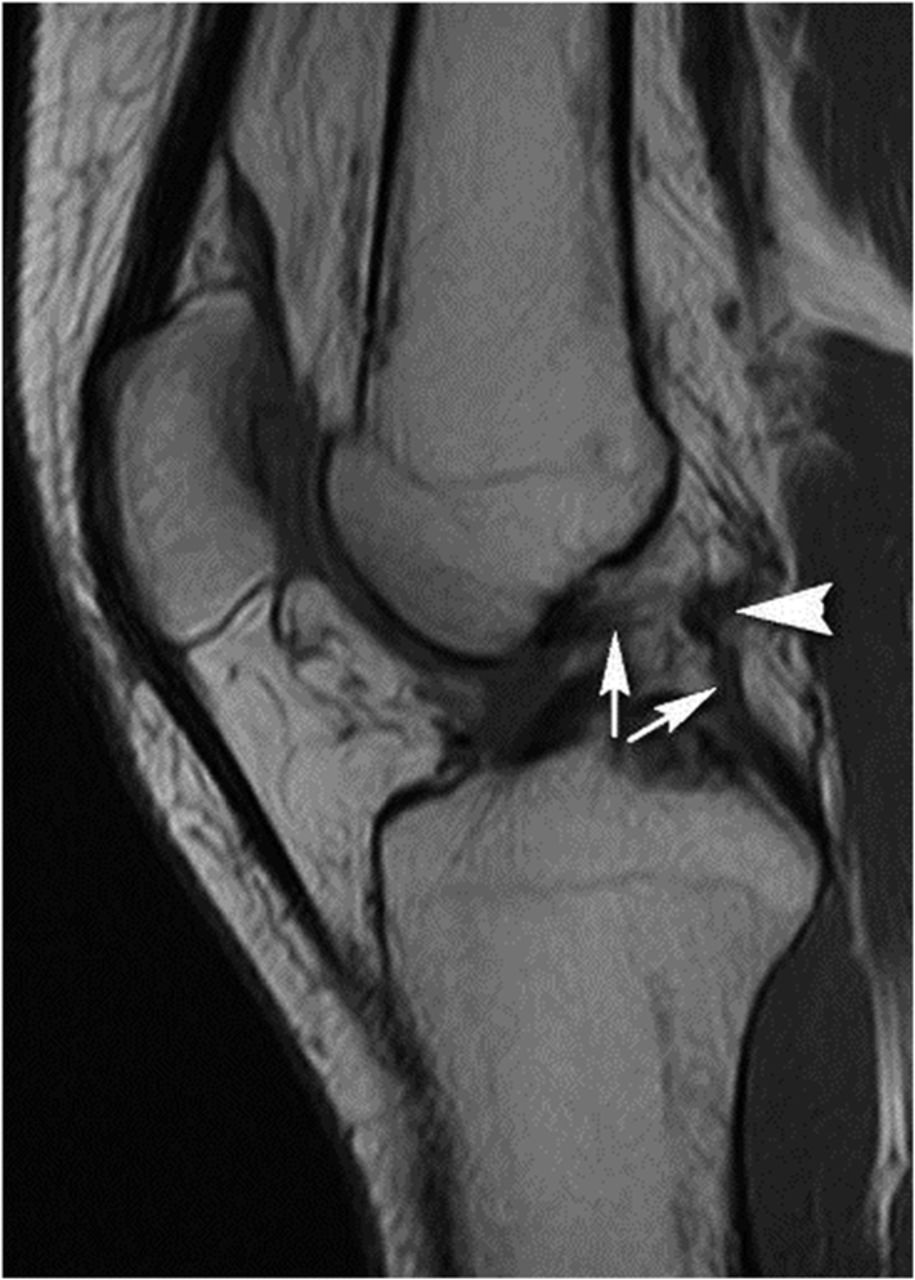
A twenty-nine-year-old female professional athlete, who had played handball from the age of twelve years and had competed in the premier league from the age of sixteen years, sustained a twisting injury to the right knee while landing. Seven days later, examination revealed a minimal right knee effusion and a positive Lachman test with a soft end point. The posterior drawer sign had a hard stop, and the posterior sag sign was negative. No lateral or medial instability was observed. Active and passive knee motion was intact. The patient denied any family history of skeletal congenital abnormalities; no abnormalities had been noted during pregnancy, childbirth, or childhood. Five years prior to this event, she had given birth to a healthy girl who had normal physical and mental development. Magnetic resonance imaging (MRI) of the right knee (Figs. 1-A, 1-B, and 1-C) demonstrated a recent ACL tear with a fully disorganized and partially retracted ligament as well as associated intra/periligamentous edema.
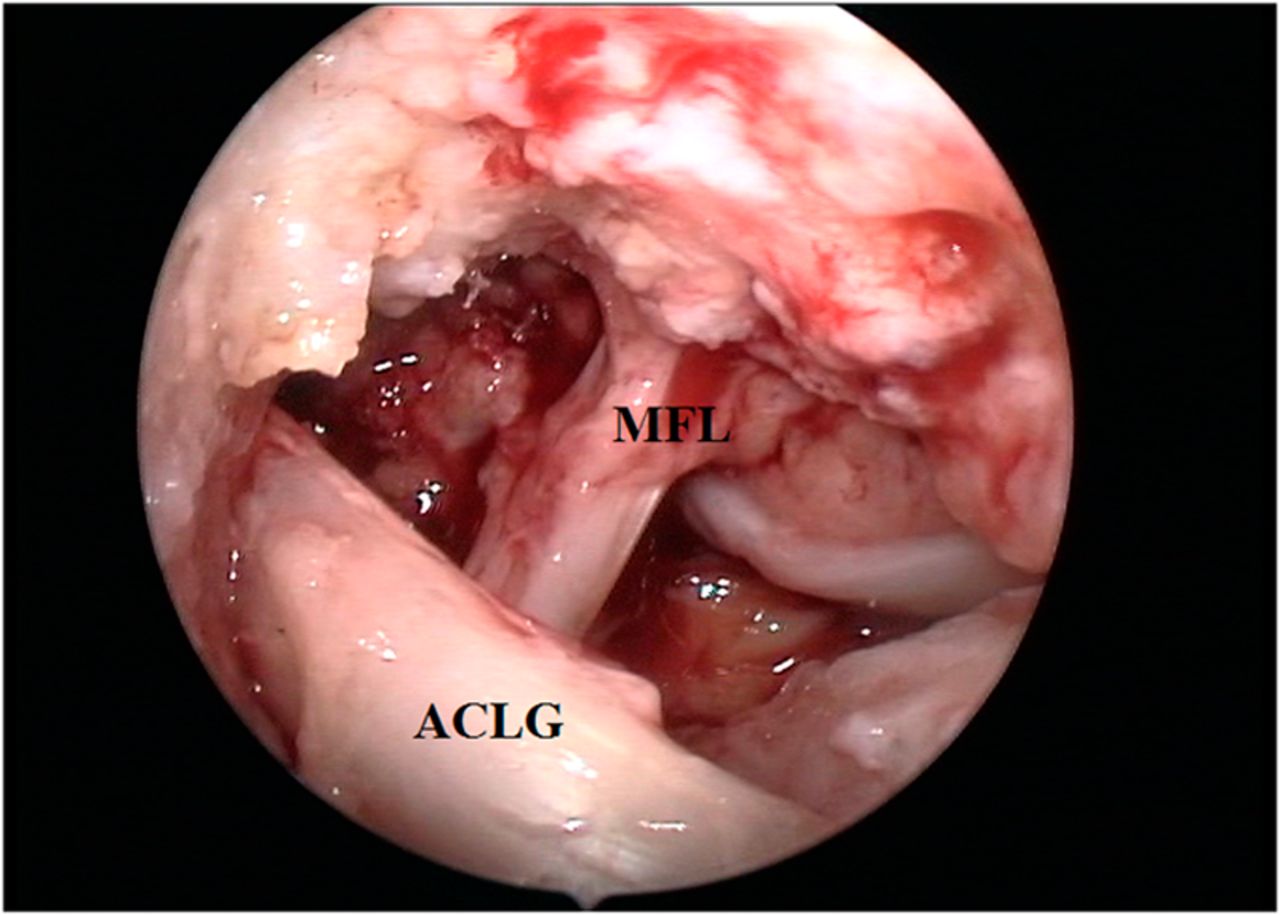
The imaging on the injured knee confirmed that the posterior cruciate ligament (PCL) did not have a normal appearance; there was only a thin, hypointense bandlike structure, consistent with a rudimentary, extremely hypoplastic ligament. There were no visible signs of an old PCL tear, such as ligament discontinuity or retraction, bands with abnormal orientation, or insertional surface irregularity. The presence of a well-developed hyperplastic posterior meniscofemoral ligament of Wrisberg (with a thickness of up to 5 mm) was noted. “Kissing” osteochondral contusions were present in the lateral compartment, on the weight-bearing surface of the femoral condyle, and on the posterior tibial plateau margin. Grade-II chondromalacia of the patellofemoral joint and an osteochondral lesion on the medial trochlear ridge, with a partial chondral defect and focal irregularity of the subchondral bone, were also present. Because of unusual MRI findings in the right knee, an MRI of the left knee was also obtained (Figs. 2-A, 2-B, and 2-C). The imaging on the uninjured knee revealed a hypoplastic PCL with a well-developed relatively hyperplastic ligament of Wrisberg. The ACL was intact and normal. There was an 11-mm intraosseous ganglion cyst in the tibial insertion of the posterior root of the medial meniscus, grade-II/III patellar chondromalacia predominantly on the medial facet, and an old osteochondral lesion on the medial trochlear ridge, with a partial-thickness chondral defect. The patient initially underwent physical therapy for four weeks. Once the knee effusion subsided, arthroscopic ACL reconstruction with a single-bundle bone-tendon-bone technique was performed. Prior to surgery, there was an 8-mm difference in the Lachman test (with a soft end point) between the right knee and the uninjured left knee. The pivot shift test on the right was positive (grade I with glide pivot). The posterior drawer sign was symmetrical with a hard stop on both knees. The surgery was performed under general anesthesia with the use of a tourniquet. The bone-tendon-bone graft was harvested and prepared. A standard anterolateral portal was used for viewing, and an anteromedial portal was used as a working portal. The ACL stump was debrided; instead of a normal PCL, there was a hyperplastic posterior meniscofemoral ligament of Wrisberg (Fig. 3). Tugging on the ligament of Wrisberg with a hook induced movement at the posterior horn of the lateral meniscus. The knee was placed in flexion between 110° and 120°. The femoral guide was introduced into the joint through the anteromedial portal, and a drill wire was placed into the center of the anatomic ACL insertion at the 10 o’clock position and was overdrilled with a 10-mm-diameter reamer. A suture was then retrieved, and a guide pin was drilled into the joint, followed by a cannulated reamer with an equal diameter to the graft in order to create the tibial tunnel. A grasper was placed through the tibial tunnel to retrieve the suture. The graft was passed through the tibia into the femoral socket, and once properly positioned in the tunnel, it was fixed with round cannulated interference screws. Firm traction was applied to the tibial bone block and the graft was fixed into the tibial tunnel with round cannulated interference screws (Fig. 4). Knee stability was checked with the Lachman and anterior drawer tests. Two drains were placed, and the operative wound was closed in the usual fashion. Postoperative radiographs showed that there were no signs of hypoplastic tibial eminences; the correct position of the interference screws was also evident (Figs. 5-A and 5-B). Six months later, the patient had a stable knee with a full range of motion, and both the Lachman and pivot shift tests were negative. She had continued playing handball professionally. Two years after the surgery, the patient had full range of motion in the operated knee and good strength in the quadriceps femoris muscle. There was a 2-mm difference in the Lachman test (with a firm end point) between the operated and healthy knee. The pivot shift test on the right was negative. The patient had continued playing professional handball without any limitations.
Proceed to Discussion >>Reference: Milankov MZ, Rasovic P, Miljkovic N. Bilateral congenital posterior cruciate ligament hypoplasia: A case report. JBJS Case Connect, 2013 Jan 09;3(1):e3.
Aplasia or hypoplasia of the PCL, the underdevelopment or incomplete development of the posterior PCL without other congenital anomalies, is an extremely rare congenital condition. To the best of our knowledge, only two cases have been reported in the literature: a unilateral aplasia in a twenty-eight-year-old man and bilateral hypoplasia in a forty-two-year-old woman. Both of these patients had experienced symptoms of pain while running, and the diagnosis had been established with MRI. Our patient had sustained an ACL rupture, and a hypoplastic PCL was also detected by MRI. The PCL is stronger than the ACL and is a primary restraint to tibial posterior draw, contributing approximately 90% to the resistance across most of the arc of knee flexion. Because of the strength of the PCL, isolated PCL rupture often does not lead to disabling instability. Shelbourne et al. analyzed patients with isolated PCL injuries who were not treated surgically: half of them returned to the same sport at the same or higher level, one-third returned to the same sport but at a lower level, and one-sixth switched sports because of this injury. In patients with an isolated PCL lesion, most of the arthritic changes were found in the medial tibiofemoral and patellofemoral compartments, as seen in our patient. During the ACL reconstruction in our case, after the ACL stump was debrided, we were able to clearly differentiate the ligament of Wrisberg, as shown on MRI. By tugging on the hyperplastic ligament of Wrisberg with a hook, we were able to induce movement at the posterior horn of the lateral meniscus. In a case of congenital absence of the cruciate ligaments, Berruto et al. found a ligamentous structure similar to the PCL that was hypoplastic and thin, as well as a rudimentary meniscofemoral ligament. The ligament of Wrisberg extends between the medial side wall of the femoral intercondylar notch and the posterior horn of the lateral meniscus, and presents as a substantial and relatively large structure in some knees. The meniscofemoral ligaments have been treated as unimportant vestigial structures in the past. However, now that their function in helping to control posterior laxity has been demonstrated, some authors have proposed that meniscofemoral ligaments may act as a “third” cruciate ligament or as secondary restraints to posterior tibial translation in the PCL-injured knee. After the meniscofemoral ligaments had been cut, there was a substantial increase in laxity in both the intact and PCL-deficient knees. Because they have a mean strength of approximately 300 N, mechanically they are equivalent to the posteromedial bundle of the PCL. Conversely, the ligament of Wrisberg is tight in the extended knee and slackens with knee flexion because its femoral attachment moves down toward the tibial plateau as the knee flexes. Isolated congenital aplasia or hypoplasia of the PCL is clinically and biomechanically similar to an isolated PCL lesion; because of the rarity of this condition, the therapeutic approach is not standardized. Da Gama Malchér et al. proposed a conservative treatment, while Lee et al. proposed PCL reconstruction. Our patient was a professional athlete who had no problems prior to the ACL injury, likely because of the hyperplastic meniscofemoral ligament of Wrisberg that provided sufficient stability. As a result, ACL reconstruction alone was adequate treatment.
Reference: Milankov MZ, Rasovic P, Miljkovic N. Bilateral congenital posterior cruciate ligament hypoplasia: A case report. JBJS Case Connect, 2013 Jan 09;3(1):e3.
Synovial chondromatosis
Pigmented villonodular synovitis
Hypoplastic posterior cruciate ligament (PCL), hyperplastic ligament of Wrisberg
Intra-articular lipoma
Rupture of the PCL bilaterally and the anterior cruciate ligament (ACL) on the injured knee

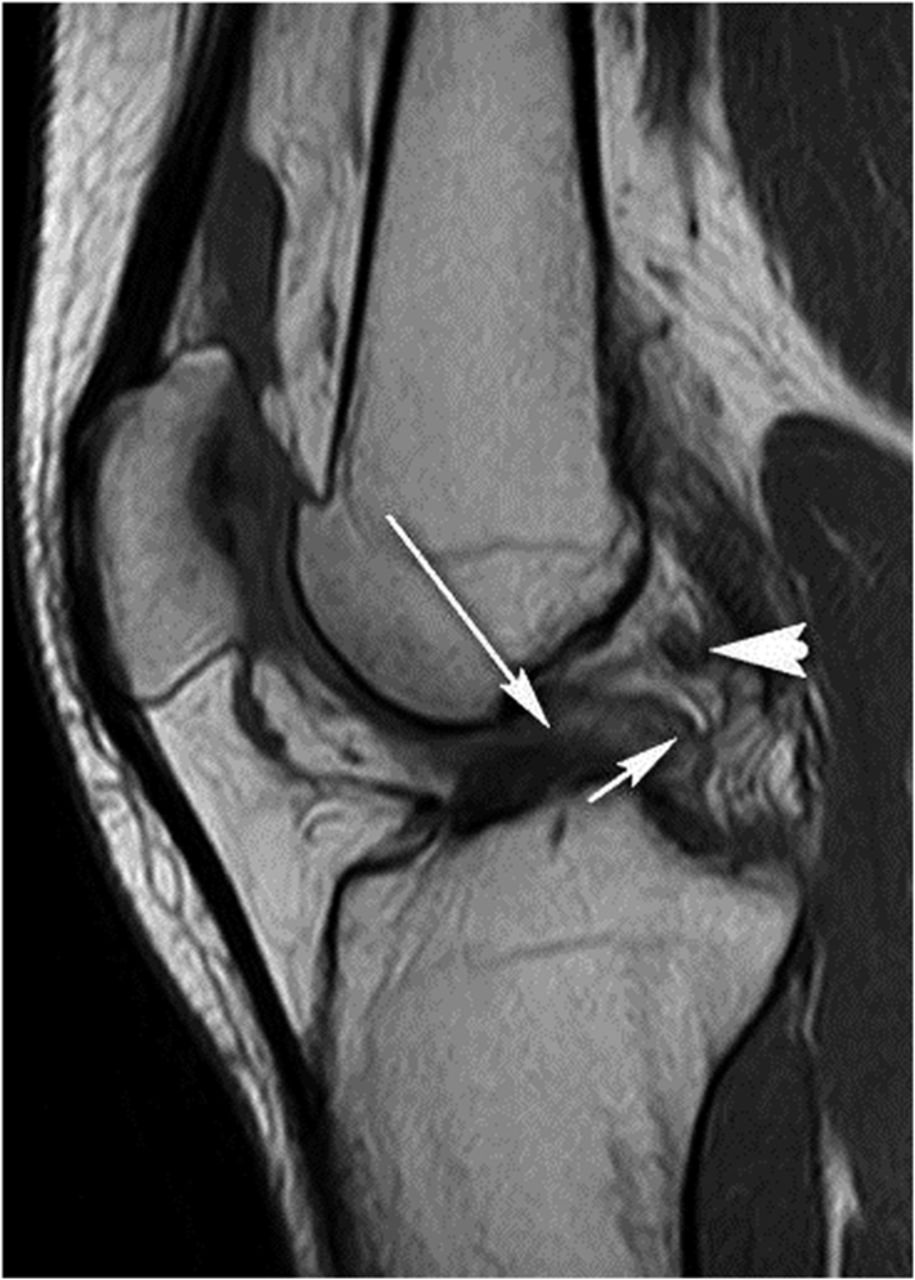
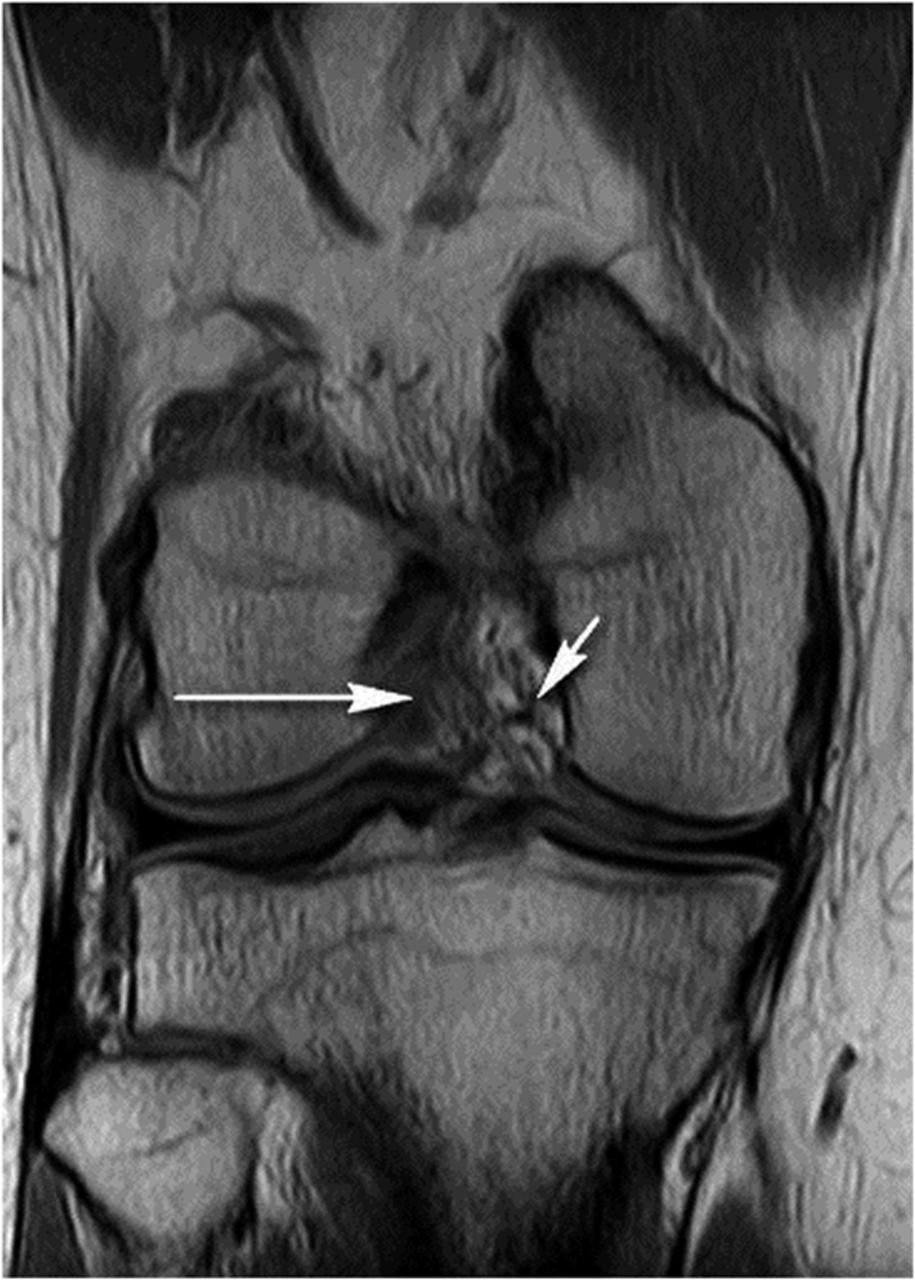

 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 1-C
Fig. 1-C Fig. 2-A
Fig. 2-A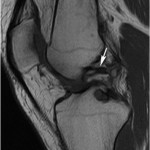 Fig. 2-B
Fig. 2-B Fig. 2-C
Fig. 2-C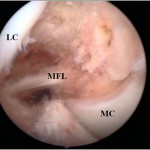 Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5-A
Fig. 5-A Fig. 5-B
Fig. 5-B