A 52-Year-Old Man with Discomfort Following Total Knee Arthroplasty
October 4, 2017
A fifty-two-year-old man with no relevant medical history underwent an uneventful right-sided total knee arthroplasty for symptomatic osteoarthritis. The preoperative (Fig. 1-A) and immediately postoperative radiographs (Fig. 1-B) did not reveal any osseous lesion, and the tibia and femur both appeared to be normal during surgery. Six weeks later, he returned to the clinic prepared to undergo the same operation on the left side, which was subsequently successfully undertaken.
Five months following the right-sided total knee arthroplasty, the patient reported discomfort in the upper medial aspect of the tibia. On examination, he had a good range of knee motion, and he was systemically well. Blood tests showed no signs of infection, and given his activity of cycling thirty-five miles and walking two and one-half miles daily, a clinical diagnosis of pes anserine bursitis was made. Nevertheless, radiographs were obtained (Fig. 1-C).
One month later, the patient returned to the clinic, and although the tibial tenderness had improved, the radiographs had revealed osseous resorption with cortical destruction of the proximal part of the medial aspect of the tibia (Fig. 1-C). As reported by a musculoskeletal radiologist, the magnetic resonance imaging (MRI) most likely showed a periprosthetic infection (Figs. 2-A and 2-B).
A small open biopsy was performed in the operating room under fluoroscopic guidance, and a specimen from the medial aspect of the tibia was sent for microbiological and histological analysis. Cultures revealed growth of coagulase-negative Staphylococcus epidermidis. Histologic findings demonstrated hemorrhagic granulation with a scattered population of mixed inflammatory cells, including polymorphonuclear leukocytes, which indicated a low-grade infection. Results of laboratory tests revealed a C-reactive protein level of 17 mg/L (normal range, <6 mg/L), an erythrocyte sedimentation rate of 28 mm/h (normal range, 1 to 35 mm/h), and a white blood-cell count within normal limits.
After discussion with orthopaedic colleagues and because of a likely infective process, we decided to perform a two-stage revision arthroplasty. The first stage took place six months after the primary joint replacement. Intraoperatively, the medial part of the tibial plateau macroscopically appeared to be replaced by a loculated, firm, organized hematoma that was densely attached to the surrounding soft tissue (Fig. 3). This was all removed and sent for histological analysis, and an antibiotic cement spacer was placed in situ. The patient was started on parenteral antibiotics, followed by oral antibiotics. Microscopic evaluation of the intraoperative specimens revealed no neutrophils. Microbiological cultures of the specimens revealed no growth of organisms.
Histologic analysis showed an expanded synovium with a hemorrhagic appearance that showed a proliferation of small capillaries, the features of which were initially described as representing an organizing hematoma (Fig. 4). Evidence of an acute inflammatory process was not seen. The diagnosis from the local histopathology department was unclear, so the specimen was sent to the national bone tumor unit, which provided a diagnosis after the second-stage revision had taken place.
The consultant pathology report indicated epithelioid hemangioma.
The second stage of the joint revision took place six weeks after the first stage. The last follow-up was eighteen weeks postrevision surgery, by which time the conclusive report from the national bone tumor unit had been received. At this time, the C-reactive protein level and the erythrocyte sedimentation rate both had returned to the normal range. The patient had cycled eleven miles to the clinic, was symptom-free and constitutionally well, and had a good range of movement in both knees.
Proceed to Discussion >>Reference: Viswanath A, Nolan JF. Periprosthetic epithelioid hemangioma of the proximal part of the tibia: a case report. JBJS Case Connect. 2012 Oct-Dec;2(4):e70.
This is a case of an epithelioid hemangioma of bone that appeared within a few months of total knee replacement. To our knowledge, there are no other reports documenting a potential association between arthroplasty and the development of an epithelioid hemangioma.
Epithelioid hemangioma, previously known as angiolymphoid hyperplasia with eosinophilia or histiocytoid hemangioma, has recently been accepted into the World Health Organization Classification of Bone Tumors, placed toward the benign end of the spectrum between hemangioma (benign) and angiosarcoma (malignant). It is one of a group of vascular lesions characterized by large epithelioid endothelial cells that have abundant eosinophilic cytoplasm. There have been relatively few reported cases of epithelioid hemangioma of bone, although some believe this may be because of its previous erroneous classification as a low-grade hemangioendothelial sarcoma. Epithelioid hemangioma, however, is recognized as a distinct entity. It is usually a solitary lesion that is eccentrically placed when occurring in long bones and well-circumscribed with expanded bone, but it is rarely aggressive. To date, there have been no reports of recurrence. It most commonly affects long bones; however, when it affects small tubular bones, it can be associated with cortical destruction and local soft-tissue invasion. Macroscopically, the tumor is described as multiloculated, reddish-brown, and hemorrhagic in appearance.
In many previously reported cases, patients with epithelioid hemangioma presented with localized pain of some duration (often months). In our patient, however, the symptoms were acute. The lesion was discovered prior to implant failure because radiographs were obtained, despite a presumptive clinical diagnosis of pes anserine bursitis. Given that the initial culture report and blood tests were suggestive of infection, the correct management was undertaken. Management was aggressive and appropriate for a potentially infected joint replacement. If the histology from the initial biopsy had pointed toward a benign vascular lesion rather than infection, a single-stage revision might have been undertaken.
Associations with concurrent skin lesions and with pregnancy have been made, but the etiology for this tumor is yet to be found. In skin and soft tissues, epithelioid hemangioma has been described as inflammatory and potentially reactive rather than neoplastic. In our patient, the tibia looked grossly normal during the primary joint replacement operation; therefore, no tissue removed at this stage was sent to the pathology department. All of the changes were noted five months postoperatively when the patient experienced pain.
This case highlights the need for a thorough investigation of pain that occurs following a joint replacement. Once an osteolytic lesion is demonstrated on radiographs, most common pathologies may be investigated and excluded; however, if pain is not investigated because it is transient, a benign but locally aggressive tumor, such as an epithelioid hemangioma, may lead to implant failure.
Reference: Viswanath A, Nolan JF. Periprosthetic epithelioid hemangioma of the proximal part of the tibia: a case report. JBJS Case Connect. 2012 Oct-Dec;2(4):e70.
What is the diagnosis?
Epithelioid hemangioma
Bacillary angiomatosis
Fungal infection with yeast, consistent with Cryptococcus
Metastatic adenocarcinoma
Adverse local tissue reaction from polyethylene debris


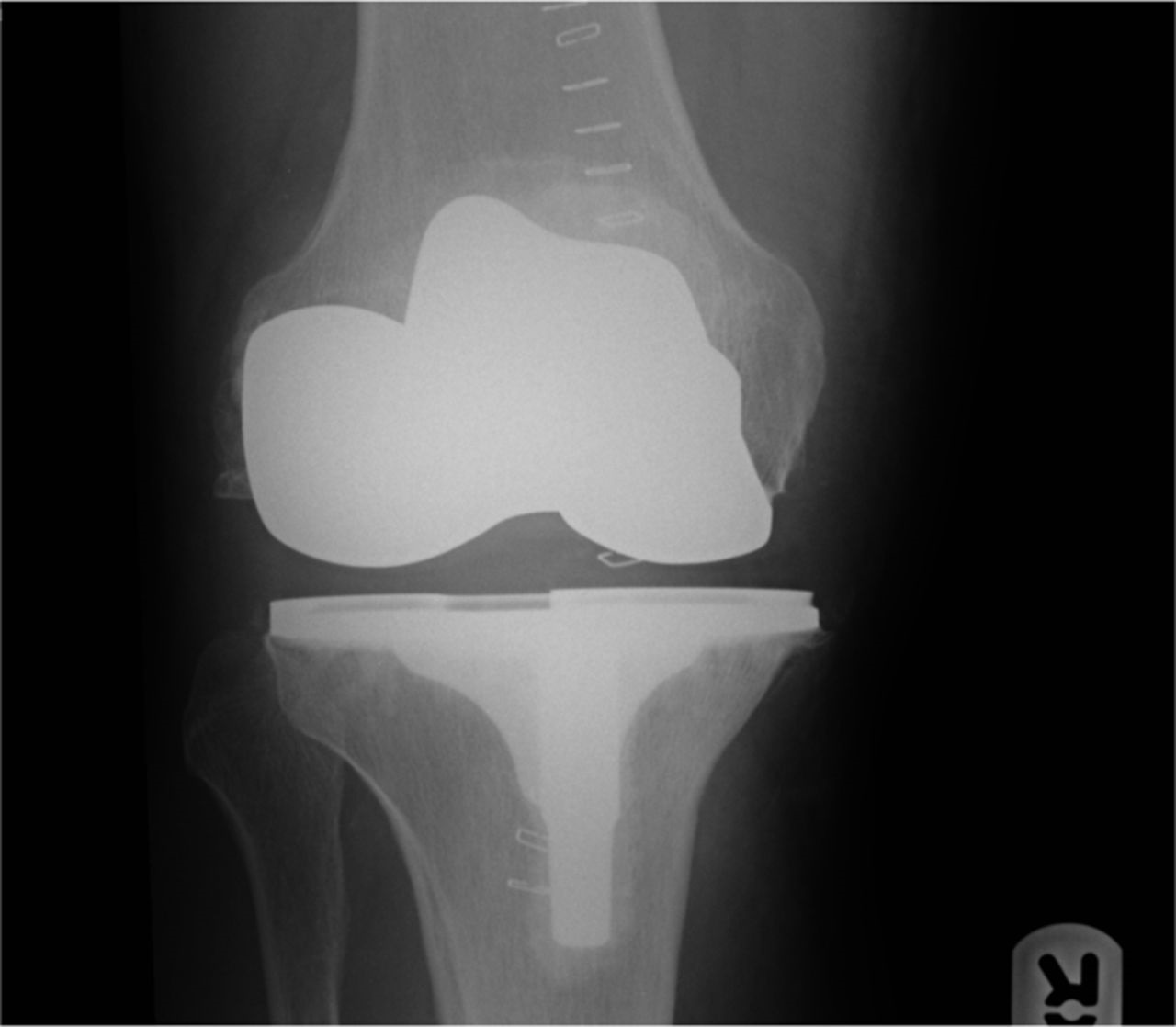

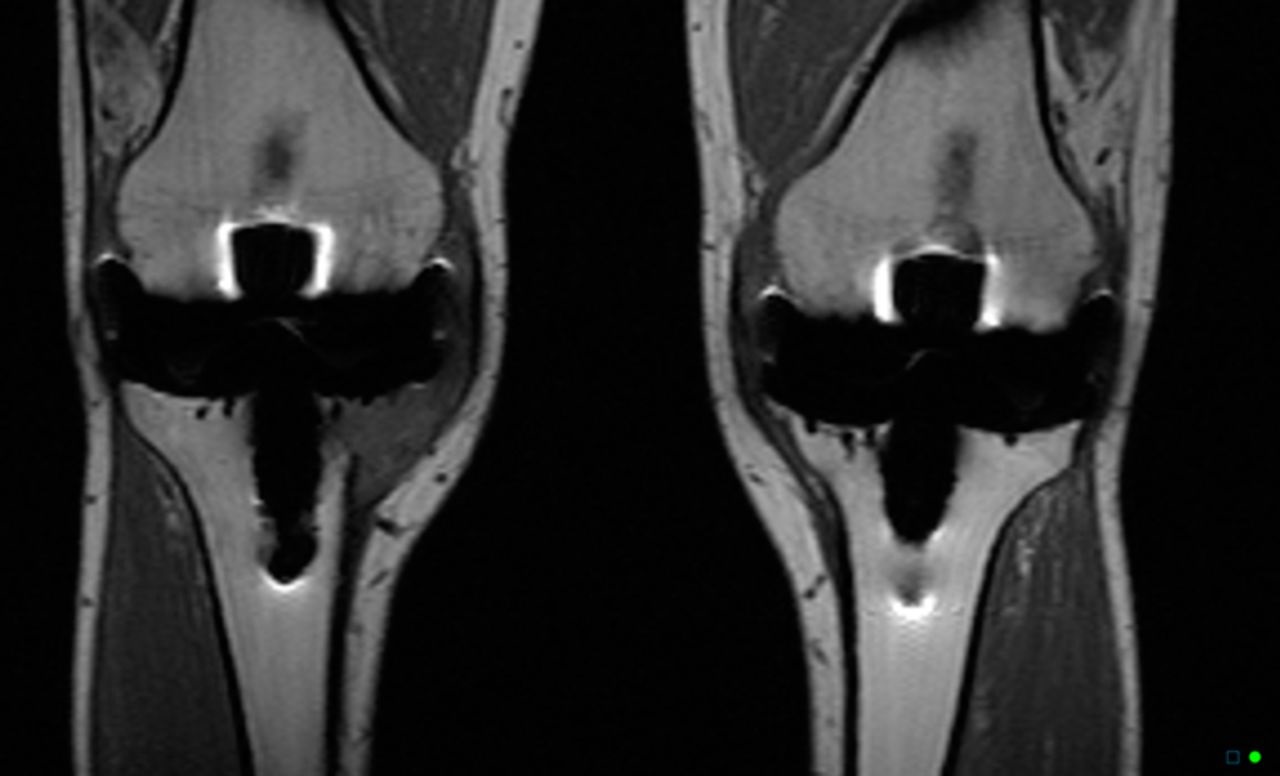
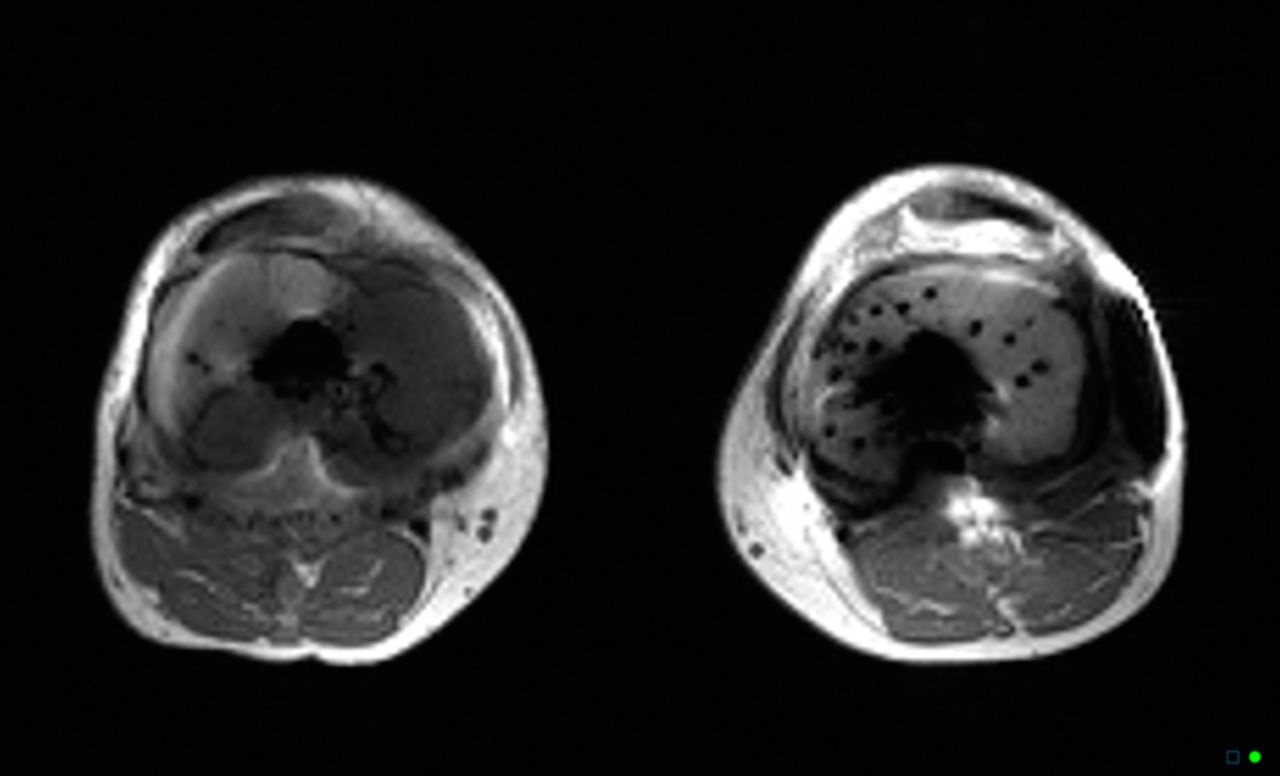

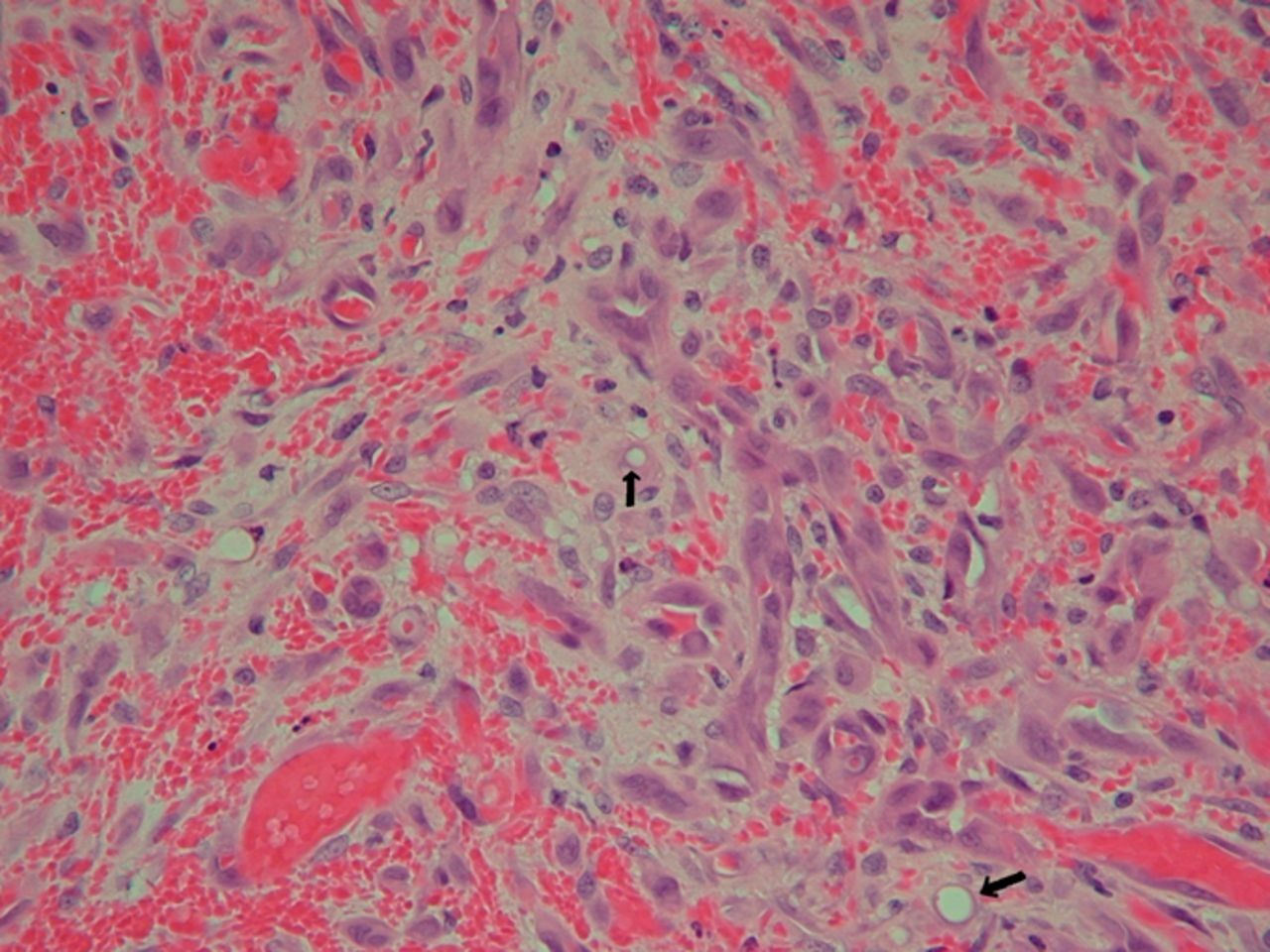
 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 1-C
Fig. 1-C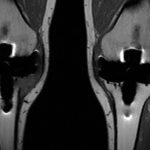 Fig. 2-A
Fig. 2-A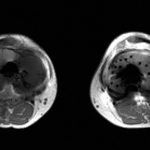 Fig. 2-B
Fig. 2-B Fig. 3
Fig. 3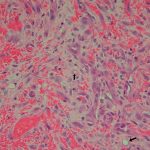 Fig. 4
Fig. 4