A 44-year-old man presented with 1 year of worsening, chronic right hip pain. He described severe symptoms that were localized to the right groin and radiated to the thigh. The pain was exacerbated when getting up from a sitting position, and he became functionally debilitated secondary to the worsening pain. He also reported difficulty reciprocating stairs, requiring the banister for support. He stated that there had been no traumatic injury to the right hip. Prior to presentation, he had undergone 4 intra-articular injections in the right hip that had provided temporary pain relief.
On examination, the patient had a body mass index (BMI) of 34.27 kg/m2. Hip flexion was to 90° with pain, internal rotation in flexion was to 5°, external rotation in flexion was to 10°, and abduction was to 35°. He exhibited no weakness and was neurovascularly intact distally.
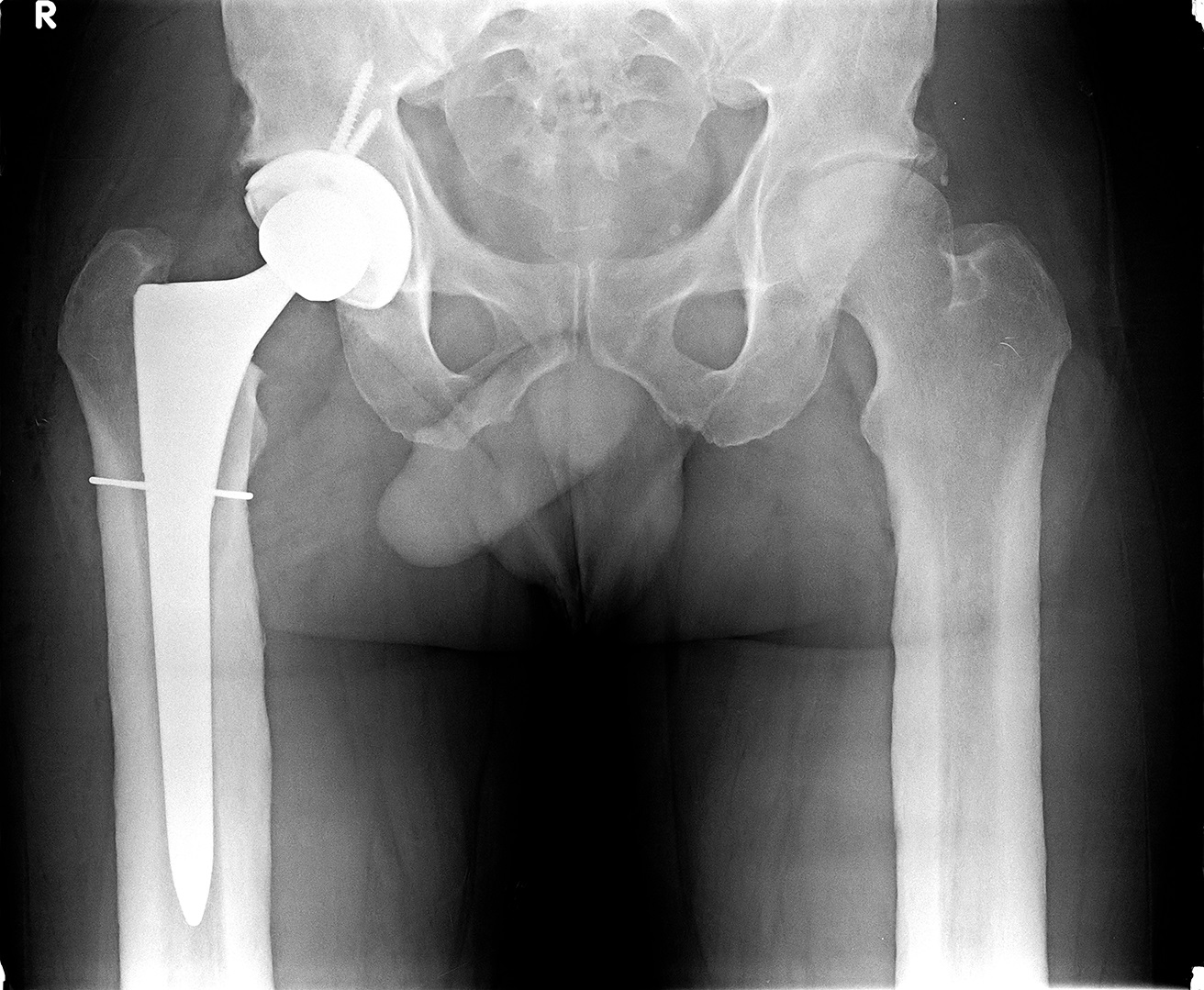
Radiographs demonstrated bilateral femoral cortical thickening exhibited in the diaphysis of the long bones (Figs. 1 and 2). Additionally, substantial joint space narrowing and subchondral sclerosis consistent with right hip osteoarthritis were noted (Fig. 3). A right total hip arthroplasty was recommended, and after discussion of the risks and benefits of the procedure, a shared decision was made to proceed with the surgery.
The clinical and radiographic features, especially bilaterally symmetric cortical thickening, most prominent in the diaphysis with epiphyseal sparing, were interpreted as diaphyseal dysplasia (Camurati-Engelmann disease).
The patient completed all of the appropriate preoperative medical evaluations and optimization for surgery. The senior surgeon routinely uses an uncemented construct that consists of a cluster-hole cup with a modern, highly porous ingrowth surface (R3; Smith & Nephew), a ream-and-broach dual-taper stem (SYNERGY; Smith & Nephew) with a sintered-bead porous coating at the primary ingrowth surface of the proximal one-third of the stem, and a grit-blasted 3°-tapered distal surface with 3 fins for rotational stability. Considering how Camurati-Engelmann disease primarily affects the bone diaphysis rather than the metaphysis, we determined the metaphysis to be the more optimal location for fixation. Furthermore, the sclerosing effect on the diaphysis results in metaphyseal-diaphyseal mismatch, which was addressed by reaming the diaphysis and broaching to fill the metaphysis. Given the unknown bone quality, cemented stem and cup systems also were readily available as backups. Templating for the restoration of leg lengths and the femoral offset took into account the length of the neck cut, the acetabular component size and position, and the femoral component size and offset. Finally, given the abnormal bone, we planned to have a cable system immediately available to be placed either prophylactically or for fixation, as needed.
A standard, contemporary “mini-posterior” approach to the right hip was used. The hip was dislocated without difficulty. The acetabulum was prepared in the routine fashion, and a press-fit acetabular shell (58 mm) was placed with excellent press-fit fixation. The senior surgeon’s preference is to place acetabular screws in all cases; therefore, 2 acetabular screws were placed in the posterosuperior quadrant. Given the excellent fixation, it was felt that inferior screws were not necessary.
The next step was to prepare the femur; reaming of the medullary canal proceeded uneventfully, beginning with the size-12 reamer and proceeding up in 1-size increments. The calcar and the quality of the bone were monitored closely with each subsequent reamer. As our reamer approached the template size 18, we noted that the bone was of good quality, although cortical bone was noted in the reaming debris much earlier than usual and well before adequate fit of the canal was obtained. The medullary canal remained patent and adequate. Broaching commenced carefully. A prophylactic cable was placed around the proximal aspect of the femur as the broaching size approached filling of the metaphysis. With a well-fitting broach in place (size 18, 180 mm in length), a trial reduction (36-mm head) was carried out, and stability throughout physiologic and supraphysiologic motion was ensured. Next, the trial components and the broach were removed, and the final implants were placed. Standard posterior capsule and piriformis repairs were carried out. Routine postoperative imaging was obtained, which showed appropriate alignment (Figs. 4 and 5).
Postoperatively, the patient was allowed weight-bearing as tolerated and advised to adhere to universal hip precautions. He mobilized quickly and walked with a walking aid (a rolling walker in the hospital). He was discharged home on postoperative day 3 following an excellent recovery with no complications. The patient was seen in clinic for routine follow-up visits at 2 weeks, 3 months, and 6 months, confirming an excellent recovery without issues. He advanced his walking and activity as tolerated. He was using a walker at the 2-week follow-up, and he was using a cane at the 3-month follow-up. At the 6-month follow-up, he was not using any walking aids.
Proceed to Discussion >>Reference: Ge DH, Yu S, Ziegler JD, Schwarzkopf R. Total hip arthroplasty in a patient with Camurati-Engelmann disease: a case report. JBJS Case Connect. 2018 Apr-Jun;8(2):e45.
The frequency of Camurati-Engelmann disease is estimated to be 1 in 1,000,000, with approximately 300 reported cases worldwide.
Camurati-Engelmann disease is linked with a missense mutation in transforming growth factor (TGF)-β1. The majority (82.2%) of mutations occur in exon 4, which encodes the region in the TGF-β1 latency-associated peptide that surrounds the residues that are responsible for homodimerization (Cys223 and Cys225). Exon-4 mutations cause early activation of the mature peptide and an increase in TGF-β1 activity. Under physiologic conditions, TGF-β1 stimulates bone formation and suppresses bone resorption. Thus, disruption in both osteoblast and osteoclast function leads to hyperostosis along the long bone diaphysis and sclerosis of the skeleton, which produces the clinical symptoms of limb pain or waddling gait.
It has been reported that a majority of patients demonstrate radiographic involvement of the long bones (94%), the pelvis (63%), and the skull (54%). The hallmark of the disorder is bilateral and symmetric cortical thickening of the long bone diaphyses, involving both the periosteal and endosteal surfaces. Increased tracer uptake in the femur, the lower legs, the humeri, and the forearms via scintigraphy can assist in early detection of the disease, even before sclerosis can be seen on radiographs.
Glucocorticoids have been found to downregulate TGF-β signaling and counteract the increased bone formation in patients with Camurati-Engelmann disease. They suppress the proliferation and differentiation of osteoblasts but enhance the proliferation and differentiation of osteoclast precursors. In particular, prednisolone has been shown to improve limb pain and fatigue. Although bisphosphonates are used in the treatment of osteoporosis, they have not been demonstrated to be effective in the treatment of Camurati-Engelmann disease. Losartan recently has been reported to relieve pain in a few cases because of downregulation of TGF-β type-1 and 2 receptor expression, but additional research needs to be performed to validate its widespread use.
Only 1 case of total hip arthroplasty in a patient with Camurati-Engelmann disease was found in the literature. However, reaming of the medullary canal or osteotomy have been reported to result in temporary remission of pain.
Our patient demonstrated advanced osteoarthritis of the right hip with debilitating pain that was not responsive to nonoperative treatment. A total hip arthroplasty was recommended. Given the rarity of Camurati-Engelmann disease, this was the first arthroplasty that we have performed on a patient affected by this disease. Furthermore, to our knowledge, this is the first reported case that utilized all uncemented components for total hip arthroplasty in a patient with Camurati-Engelmann disease. Preoperative planning was critical to ensure that we would be prepared to manage any quality of bone.
Given the narrowed medullary canal, we feel that a ream-and-broach system is the most applicable with these types of cases. A stem system in which conversion to a cemented version easily can be done is also recommended when there is concern regarding the bone quality or the ability to obtain metaphyseal fill. With our patient, we prophylactically placed a cable around the proximal aspect of the femur. We routinely recommend prophylactic placement of a cable prior to broaching in cases with dense, sclerotic cortical bone in which microscopic fractures, which may not be readily appreciated intraoperatively, may exist.
Reference: Ge DH, Yu S, Ziegler JD, Schwarzkopf R. Total hip arthroplasty in a patient with Camurati-Engelmann disease: a case report. JBJS Case Connect. 2018 Apr-Jun;8(2):e45.
What is the diagnosis?
Paget disease and osteoarthritis
Osteopetrosis, delayed type (Albers-Schönberg), and osteoarthritis
Endosteal hyperostosis (Van Buchem type) and osteoarthritis
Melorheostosis and osteoarthritis
Diaphyseal dysplasia (Camurati-Engelmann disease) and osteoarthritis




 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5
Fig. 5