A seventy-three-year-old woman of Dominican descent presented to our emergency department with the sudden onset of severe right groin pain while walking. The known past medical history included hypothyroidism and well-controlled type II diabetes mellitus. She denied any antecedent trauma or injury; however, she had experienced a three-week prodrome of dull pain to the right groin. Furthermore, she also had a several-year history of low back and bilateral knee pain. She had been an active community walker prior to presentation; she occasionally had used a cane for assistance outside the home because of the pain in the hips and the knees.
On examination in the emergency department, the right lower extremity was shortened and externally rotated. She had tenderness to palpation over the groin and experienced pain with the log roll and axial load tests. She also had flexion contractions of 30° of the hips and the knees bilaterally. The neurovascular examination was normal. Upon closer inspection, the patient was found to have mild increased pigmentation of the sclera and pinna of the ears.
Radiographs of the right hip (anteroposterior and cross-table lateral) and pelvis (anteroposterior) revealed a vertically oriented displaced fracture of the femoral neck (Figs. 1-A and 1-B). There was symmetric joint space narrowing about the hip joints bilaterally, as well as subchondral erosions and cysts. Additionally, there was overall relative radiolucency of the bone and extensive enthesopathy diffusely about the lumbar spine transverse processes, the iliac wings, the anterior superior iliac spines, the anterior inferior iliac spines, and the ischial tuberosities.
Given the extensive joint space narrowing and degenerative changes about the hip as well as the relatively high level of functioning and walking capacity, the patient was scheduled for a right total hip arthroplasty. At the time of surgery, the soft tissues, including the iliotibial band overlying the greater trochanter, the trochanteric bursa, the hip capsule, and the articular cartilage, were found to be stained with dark pigment (Figs. 2-A and 2-B).
Postoperatively, the patient’s urine and blood were collected for additional analysis. The urine became darkly pigmented upon exposure to air (Fig. 3). Histology of the femoral head revealed fragmentation and deep fissuring of the articular cartilage, as well as some brown-black extracellular pigmentation of the hyaline cartilage (Fig. 4).
The patient was diagnosed with femoral neck fracture and ochronosis (alkaptonuria). Postoperatively, the patient progressed well. By two months after the total hip arthroplasty, the right hip pain had resolved. She walked with a walker and was limited only by bilateral knee pain. At the one-year follow-up, she was walking with only a cane, but she continued to be limited by bilateral knee pain; the right hip was pain-free.
Proceed to Discussion >>Reference: Park BK, Egol KA. Displaced insufficiency femoral neck stress fracture in the setting of ochronosis: a case report. JBJS Case Connect. 2014 Jan-Mar;4(1):e21.
Atraumatic insufficiency fractures of the hip account for approximately 3% of all hip fractures. However, the incidence of stress fractures in the elderly is not well defined. Stress fractures are usually incomplete, but they can progress to complete displaced fractures with minimal or no trauma. Femoral neck stress fractures are classified as either compression-type fractures, occurring on the inferomedial neck, or tension-type fractures, occurring on the superolateral neck. Tension-type fractures are more common in the elderly population. Moreover, stress fractures in the elderly are also considered insufficiency fractures but different from stress fractures that occur because of abnormal loading. As in our case, elderly patients with insufficiency femoral neck stress fractures usually experience a prodrome of pain.
To our knowledge, femoral neck stress fracture in the setting of ochronosis previously has only been reported once. As described in the nurse anesthetist literature, a sixty-three-year-old man was found to have a nondisplaced femoral neck stress fracture on magnetic resonance imaging after a one-week history of severe hip pain. Our patient was an elderly woman who previously had not been diagnosed with ochronosis and osteopenia but presented with a complete displaced femoral neck fracture. In light of the absence of any trauma, the presence of a vertically oriented fracture line, and the prodrome of pain, we propose that the patient had developed a tension-type insufficiency femoral neck stress fracture, which had progressed to completion and displacement during normal walking.
Insufficiency stress fractures in elderly patients have a well-known association with osteoporosis. However, with limited literature on increased bone turnover, altered collagen cross-linking, osteocyte damage, and decreased bone mineral density in the setting of ochronosis, there is no established metabolic connection between osteoporosis and ochronosis. Concomitant osteopenia/osteoporosis may be unrelated or secondary to disuse of the painful joint.
One study attempted to address the treatment of osteoporosis in the setting of ochronosis. This small case series investigated four subjects with ochronosis and documented osteoporosis. Each patient was treated with oral bisphosphonates in an attempt to slow the deterioration of bone mineral density. After two years of bisphosphonate therapy, continued rapid decrease in bone mineral density was reported. Furthermore, two of the patients developed stress fractures, and one sustained a femoral neck fracture two months after completing a two-year course of alendronate. The authors theorized that bisphosphonate therapy was ineffective in treating these osteoporotic patients because of the effects of homogentisic acid. Therefore, prevention of hip fractures in the ochronotic population may be more difficult.
We recommend that clinicians have a heightened suspicion for stress fractures in patients with ochronosis who present with increased hip or groin pain. Because these patients also present with arthropathy due to intra-articular homogentisic acid deposition, it is important to differentiate the source of pain. Not recognizing a stress fracture may lead to eventual displaced fractures and potential complications with surgery, as well as a higher risk of osteonecrosis, malunion and nonunion, and the associated morbidity of hip fractures in the elderly.
Alkaptonuria is a rare condition; its relationship to stress fractures has not been established. Early recognition of alkaptonuria and its musculoskeletal manifestations may be helpful in the prevention and treatment of degenerative arthritis, stress fractures, and insufficiency fractures.
Reference: Park BK, Egol KA. Displaced insufficiency femoral neck stress fracture in the setting of ochronosis: a case report. JBJS Case Connect. 2014 Jan-Mar;4(1):e21.
What is the diagnosis?
Metastatic malignant melanoma with pathologic fracture
Femoral neck fracture and ochronosis (alkaptonuria)
Femoral neck fracture and metallosis
Atypical femoral fracture
Femoral neck fracture and bone discoloration from previous tetracycline use


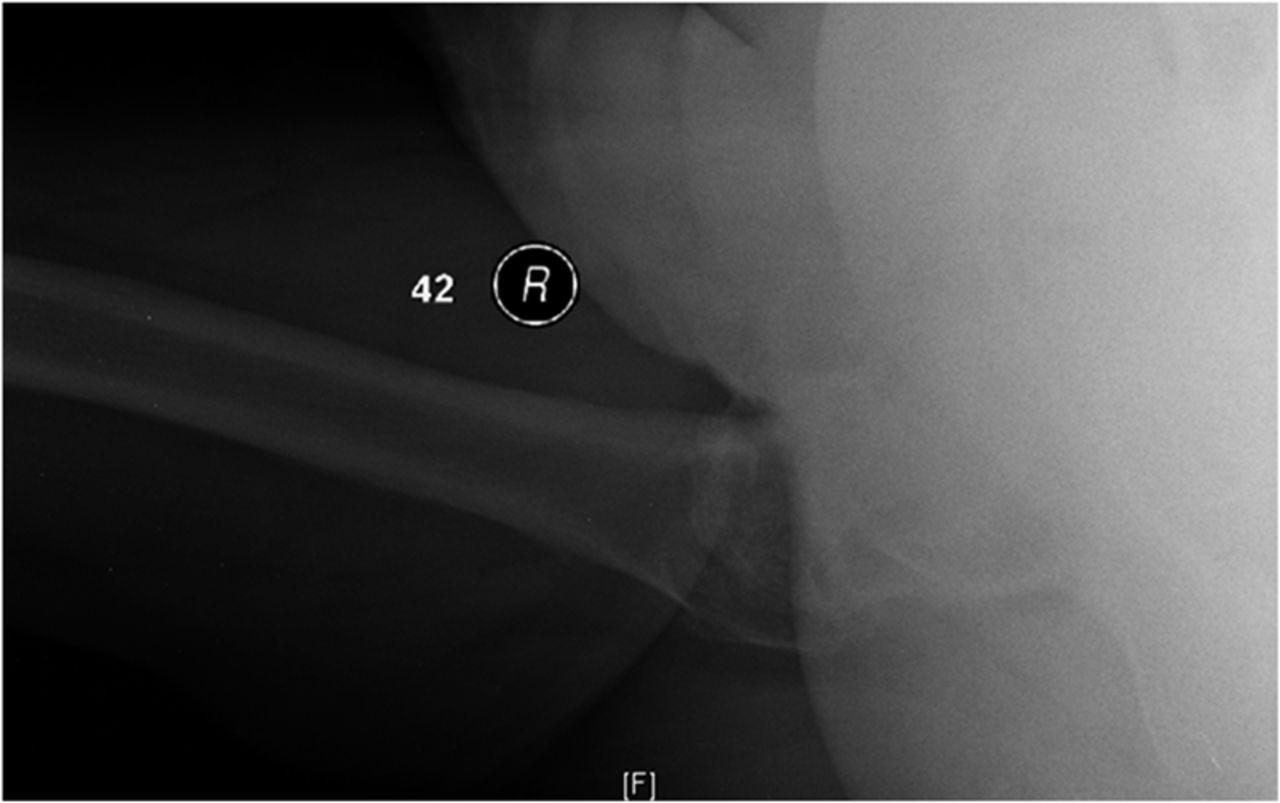
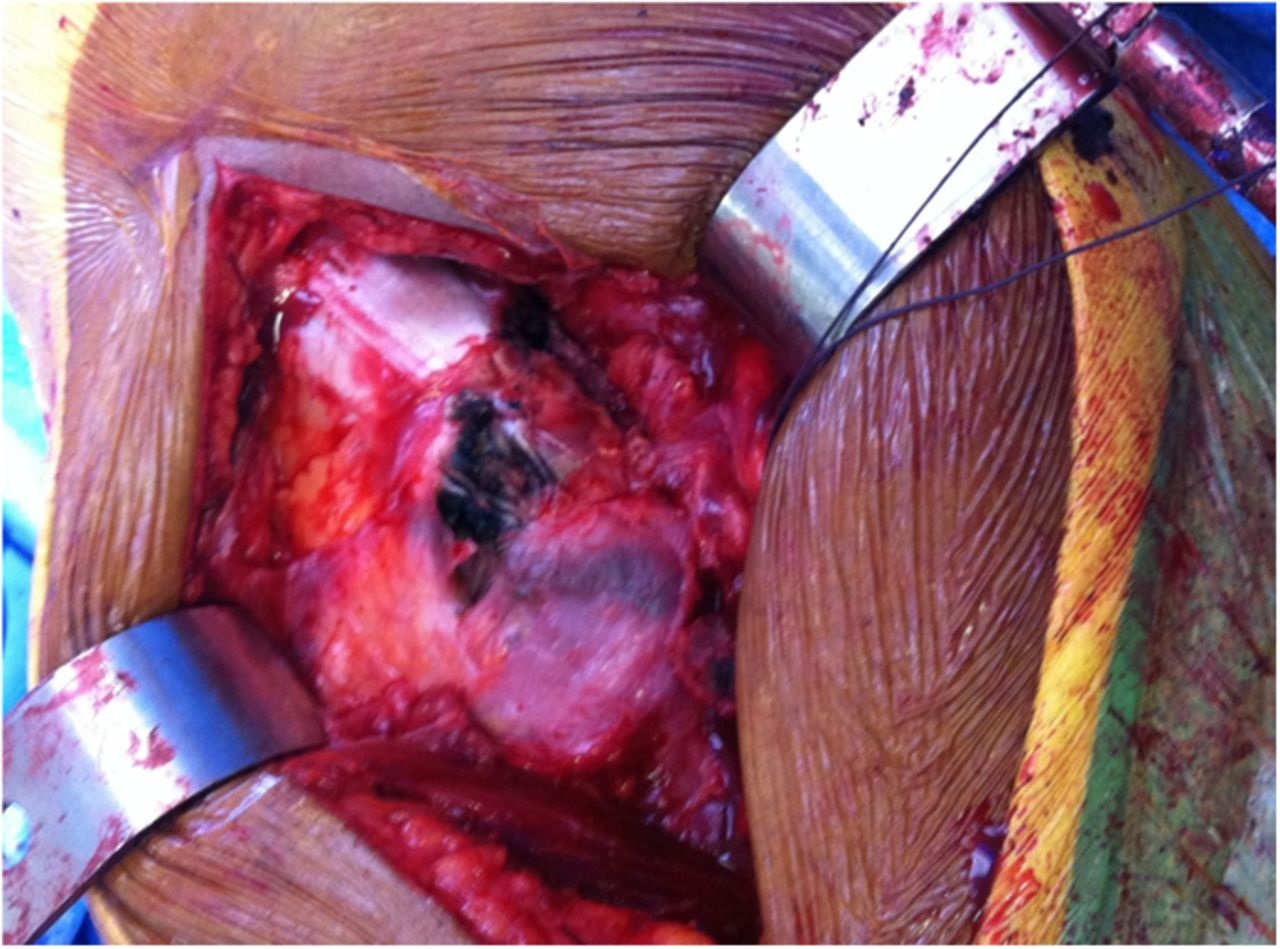



 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B Fig. 3
Fig. 3 Fig. 4
Fig. 4