A 19-Year-Old Woman with Growing Pain and Swelling in the Hip
August 15, 2018
A 19-year-old woman was referred to the orthopaedic oncology service with a 3-month history of a slowly enlarging lesion on the proximal aspect of the right femur. The medical and surgical histories were noncontributory. The symptoms had begun with nagging pain in the right hip, which became persistent and increased in intensity, especially after shifts at her job as a server. She did not recall any inciting traumatic incident other than a fall down the stairs when she had hit her head 4 months prior. She had not noted any loss of consciousness after the fall; however, she had experienced a severe headache, nausea, and blurred vision. When this had not improved the next day, she had presented to an urgent care center for evaluation, where she had been diagnosed with a concussion. She had not had any head imaging done at that time. The symptoms had resolved over the next week. She had not noted any trauma to the thigh at that time, nor any pain in the thigh afterward, and had not noticed any issues with ambulation. Over the course of 2 to 3 months, the thigh pain and local swelling increased in intensity and began hindering her sleep. She did not have any erythema to the area. The pain was worse at night and intensified with walking and standing for long periods of time. She initially managed the pain with oral nonsteroidal anti-inflammatory drugs (NSAIDs), but eventually the pain progressed.
On examination, the patient had an 8 × 8-cm, firm, immobile mass in the proximal aspect of the right thigh that was tender to palpation. She had full hip range of motion, with pain at extremes of motion. Radiographs revealed a well-circumscribed soft-tissue-based mass that was intimately associated with the anterior cortex of the proximal aspect of the femur, with an indeterminate mineralization pattern of osteoid or egg-shell configuration, which appeared slightly more mature at the 4-week follow-up (Figs. 1-A and 1-B). Subsequent computed tomography (CT) demonstrated primarily peripheral curvilinear mineralization, with some areas of developing cortical bone. Some finer central mineralization and mild anterior cortical reaction were noted (Figs. 2-A and 2-B). Concurrent magnetic resonance imaging (MRI) showed T2-weighted hyperintensity and mild T1-weighted high signal intensity of the mass, with surrounding T2-weighted signal intensity with edema in the anterior thigh musculature (Fig. 3). There was central postcontrast enhancement without fluid elements or fluid-fluid levels. A CT-guided core needle biopsy of the mass was performed, which was inconclusive. Subsequently, an open biopsy was performed to further characterize the mass (Figs. 4 and 5).
The open biopsy was interpreted as heterotopic ossification (HO) with no evidence of malignancy.
Because of the results of the 2 biopsies and the symptomatic nature of the mass, the patient elected to proceed with resection. The mass was successfully removed from the proximal aspect of the femur and the surrounding musculature, and it appeared to be localized to the origin of the vastus intermedius. There were no surgical complications. At 12 months after excision, there had been no recurrence (Figs. 6-A and 6-B). Pathology confirmed the diagnosis of HO, and the patient recovered from surgery uneventfully.
Proceed to Discussion >>Reference: O’Callaghan PK, Carter E, Walton Z, Chapin R, Bruner E. Heterotopic ossification formation following a simple concussion: a case report. JBJS Case Connect. 2018 Apr-Jun;8(2):e26.
To the best of our knowledge, this is the first case report of HO associated with a concussion. HO develops as a formation of bone in nonskeletal tissue, typically between the joint capsule and the muscle of the affected limb. Clinically, this presents as warmth, swelling, pain, and a substantial reduction in range of motion. This may cause HO to be mistaken for other inflammatory disorders, such as infectious myositis, osteomyelitis, and cellulitis. Additionally, the clinical and imaging presentation, including postcontrast enhancement, mimics that of soft-tissue sarcoma.
The most common entities that are associated with the development of HO include traumatic brain injury (TBI), spinal cord injury (SCI), trauma to the affected limbs, and surgical insults. However, HO also has been reported in cases of tetanus, poliomyelitis, tabes dorsalis, syringomyelia, myelitis, myelodysplasia, anoxic brain damage, and stroke. Although relatively uncommon (HO occurs in approximately 11% of patients with TBI and in 20% of patients with SCI), HO can seriously impair a patient’s life.
To clinically differentiate HO from other inflammatory disorders in the differential diagnosis, a rise in serum alkaline phosphatase may be helpful. Radiographs demonstrate mineralization, which is not expected in the initial presentation of myositis and has a more peripheral zonal distribution than that expected with osteosarcoma. There are rare reports of soft-tissue aneurysmal bone cysts that have less robust mineralization than HO on CT and that demonstrate large areas of nonenhancing hemorrhage with fluid-fluid levels on MRI. Ultimately, a biopsy may be necessary to help distinguish these entities. The timing of HO occurrence varies from 4 to 12 weeks after injury, with a peak around 2 to 3 months, although this delay may lead to difficulty in establishing the diagnosis early on.
Various treatments options that help to reduce symptoms and prevent the recurrence of HO exist, although their efficacy is debated. Treatment with NSAIDs, specifically indomethacin, is reported to reduce HO formation and patient discomfort, especially in patients with SCI; however, the use of NSAIDs is limited by their various side effects. In addition, treatment with radiation therapy reportedly is effective at slowing HO formation in patients with neurologic injuries, although radiation treatment can result in various complications, such as wound-healing complications, osteonecrosis, and a risk of late sarcoma development, as demonstrated in recent case reports. Surgical resection is often chosen as treatment for HO that has not been receptive to nonoperative management, especially in patients with a neurologic basis. The timing of the resection is important in order to allow sufficient time for maturation and prevention of recurrence. Surgical resection is controversial. Recommendations for surgical resection timing range from 4 months to 2 years after diagnosis. Unfortunately, recurrence is common in patients with neurologic HO, even after surgical resection, with estimates that approximately 20% of patients experience some symptomatic HO recurrence.
TBI is a complex disease with many causes and a large spectrum of severity. Typically, the severity of TBI is determined by the Glasgow Coma Scale, with scores ranging from 13 to 15 for mild TBI (mTBI), from 9 to 12 for moderate TBI, and from 3 to 8 for severe TBI. Acute injuries include skull fractures, intracranial hematomas, and deformation and destruction of brain tissue. While the terms concussion and mTBI traditionally have been used interchangeably, there has been a recent push toward classifying them differently, with the spectrum including subconcussive blows, concussion, mTBI, and TBI, although currently there are no distinct criteria for this classification. mTBI also has been defined as a head trauma that produces (1) a loss of consciousness of ≤30 minutes, (2) posttraumatic amnesia, (3) any alteration in mental state at the time of the injury, or (4) a focal neurologic deficit. Given that our patient did not lose consciousness or suffer memory loss, we would classify her as having a concussion rather than mTBI. Although on the low end of the spectrum, concussions still pose a serious risk to any affected individuals. As athletes continue to engage in high-energy contact-based physical activities, the incidence of concussion continues to increase at an alarming rate. The Centers for Disease Control and Prevention (CDC) estimates that approximately 1.6 to 3.8 million concussions occur in sports and recreational activities in the U.S. annually. In a study of 17,000 football players, 5.1% experienced a concussion during a 3-year period, and those with a previous concussion were 3 times more likely to experience a second concussion during the same season; 30.8% of those with a concussion returned to play the same day. This prevalence of early return to play places these individuals at a substantial risk of neurologic injury and second-impact syndrome, a sequence that includes a space-occupying hematoma and rapid brain swelling, which often results in permanent damage.
To our knowledge, this is the only case report describing HO formation associated with a concussion and no other risk factors. When evaluating patients with masses who present with a differential diagnosis that includes HO, it may be useful to ask about recent or remote concussions that the patient may have sustained.
Reference: O’Callaghan PK, Carter E, Walton Z, Chapin R, Bruner E. Heterotopic ossification formation following a simple concussion: a case report. JBJS Case Connect. 2018 Apr-Jun;8(2):e26.
What is the diagnosis?
Extraskeletal osteosarcoma
Parosteal osteosarcoma
Soft-tissue aneurysmal bone cyst
Heterotopic ossification
Juxta-articular osteochondroma

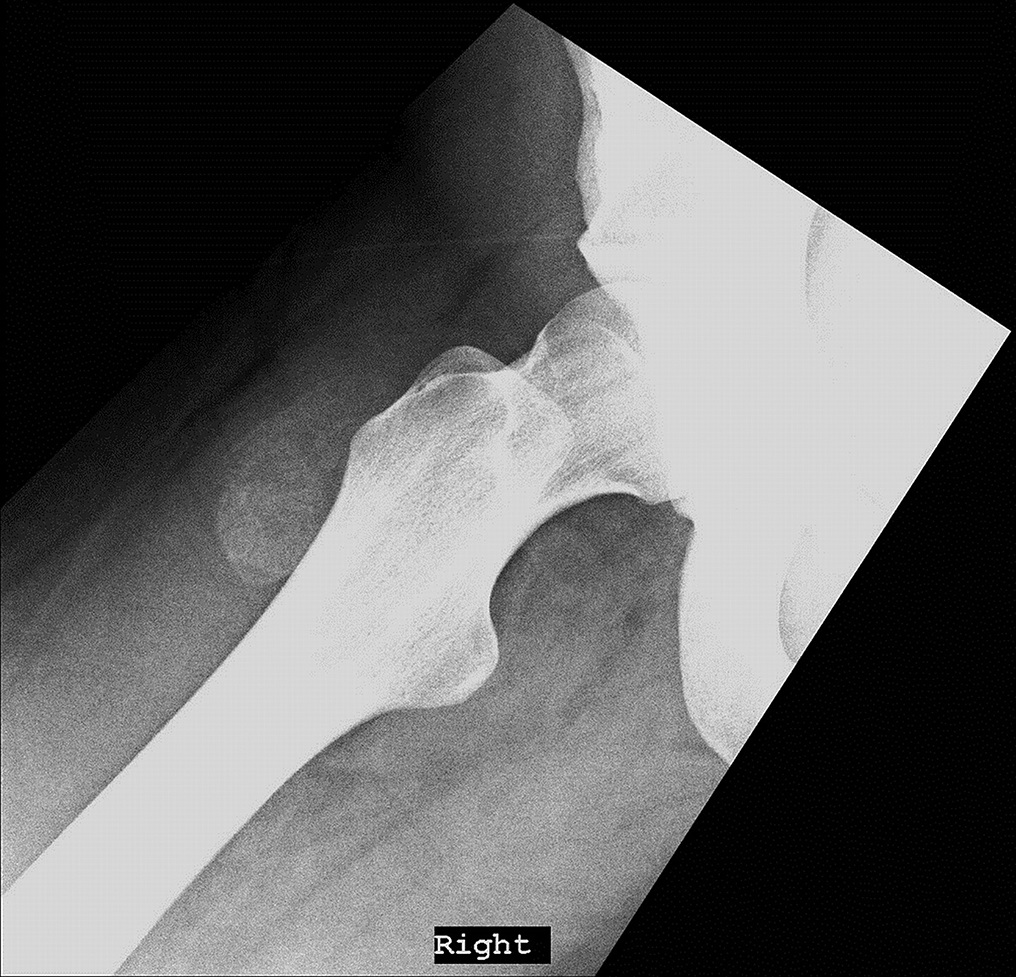



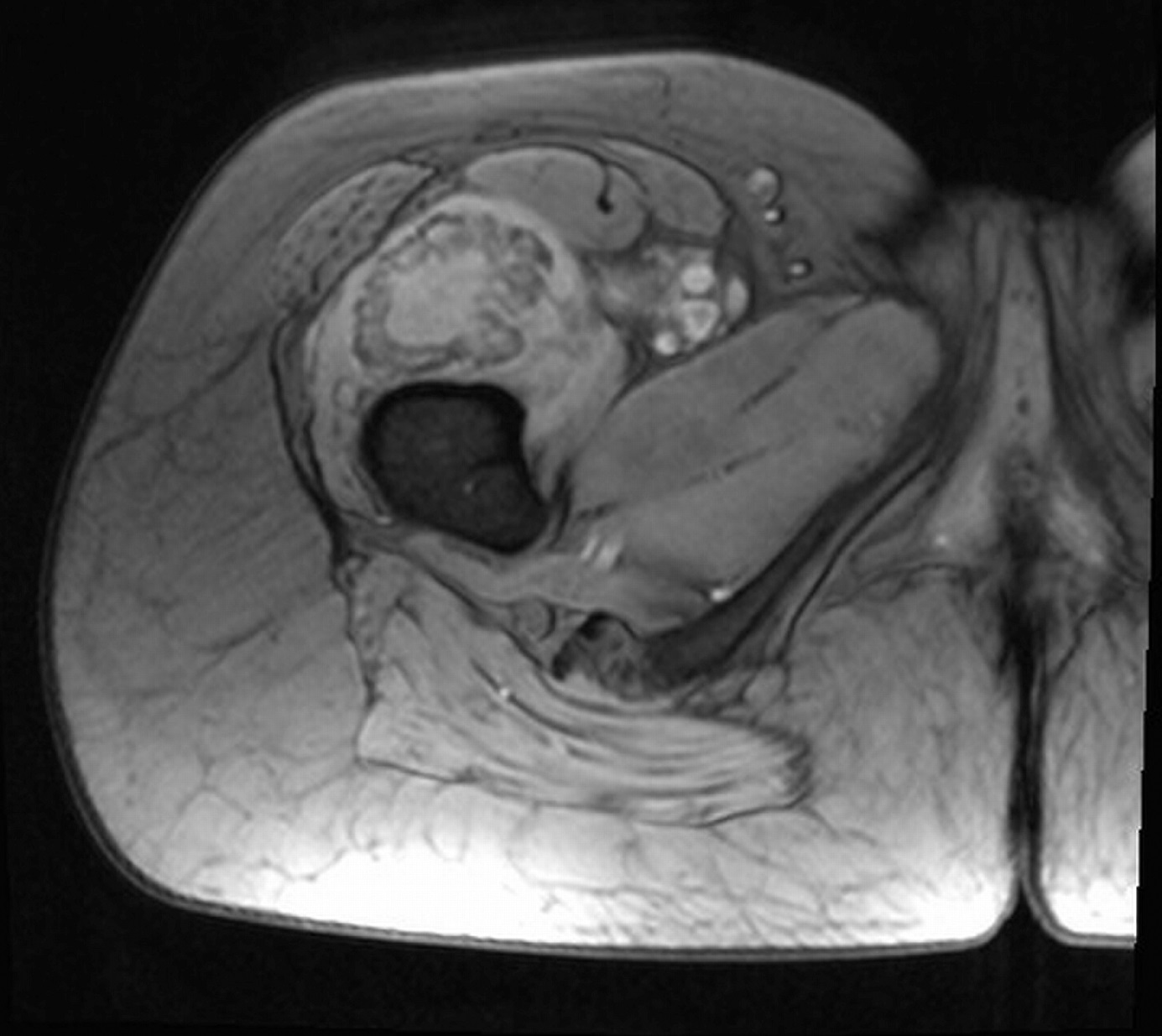
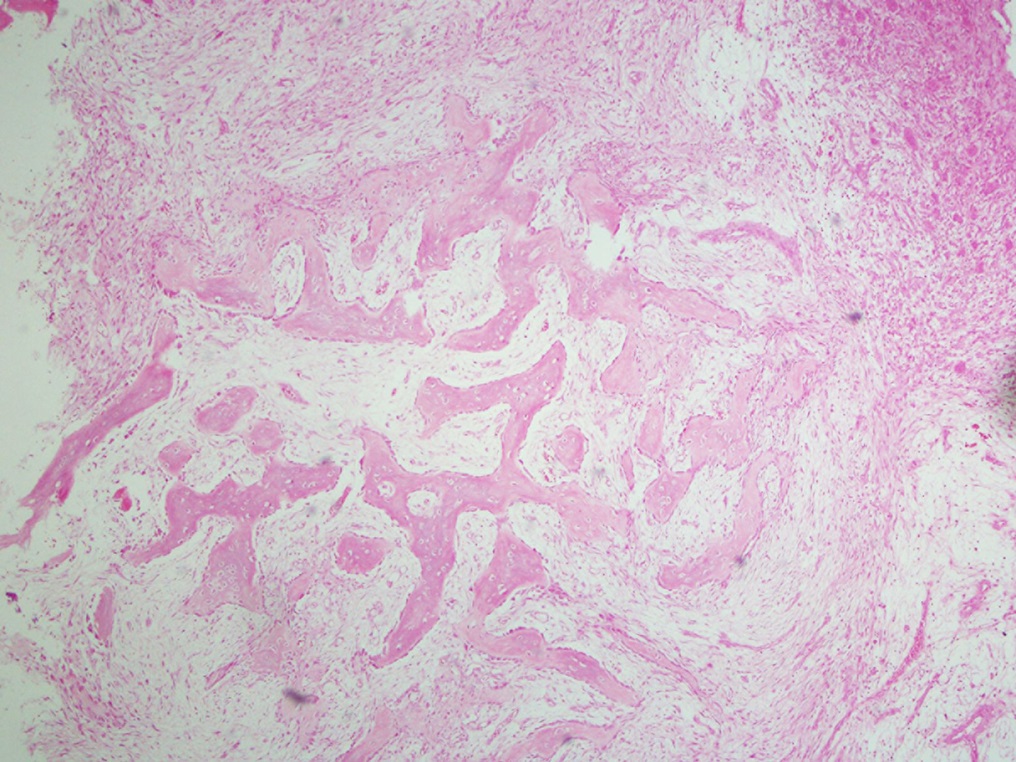
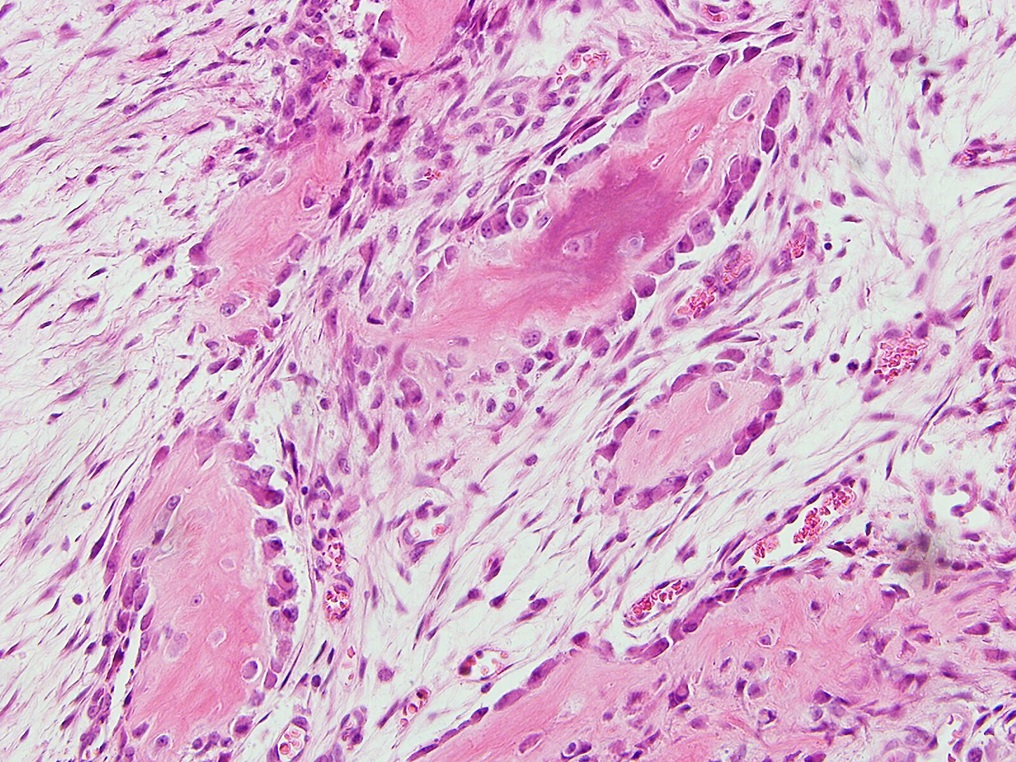
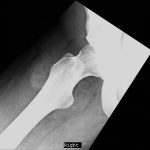 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B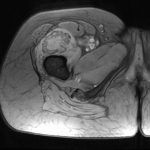 Fig. 3
Fig. 3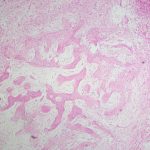 Fig. 4
Fig. 4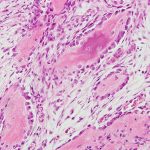 Fig. 5
Fig. 5 Fig. 6-A
Fig. 6-A Fig. 6-B
Fig. 6-B
