A 69-Year-Old Woman with a Swollen Arm Following a Fall
October 7, 2020
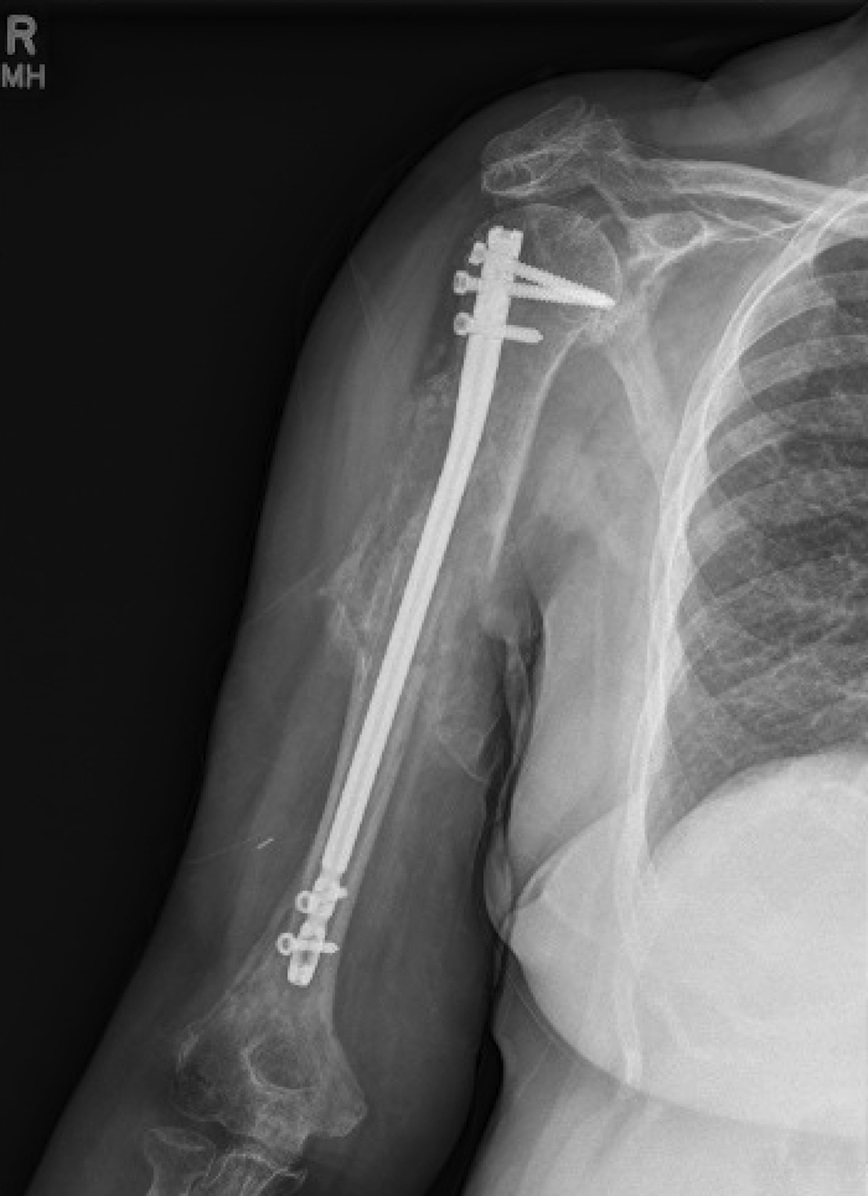
A 69-year-old, right-hand-dominant woman presented 7 days after sustaining a closed right proximal humeral shaft fracture after a fall from height. Her medical history included myasthenia gravis and right rotator cuff arthropathy. She was a nonsmoker and a community ambulator requiring the use of a walker. She had no previous injuries, no relevant surgical history, and no previous neurological deficits of the right upper extremity. On presentation, she was neurovascularly intact with extensive swelling and ecchymoses of the arm. Radiographs demonstrated substantial displacement of the fracture (Figs. 1-A and 1-B).
The fixation of the fracture was performed 12 days after the injury. Before surgery, the patient was neurovascularly intact but had mild weakness with flexion at the right thumb interphalangeal joint along with persistent swelling of the arm. A standard starting point for intramedullary fixation of the humerus was used. On opening the humeral canal, 100 mL of blood was released, suggestive of a fracture hematoma. The hematoma was completely evacuated, and there was no sign of active arterial bleed. Because the patient had limited mobility of the shoulder, a Shantz pin on the distal fragment and a blunt bone hook on the proximal fragment were used to reduce the fracture via a small lateral incision. A Stryker proximal humeral nail size 8 × 240 mm was used. Postoperatively, she had intact sensation and motor function of the axillary, median, radial, and ulnar nerves as well as a palpable radial pulse.
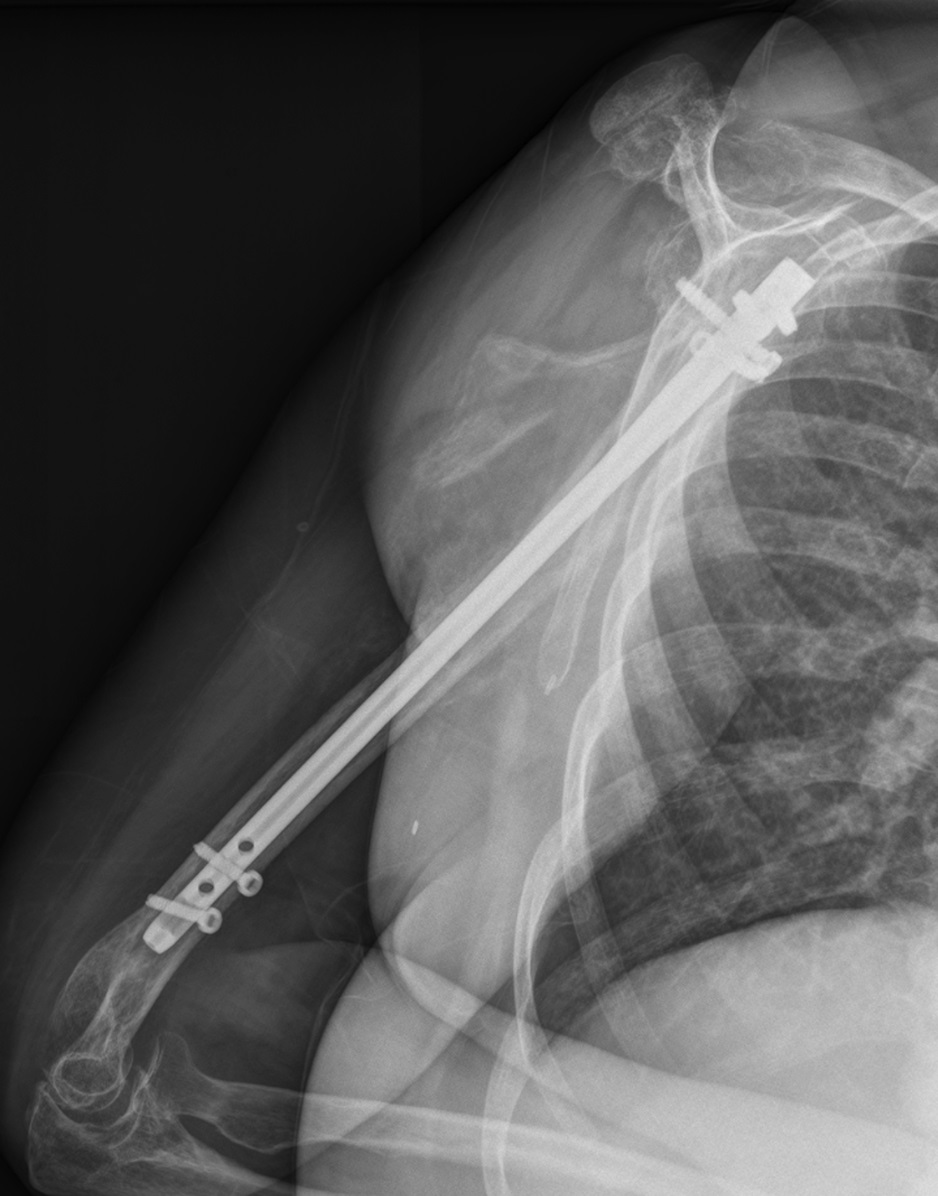
At her 6-week postoperative visit, the patient presented reporting progressive arm swelling, weakness, and loss of sensation in the right hand. Radiographs demonstrated interval healing of the previous fracture and appropriate position of the implant (Figs. 1-C and 1-D). She had a normal vascular examination but had no wrist flexion or extension and was 0/5 for her anterior interosseous and posterior interosseous nerve function. The only motor function that the patient retained was the ability to weakly flex the fourth and fifth digits, as well as active flexion and extension of the elbow. She had no sensation to light touch over the median, radial, and ulnar nerve distributions over the hand. Computed tomography (CT) without contrast of the right arm demonstrated a large compressive hematoma on the medial and posterior aspects of the right upper arm, which measured 71 × 94 mm (Fig. 2-A). CT angiogram was performed (Figs. 2-B through 2-D). Distally, the brachial, radial, and ulnar arteries were patent.
The CT angiogram demonstrated a pseudoaneurysm of the brachial artery.
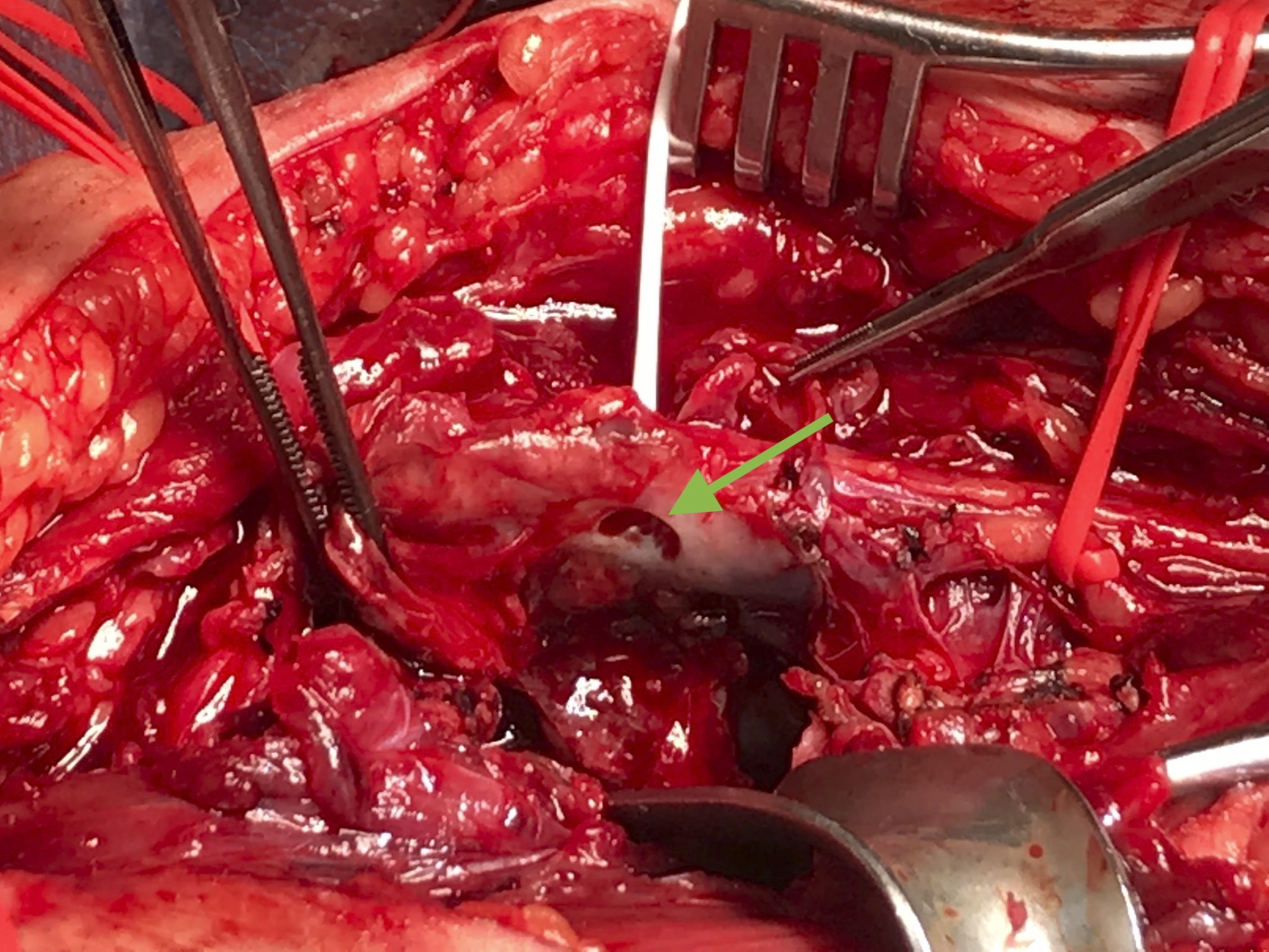
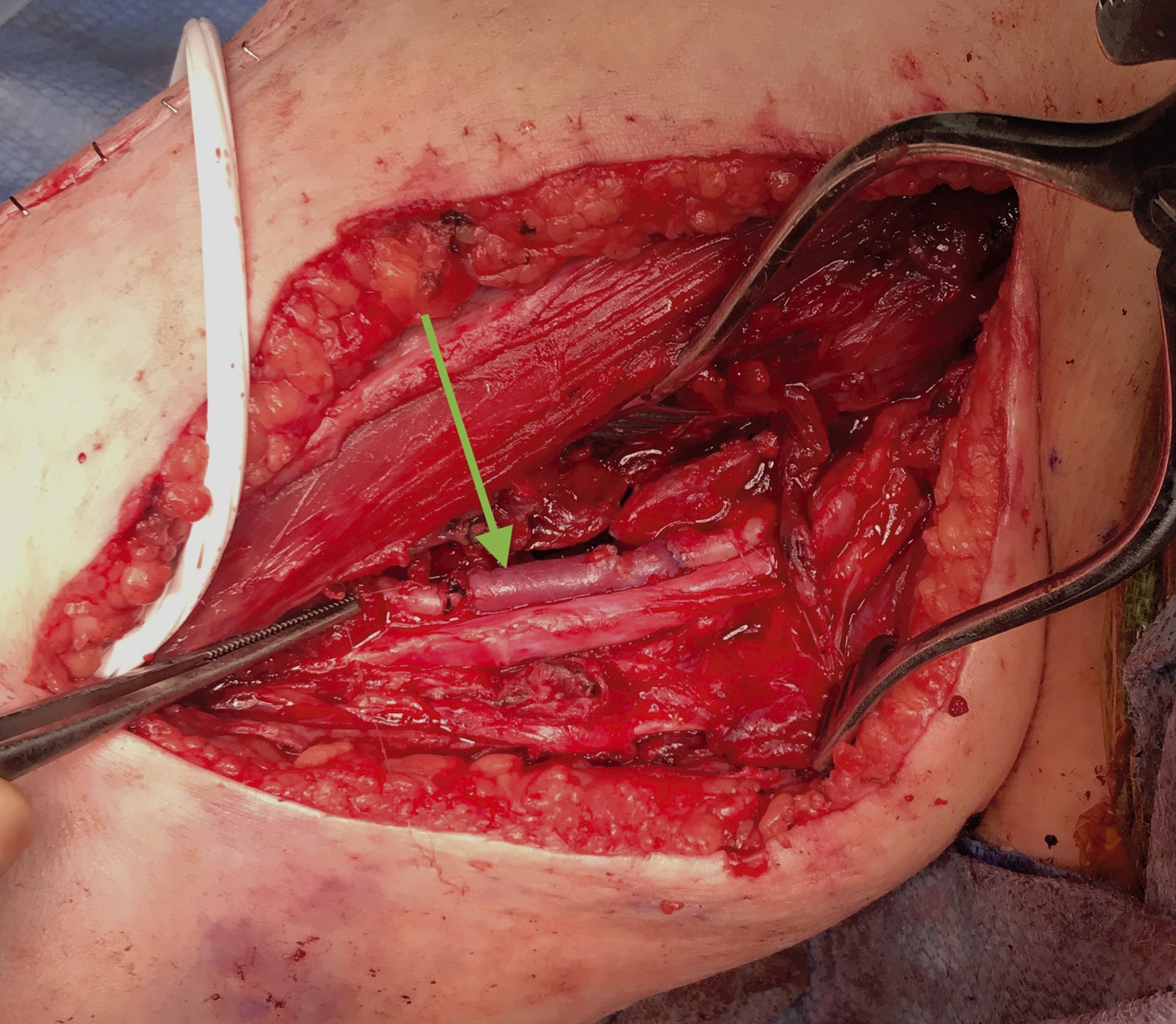
The patient was emergently taken to the operating room and a vascular surgical procedure was performed. Intraoperatively, the pseudoaneurysm extended deep into the lateral arm with visible compression of the median and ulnar nerves. The median, ulnar, and musculocutaneous nerves were intact with no gross injury. The radial nerve was not visualized but was palpated and intact. There was no evidence of muscle necrosis. Exploration of the brachial artery after proximal and distal control revealed the large puncture in the wall of the brachial artery, which was consistent with the location of the original medial spike of the humeral fracture (Fig. 3-A). The hematoma was decompressed, and a neurolysis of the median and ulnar nerves was performed. The pseudoaneurysm was resected, and the artery was bypassed with a reverse cephalic vein interposition graft (Fig. 3-B).
Immediately postoperatively, the patient’s neurovascular examination remained unchanged. At her 2-week postoperative visit, she was noted to have the return of sensation in the ulnar nerve distribution and continued to have flexion of the fourth and fifth digits. She was able to actively flex and extend the elbow. Her examination at her 2-month postoperative visit showed slightly increased strength in flexion of the fourth and fifth digits. Fracture alignment was noted to be unchanged with robust callous formation (Figs. 4-A and 4-B). She was improving and requested to return to work. An electromyography was ordered to evaluate her neurological function. Unfortunately, this could not be performed because the patient unexpectedly died 3 months after surgery due to unknown causes.
Proceed to Discussion >>Reference: Manzano G, Brown C, Harth K, Ochenjele G. Acute presentation of a pseudoaneurysm after a proximal humerus shaft fracture: a case report. JBJS Case Connect. 2020 Jan-Mar;10(1):e0131.
We present the first case of a symptomatic pseudoaneurysm in the acute period 8 weeks after a proximal humeral shaft fracture. This is in contrast to previous case reports in which patients presented with a pseudoaneurysm at an average of 8.5 months after their injury. Symptomatic pseudoaneurysms after trauma typically present over the course of months to years after injury. A pseudoaneurysm occurs when damage to the arterial wall causes a leakage of blood into the surrounding tissues with persistent communication between the originating artery and resultant cavity. Infection and trauma are common etiologies of pseudoaneurysms. Pseudoaneurysms due to trauma have been found to occur in less than 0.5% of patients and therefore may often be missed. Diagnosis may be difficult because brachial artery pseudoaneurysms less than 2 cm in diameter can be silent or asymptomatic during a long enlarging period. Symptoms are usually limited to the mass effect of the lesion, which include tenderness, pain, and swelling. Subsequent neurological and vascular deficits become apparent as the surrounding structures are impinged. In proximal humeral shaft fractures, neurovascular injury is rare and therefore further workup is critical in a patient presenting with this sequela. In our patient, neurologic compromise was present and intraoperatively the expanding hematoma associated with the pseudoaneurysm had a compressive mass effect on the nerves. However, her neurovascular presentation may also suggest the presence of mixed proximal nerve injuries instead of direct compression from the pseudoaneurysm. Previous reports also described associated neurological deficits due to the mass effect of the pseudoaneurysm. If not diagnosed promptly and managed correctly, pseudoaneurysms can cause serious threat to limb and life. Thrombotic sequelae can occur, leading to ischemia of the limb and possible amputation. In rare cases, rupture can occur and can be associated with high mortality. Arterial duplex evaluation with ultrasound may be sufficient for evaluation and diagnosis in a patient with suspected pseudoaneurysm. CT angiogram of the upper extremity can provide additional anatomic detail if duplex becomes challenging in the setting of such a large compressive hematoma and can aid in additional operative planning.
A high index of suspicion for the development of a pseudoaneurysm is critical in a patient with a substantially displaced proximal humeral shaft fracture, especially one with a sharp bony fragment. The combination of a medial spike on the distal fracture fragment, a very stiff shoulder, severe displacement of the shaft, and delayed presentation 7 days after injury was most likely responsible for injury to the brachial artery in our patient. This medial spike was also evident in previous reports of pseudoaneurysm after proximal humeral shaft fractures. Intraoperatively, the vascular surgery team did notice the area consistent with the initial bony puncture on the arterial wall at the level of the fracture (Fig. 3-A). This likely enlarged over time, and the hematoma caused distortion of over 50% of the luminal diameter of the brachial artery requiring complete replacement of the artery for reconstruction. The severe displacement of this fracture might also suggest that the initial displacement on injury was probably greater than what was represented on static radiographs, which would have increased the risk of brachial artery injury. Iatrogenic injury to the brachial artery after surgical fixation of humeral fractures has been previously reported after plating, but not intramedullary nailing. However, it was unlikely that injury to the brachial artery occurred during operative intervention because no pulsatile bleeding was encountered. The bleeding that we encountered with our opening reamer was suggestive of a fracture hematoma. In addition, meticulous reduction and nail insertion techniques were performed. Reaming was performed with fluoroscopic visualization and was not performed at the fracture site.
Multiple treatment options exist for symptomatic pseudoaneurysms. Endovascular techniques may be considered to address pseudoaneurysms, but an open approach is needed when neurovascular compromise is present and large hematomas require drainage. Most pseudoaneurysms of the upper extremity, especially of the brachial region, should be treated with repair and/or reconstruction as indicated to preserve arterial inflow to the extremity.
We recommend close follow-up and a thorough history and physical examination in the acute period after a severely displaced proximal humeral shaft fracture. A high index of suspicion should be adopted, and early imaging as a precaution, such as an arterial duplex, should be considered. Awareness of this life and limb-threatening complication is important for timely diagnosis and management.
Reference: Manzano G, Brown C, Harth K, Ochenjele G. Acute presentation of a pseudoaneurysm after a proximal humerus shaft fracture: a case report. JBJS Case Connect. 2020 Jan-Mar;10(1):e0131.
What is the diagnosis?
Laceration of the median nerve by fracture
Laceration of the radial nerve by fracture
Lipofibromatous hamartoma of the median nerve
Brachial artery pseudoaneurysm
Inflammatory pseudotumor



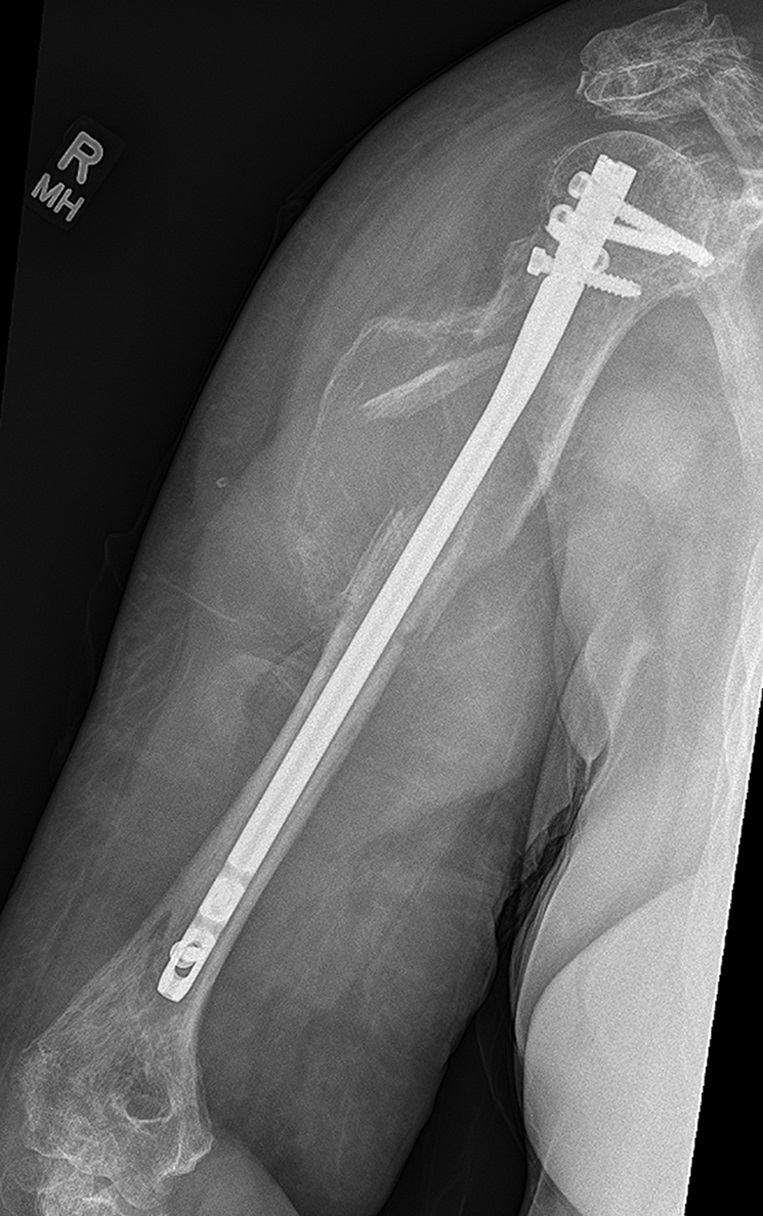
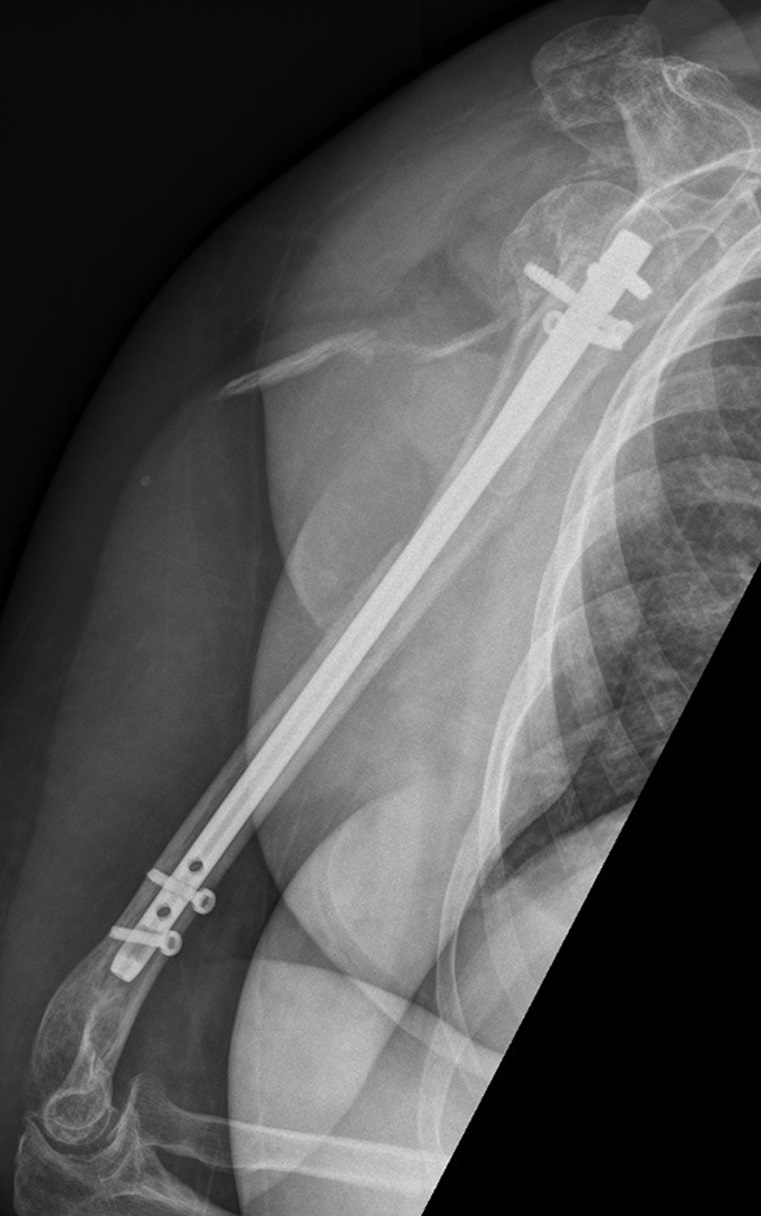
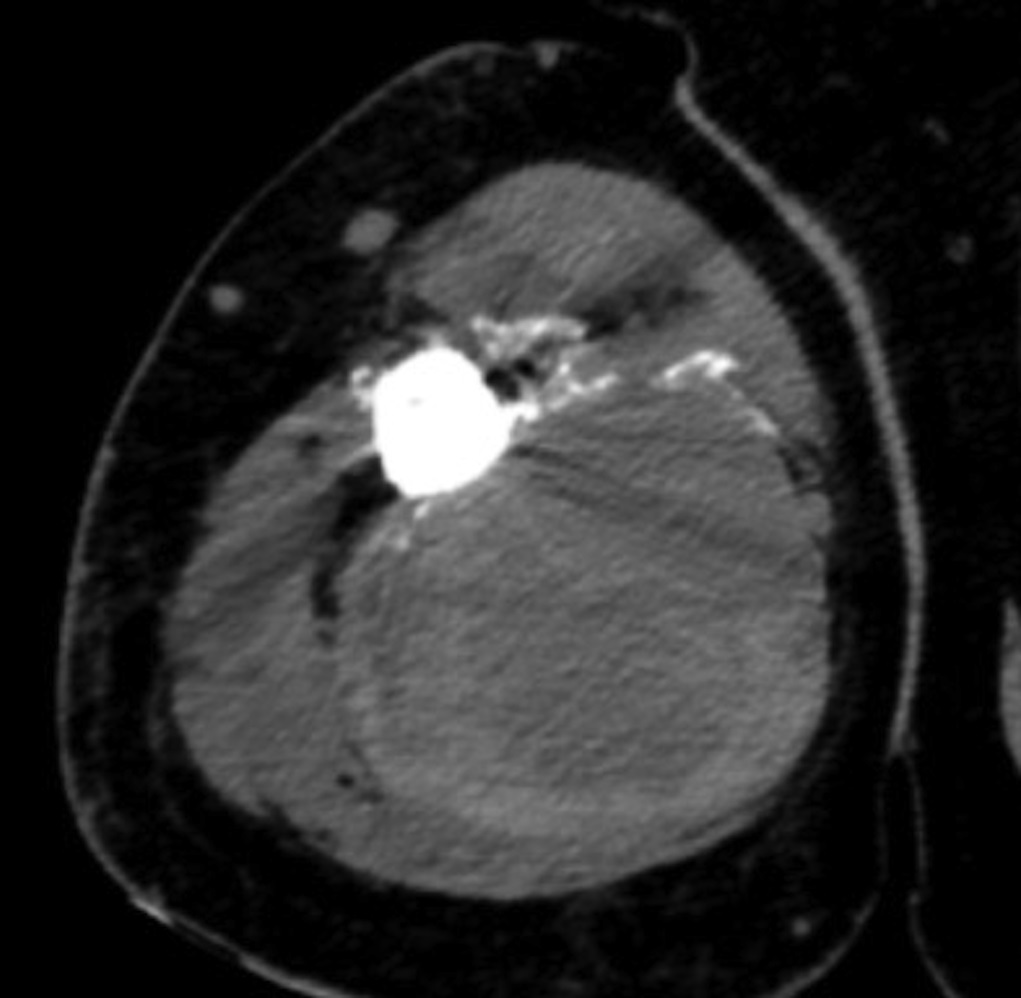

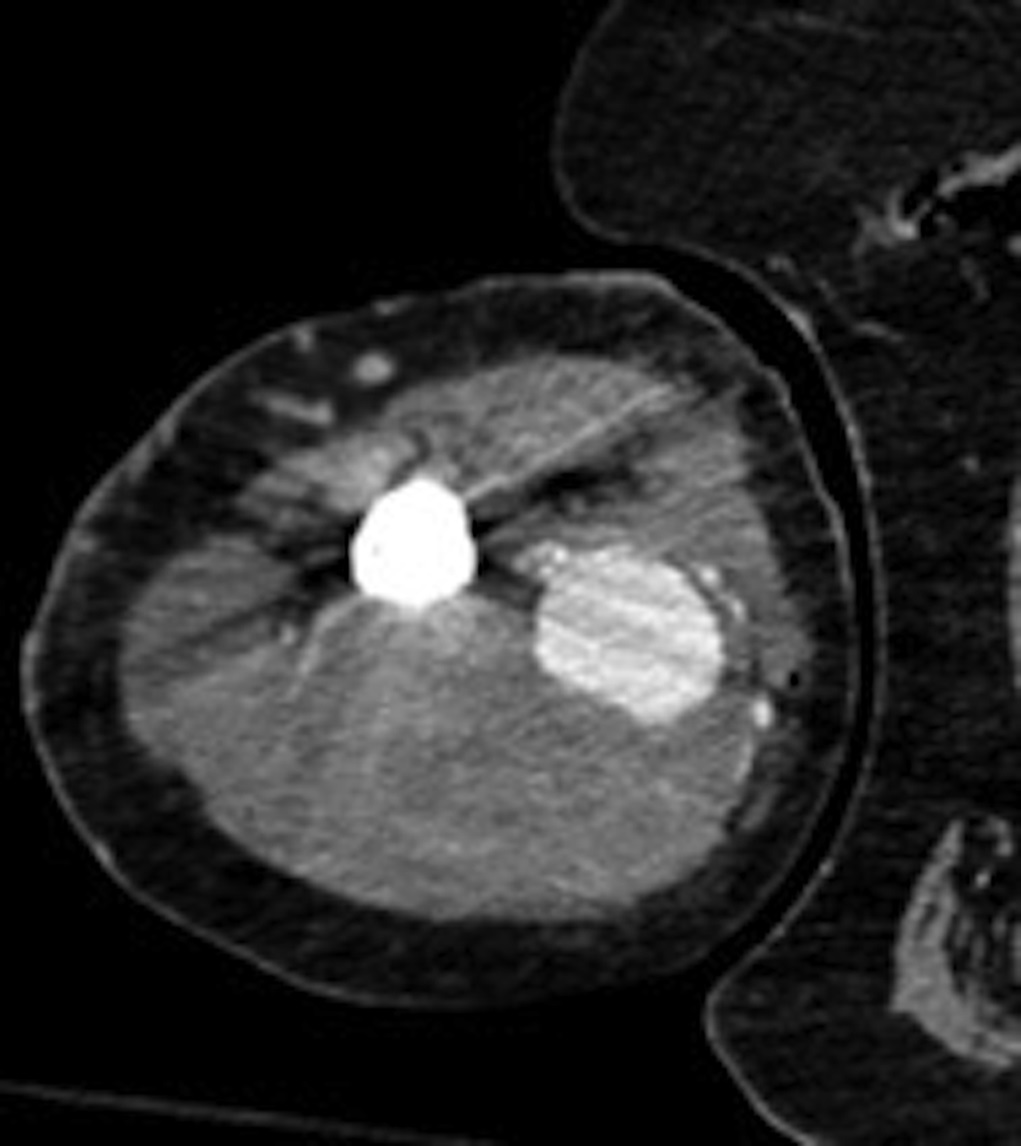

 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 1-C
Fig. 1-C Fig. 1-D
Fig. 1-D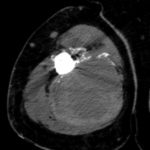 Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B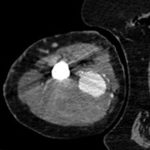 Fig. 2-C
Fig. 2-C Fig. 2-D
Fig. 2-D Fig. 3-A
Fig. 3-A Fig. 3-B
Fig. 3-B Fig. 4-A
Fig. 4-A Fig. 4-B
Fig. 4-B