A sixty-two-year-old woman with no prior neck problems was referred to our institution for evaluation because of a two-week history of neck pain with progressive tetraparesis. She reported the onset of severe neck pain radiating into the shoulders. There had been no antecedent trauma. Two days prior to admission, she had had increasing numbness in both hands with decreased grip strength and increasing leg weakness. She reported no incontinence. She had had a weight loss of 10 to 15 lb (4.5 to 6.8 kg) over several months and had felt generally unwell. The patient’s medical history included long-standing medication-resistant hypertension and mild chronic renal failure with a creatinine level of 200 mol/L. She also had a history of congestive heart failure, and fourteen years before the onset of the severe neck pain, she had had a cerebrovascular accident on the left side, with a minimal residual deficit consisting of a right facial droop. She reported episodes of gout in the past and ongoing problems with constipation and arthralgias. Physical examination revealed posterior tenderness in the midcervical region. Neurologically, the patient required support for walking because of poor balance and weakness. The upper-extremity strength was 4 of 5 in all muscle groups, according to the classification system of the American Spinal Injury Association. The motor power of the right lower extremity was 3 of 5 in all muscle groups with the exception of the extensor hallucis longus, which was graded 4 of 5. The left lower extremity was normal with the exception of the hip flexors, which were graded 3 of 5. Sensation to light touch and pinprick was normal, but proprioception was abnormal. Reflexes were brisk, with bilateral upgoing toes and a positive Hoffmann sign in the upper extremities. Radiographs of the cervical spine revealed diffuse osteopenia. There was a 25% anterior spondylolisthesis of the third on the fourth cervical vertebra and a 50% anterior spondylolisthesis of the fourth on the fifth cervical vertebra (Fig. 1). The disc heights at the third and fourth and the fourth and fifth cervical levels were severely reduced. The facet joints at these vertebral levels were not well visualized. Magnetic resonance imaging showed a reduction in the anterior-posterior diameter of the spinal canal to 8 mm at the fourth and fifth cervical levels (Fig. 2). T2 sequencing showed spinal cord compression at the fourth and fifth cervical levels and mild hyperintensity consistent with cord edema. The lateral masses of the fourth cervical vertebra were not well defined. The patient was admitted to the hospital, where she was managed with steroids and placed in tong traction. Within forty-eight hours, the spondylolisthesis of the third on the fourth cervical vertebra was reduced anatomically and that of the fourth on the fifth cervical vertebra was corrected to 20%. There was a gradual decrease in the neurologic symptoms. The working diagnosis was cervical instability secondary to an osseous destructive process resulting in myelopathy. The differential diagnosis included tumor (probably a metastasis), infection, an inflammatory process, and degenerative and metabolic bone disease. Diagnostic investigations were initiated. Relatively urgent operative intervention was indicated for complete reduction and decompression, stabilization, and tissue biopsy. The patient was then taken to the operating room for an indirect decompression through reduction and for combined anterior and posterior stabilization (Fig. 3). The first stage of this combined procedure included anterior discectomies at the third and fourth and the fourth and fifth cervical levels, reduction, autogenous bone-grafting, and plate application. Grossly, the bone graft appeared to be of poor quality. The second stage, performed during the same operation and through a posterior approach, revealed that most of the right fourth cervical lateral mass was eroded. Tissue was obtained for biopsy. Less extensive erosive changes were noted on the left lateral mass. There was disruption of the intraspinous and supraspinous ligaments at the fourth and fifth cervical levels. Lateral-mass plates and screws and autogenous bone graft were applied from the third to the fifth cervical level. On the basis of the preoperative images and the neurologic improvement that was obtained with closed reduction, it was thought that the patient did not require direct decompression. Postoperatively, the patient wore a cervical orthosis and was able to walk short distances. The neurologic deficits decreased, but she continued to feel unwell and lethargic. The biopsy demonstrated nonspecific reactive changes within cancellous bone. There was no histologic evidence of infection or neoplasm. Additional bone from the iliac-crest bone-graft donor site was also submitted for histologic examination, which demonstrated excessive numbers of osteoclasts, numerous resorption sites, and prominent paratrabecular osteoblastic activity with adjacent fibrosis (Fig. 4). A chest radiograph showed multiple rib fractures and erosions of the lateral ends of the clavicles and the medial aspect of the proximal part of the humeral shaft. A whole-body technetium-99m bone scan demonstrated increased uptake throughout the entire skeleton, suggestive of metabolic bone disease. Radiographs of the hands revealed generalized osteopenia with coarsening of the trabecular pattern and subperiosteal resorption. Osteolysis was present in the distal phalanges, and there were a number of small erosions involving the wrist and the metacarpophalangeal and interphalangeal joints in an asymmetric pattern. A clavicular radiograph revealed distal resorption of both clavicles with widening of the acromioclavicular joints (Fig. 5). A pelvic radiograph showed osteosclerosis of the bones of the lumbar spine and pelvis with widening of the symphysis pubis and resultant formation of a pseudarthrosis. Laboratory tests showed that the level of ionized serum calcium was 1.42 mmol/L (normal range, 1.12 to 1.30 mmol/L) and the level of phosphate was 0.50 mmol/L (normal range, 0.80 to 1.45 mmol/L).
The level of parathyroid hormone was elevated at 127 pmol/L (normal range, 1.3 to 5.4 pmol/L). These findings were consistent with primary hyperparathyroidism. The findings on a technetium-sestamibi parathyroid and pertechnetate thyroid scan were consistent with the diagnosis of parathyroid hyperplasia. Several weeks after the index operative procedure, four enlarged parathyroid glands were surgically removed. A partial parathyroid gland was reimplanted into the left sternocleidomastoid. The histologic features were consistent with generalized parathyroid hyperplasia. Postoperatively, the patient had markedly improved energy and function. The patient required an intensive course of inpatient rehabilitation. At the one-year follow-up evaluation, she was living at home. She had improved energy, decreased arthralgias, no neck pain, and mild residual numbness in the left hand without any other objective neurologic deficit. Radiographs showed the fusion to be solid.
Proceed to Discussion >>Reference: Underwood HA, Fisher C, Dvorak M, O’Connell J. Primary hyperparathyroidism: an unusual cause of cervical myelopathy. A case report. J Bone Joint Surg Am. 2001 May;83(5):744-7.
To our knowledge, this is the first reported case of primary hyperparathyroidism leading to cervical myelopathy. Although there was no evidence of osteitis fibrosa, osteitis fibrosa cystica, or brown tumor in the completely eroded lateral mass of the fourth cervical vertebra, generalized bone loss was present. The erosion of the lateral masses caused instability at the third and fourth and the fourth and fifth cervical levels and accounted for the resultant subluxation. Primary hyperparathyroidism results in increased osteoclastic activity and, therefore, in decreased bone stock. Functionally, the lateral masses at the fourth cervical level did not have enough strength to support the structures cephalad and caudad to them. Surgical intervention was required for indirect neurologic decompression and stabilization. The decision to perform a combined anterior and posterior procedure was based on the poor bone quality, the excessive instability, and the necessity for reduction at the fourth and fifth cervical levels to enhance indirect decompression of the spinal cord. Although relief of spinal nerve-root pain and cord compression has been reported after parathyroidectomy alone, the severity of the cervical instability and the deformity in our patient required operative reduction and stabilization. Regression of osseous changes has been reported after parathyroidectomy. The removal of the enlarged parathyroid glands in our patient dramatically decreased the systemic symptoms and probably facilitated fusion of the involved cervical segments. In summary, hyperparathyroidism can cause instability of the cervical spine leading to myelopathy. Management requires decompression and stabilization of the cervical spine, followed by treatment of the cause of the hyperparathyroidism. Patients who present with a severe form of destructive spondyloarthropathy may have a generalized metabolic bone disease as the underlying etiology. In the current case, the laboratory and radiographic findings as well as the findings on histologic examination of bone distant from the affected site assisted us in arriving at the correct diagnosis.
Reference: Underwood HA, Fisher C, Dvorak M, O’Connell J. Primary hyperparathyroidism: an unusual cause of cervical myelopathy. A case report. J Bone Joint Surg Am. 2001 May;83(5):744-7.
Primary hyperparathyroidism
Secondary hyperparathyroidism
Hypocalciuric hypercalcemia
Chronic renal insufficiency
Hypercalcemia of malignancy



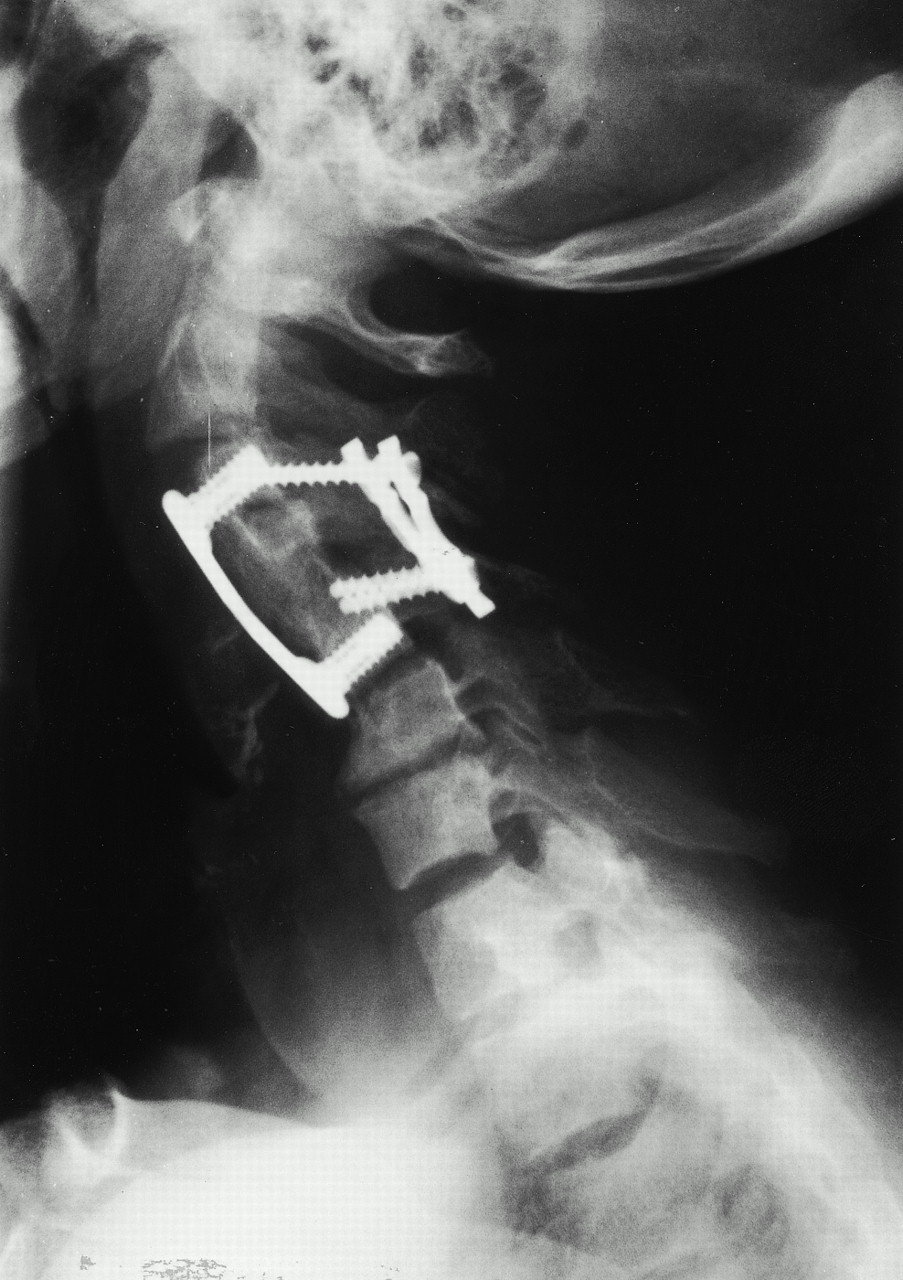
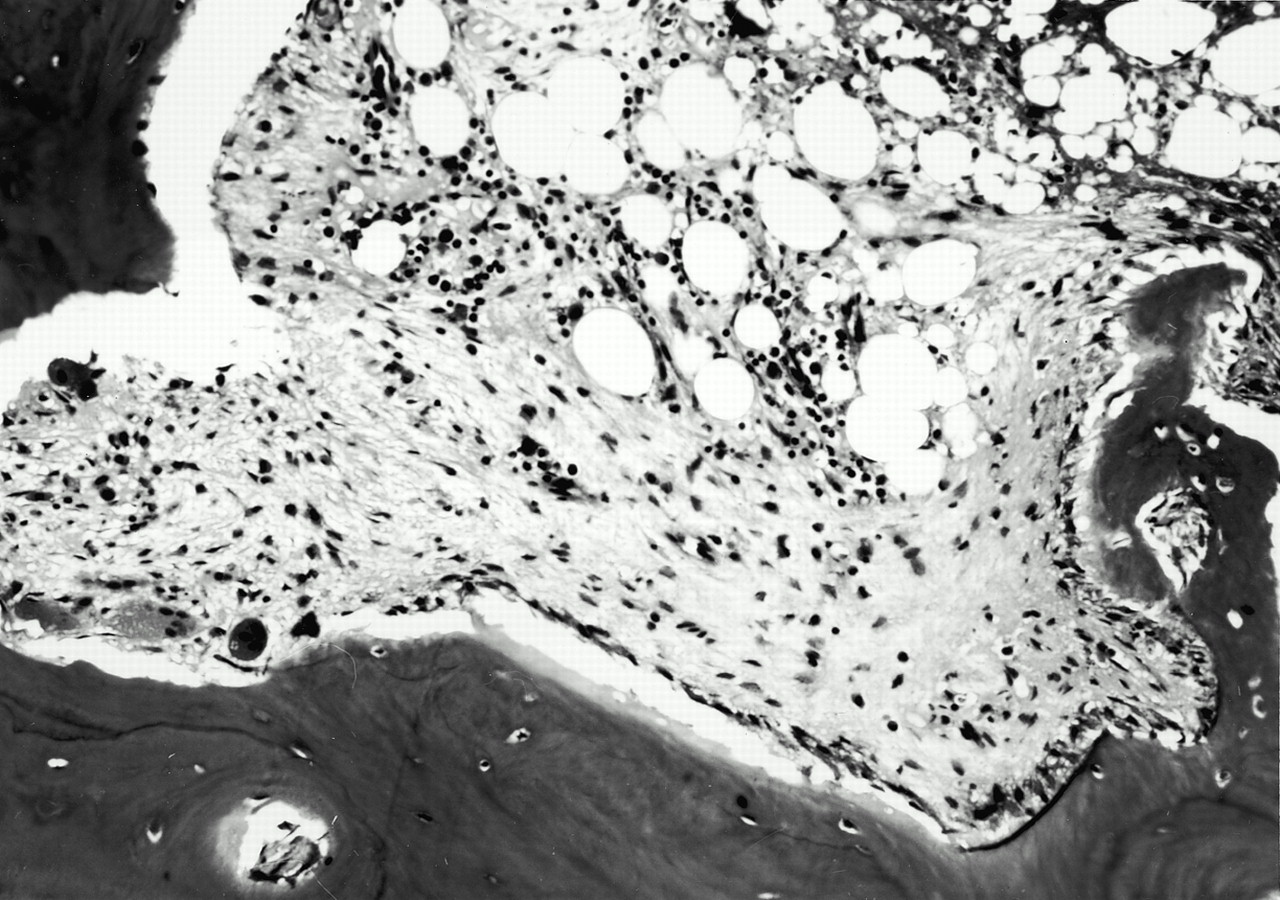

 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5
Fig. 5