A 14-Year-Old Boy with Leg Pain Following Fracture-Healing
July 5, 2018
A 14-year-old otherwise healthy boy with no surgical or family history of musculoskeletal pathology presented for referral after sustaining a transverse fracture of the distal aspect of the right tibia 3 months prior in a low-energy accident (he had been hit by a soccer ball) (Fig. 1). The referring physician had prescribed a walking boot and crutches. On evaluation at our institution, the patient was noted to have pain, a limp, and bowing of the right lower leg, and he reported that he had not been using the boot or the crutches. The medical history was remarkable only for a deep bite wound from a dog on the right lower leg 2 years prior, which had healed after 6 months. The vital signs were within normal limits, and physical examination noted mild tenderness to palpation over the right tibia. Standing radiographs demonstrated a transverse fracture of the distal aspect of the tibia with interval callus formation and a varus deformity of 15° (Fig. 2) when compared with the radiographs that were taken immediately after the injury. The leg was placed in a short cast, and activity was restricted.
Over the next month, persistent symptoms and a progressive varus deformity prompted us to obtain dual x-ray absorptiometry (DXA), magnetic resonance imaging (MRI), and computed tomography (CT) of the right lower extremity, and interventional radiologists performed a percutaneous bone biopsy. While the DXA scan was within normal limits, MRI and CT revealed persistent nonunion, cystic spaces in the marrow and the cortex, and soft-tissue involvement, concerning for a subacute chronic infection (Figs. 3-A and 3-B). The infectious disease service was consulted for management. The core biopsy and fine needle aspiration results were negative, but showed necrotic bone with some evidence of fracture-healing.
The patient reported increased swelling and pain over the distal aspect of the tibia and difficulty with ambulation that required the use of a walking boot, but he remained afebrile and felt well overall.
Despite progress over the 5 months since referral (8 months after the soccer injury), the patient presented acutely to the emergency department with worsening pain, fever, difficulty with weight-bearing, and shortness of breath. Empiric ceftriaxone and vancomycin therapy was initiated, and laboratory testing revealed mild leukocytosis (14.59 × 103/μL) with 88% neutrophils; the erythrocyte sedimentation rate (ESR) and the C-reactive protein (CRP) level remained within normal limits. Radiographs showed a hypertrophic nonunion of the distal aspect of the right tibia with stable varus alignment and soft-tissue swelling (Fig. 4-A). An MRI is shown in Fig. 4-B.
During hospitalization, the patient underwent multiple irrigations and debridements (Fig. 4-C) and a second open biopsy, which showed histopathologic findings consistent with chronic osteomyelitis. Bacterial and fungal culture results and acid-fast bacilli stain results were again negative. A sample was subsequently sent out for 16S ribosomal (r) RNA polymerase chain reaction (PCR) analysis, which identified Haemophilus parainfluenzae. Oral levofloxacin and trimethoprim/sulfamethoxazole therapy was started, and the patient was discharged home with the plan for additional staged surgical intervention, including debridement and correction of the osseous deformity.
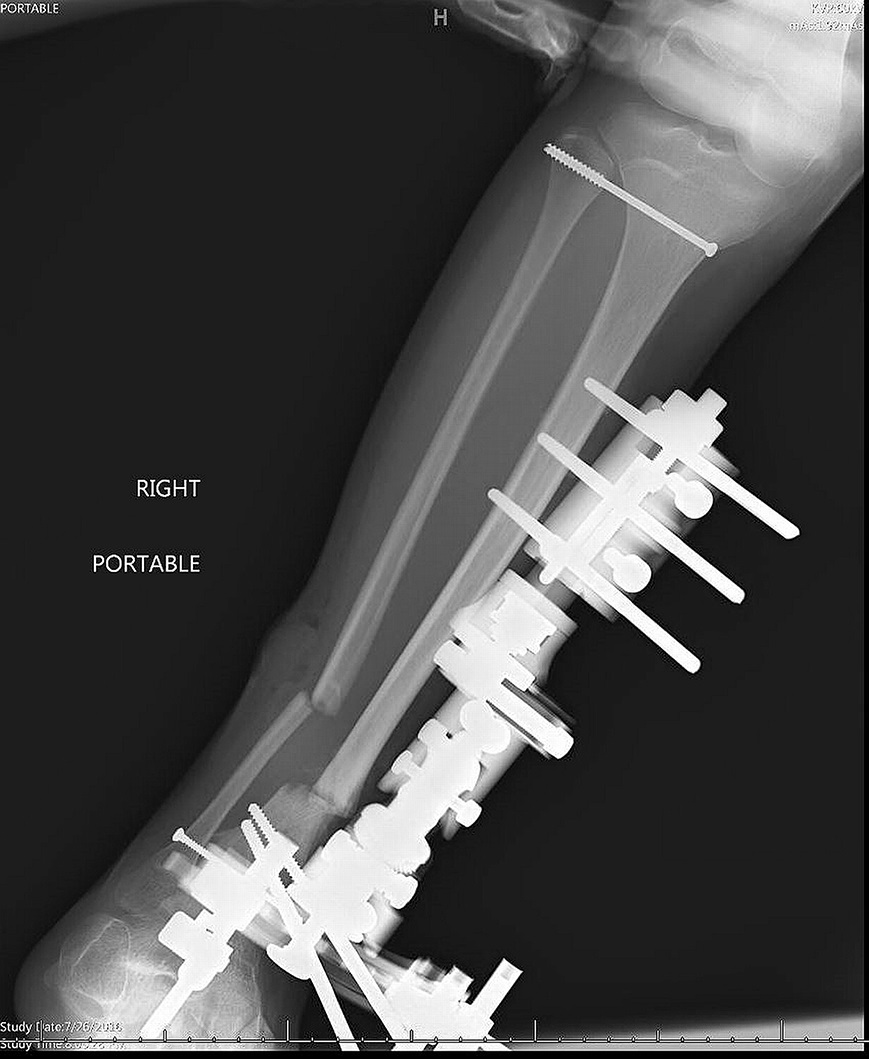
Seven months after presentation to our facility, the patient underwent irrigation and debridement of the infected site and a right tibial-fibular osteotomy, followed by external fixation to correct the varus deformity (Figs. 5-A and 5-B). The trimethoprim/sulfamethoxazole therapy was discontinued, and a year-long oral regimen of levofloxacin (500 mg daily) for the H. parainfluenzae as well as clindamycin (600 mg 3 times per day) for polymicrobial coverage of both the bone and the surgical site was begun. Four months postoperatively, the fixator was removed (Fig. 6), and the patient resumed unrestricted ambulation with a shoe lift to correct the resulting 4.8-cm leg-length discrepancy. It is likely that this discrepancy occurred as a result of the deformity and resection of the involved bone, with subsequent compression through the resection site. Lengthening of this extremity began at 8 months postoperatively, with a second tibial-fibular osteotomy at a different location and intramedullary nailing (Fig. 7). At the 5-month follow-up, he continued to do well and successfully had achieved approximately 4.9 cm of limb distraction.
Proceed to Discussion >>Reference: Ramachandran V, Haruno LS, Browne TS, Woc-Colburn LE, Rosenfeld SB, Shenava VR. Chronic osteomyelitis caused by Haemophilus parainfluenzae: a case report. JBJS Case Connect. 2018 Jan-Mar;8(1):e20.
Complex musculoskeletal infections in children can be difficult to diagnose and treat, and complications such as pathologic fractures, growth disruption, septic arthritis, or nonunion may occur. H. parainfluenzae is a fastidious gram-negative coccobacillus bacterium that is cultured on chocolate agar laced with nicotinamide adenine dinucleotide (NAD). This HACEK (Haemophilus species, Aggregatibacter species, Cardiobacterium, Eikenella, and Kingella species) organism is part of the normal flora in the human oropharynx and in the canine reproductive tract. While mostly nonpathogenic, H. parainfluenzae may cause endocarditis, biliary tract infections, meningitis, and, very rarely, musculoskeletal infections.
To our knowledge, there are only 16 previously reported cases of musculoskeletal infections caused by H. parainfluenzae. Of these prior cases, 11 had septic arthritis, 4 had osteomyelitis, and 1 had both. The median age of the affected individuals was >60 years old, and only 2 patients were ≤18 years old (both had septic arthritis). Reported treatments included antibiotic therapy in all cases and surgery in half. All of the previous cases of H. parainfluenzae osteomyelitis were within the vertebrae, the most common site of adult osteomyelitis.
Because of its precise growth requirements, H. parainfluenzae is difficult to isolate in nonspecific media. In our patient, multiple culture specimens were negative. However, broad-spectrum 16S rRNA PCR analysis is a relatively newer diagnostic method based on gene sequencing that allows enhanced identification of pathogens compared with traditional cultures. 16S rRNA PCR analysis should be considered for culture-negative specimens or in individuals with prior use of antibiotics and persistent symptoms.
Invasive medical procedures and preexisting medical conditions can predispose to H. parainfluenzae infection. Our patient did have a risk factor: the history revealed a previous dog bite that resulted in injury to the distal aspect of the right tibia with delayed wound-healing. Although we did identify a case report from 1974 describing an unusual incidence of osteomyelitis in a 14-year-old caused by H. hemoglobinophilus (canis), we did not find any cases recounting traumatic inoculation of H. parainfluenzae leading to osteomyelitis.
We speculate that the dog bite introduced polymicrobial pathogens, serving as a nidus for infection. It is also possible that the infection was hematogenous and related to minor trauma associated with the soccer injury. Within the tibia, these pathogens may have caused a low-grade chronic osteomyelitis that weakened the bone. This predisposed the patient to a pathologic fracture from a low-energy injury. Fracture and hypertrophic nonunion are well-documented sequelae of chronic osteomyelitis. The initial treatment with clindamycin may have selected out the H. parainfluenzae (a less virulent bacteria). Although only H. parainfluenzae was identified after repeated biopsy and culture, this patient’s chronic osteomyelitis was likely a polymicrobial process. Thus, both levofloxacin and clindamycin were prescribed. For similar cases in the future, it is recommended to begin treatment conservatively, and move to open biopsy when necessary. If there is residual symptomatic or cosmetic deformity, corrective surgery may be considered once complete healing of the infected site is confirmed or when the patient has returned to near baseline function.
In summary, H. parainfluenzae is a highly unusual and previously undocumented cause of pediatric osteomyelitis. H. parainfluenzae should be considered in patients with chronic osteomyelitis and repetitive negative culture specimens or in those with a history of traumatic inoculation with oral flora. This case emphasizes the complexity of musculoskeletal infections and the multidisciplinary approach that is necessary for effective management.
Reference: Ramachandran V, Haruno LS, Browne TS, Woc-Colburn LE, Rosenfeld SB, Shenava VR. Chronic osteomyelitis caused by Haemophilus parainfluenzae: a case report. JBJS Case Connect. 2018 Jan-Mar;8(1):e20.
What is the diagnosis?
Osteomyelitis
Adamantinoma
Langerhans cell histiocytosis
Periosteal osteosarcoma
Periosteal Ewing sarcoma



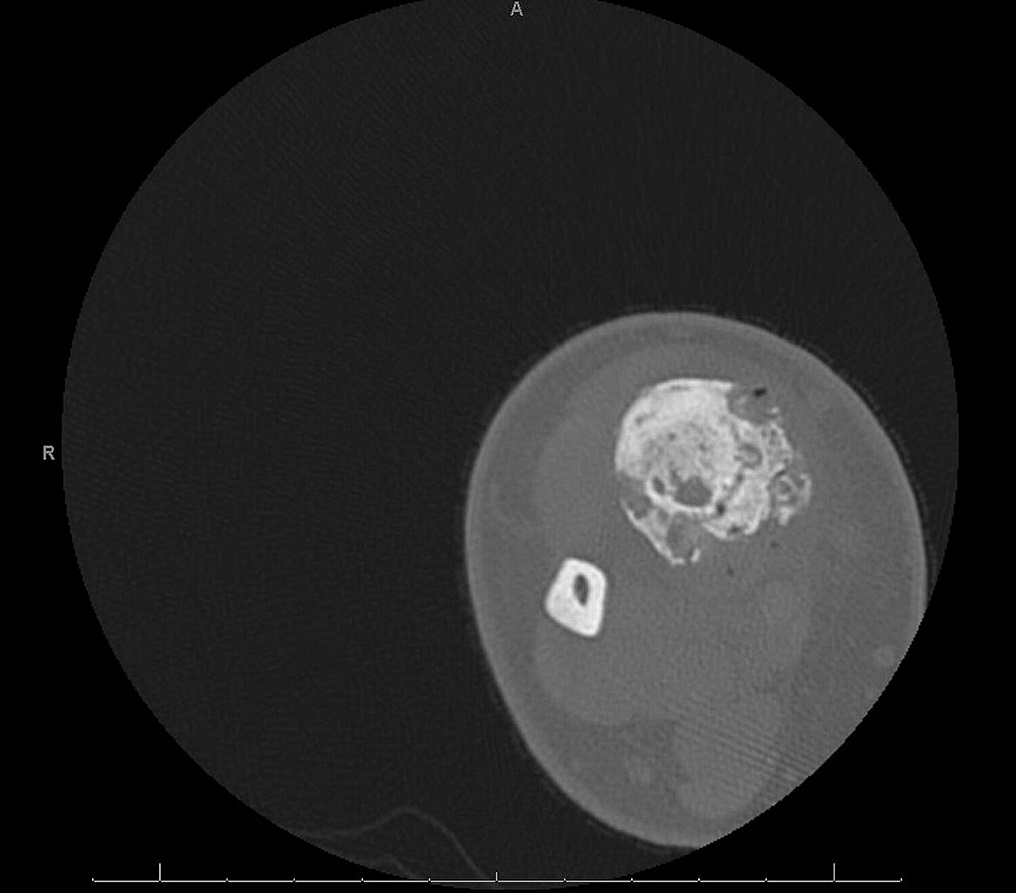



 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3-A
Fig. 3-A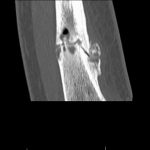 Fig. 3-B
Fig. 3-B Fig. 4-A
Fig. 4-A Fig. 4-B
Fig. 4-B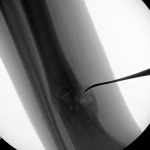 Fig. 4-C
Fig. 4-C Fig. 5-A
Fig. 5-A Fig. 5-B
Fig. 5-B Fig. 6
Fig. 6 Fig. 7
Fig. 7