A 26-Year-Old Man with Disorientation Following Leg Fracture
September 19, 2018
An otherwise healthy 26-year-old man presented after sustaining an isolated crush injury to the right lower extremity. He had been working at a factory when a slab of granite fell on his leg, with an estimated extraction time of 1 minute. On initial presentation, the patient was alert and oriented to person, place, and time. He provided a full history and was able to recall all of the details of the accident. The vital signs were within normal limits. There was a 2.5-cm oblique laceration to the anterior aspect of the tibia, with no gross contamination or arterial injury. The neurovascular examination was normal, and there were no signs of compartment syndrome. Radiographs demonstrated a displaced, transverse tibial and fibular shaft fracture (OTA/AO classification 42-A3) (Fig. 1). The wounds were irrigated at the bedside, a sterile dressing was placed, and the fracture was provisionally stabilized with a long leg plaster splint.
At 6 hours after injury (4 hours after presentation), the patient began to show signs of altered mental status and respiratory distress. He became confused and no longer oriented to time or place, as well as amnesic to the events prior to the accident. The heart rate was elevated, and the oxygen saturation dropped to 78% on room air, requiring 3 L of oxygen via nasal cannula to maintain an appropriate oxygen saturation. A chest radiograph showed evidence of noncardiac pulmonary edema (Fig. 2). No petechial rash was present, and the symptoms were attributed to the use of narcotics for pain control, which had been received in the emergency department.
Prior to surgical stabilization, the patient was treated with supportive oxygen and intravenous fluids. A preoperative medical and anesthetic workup was completed, and prompt surgical debridement and stabilization were dictated because of the grade-II open fracture. The patient was taken to the operating room within 24 hours of the injury for irrigation and debridement, and reamed intramedullary nailing was performed. The vital signs remained stable during the operation; however, he decompensated again immediately postoperatively. He became mentally altered, and the oxygen saturation dropped to 78% on room air. He required 10 L of oxygen to maintain a saturation of >92%. A bedside echocardiogram showed strain on the right side of the heart, and a chest radiograph demonstrated worsening bilateral pleural effusions (Fig. 3). A spiral computed tomography angiography (CTA) of the chest and noncontrast magnetic resonance imaging (MRI) of the head were performed (Figs. 4 and 5). A petechial rash was now visible on the torso.
The combination of symptoms and imaging findings led to the diagnosis of posttraumatic fat embolism syndrome (FES).
The patient improved from a respiratory standpoint with supportive treatment. However, he remained altered in orientation to place and time with dysarthria for 5 days postoperatively. He ultimately returned to the premorbid baseline pulmonary and neurocognitive status prior to discharge on postoperative day 8. The fracture achieved union, and the outcome was excellent at 3 months; however, the immediate postoperative course had been complicated by prolonged hospitalization and a short-term inpatient rehabilitation stay. He had returned to work at 3 months postoperatively with no residual deficits, and the last follow-up was at 12 months.
Proceed to Discussion >>Reference: Cronin KJ, Hayes CB, Moghadamian ED. Early-onset fat embolism syndrome: a case report. JBJS Case Connect. 2018 Apr-Jun;8(2):e44.
Even with many descriptions in the current literature, there is no universally accepted definition of FES. Gurd proposed a system with major and minor criteria in 1970; however, because of the complexity of the criteria, a simpler definition of hypoxia, petechial rash, and neurologic impairment typically is accepted. Debate mostly centers on the rate, morbidity, and mortality of this clinical entity. The original epidemiologic study by Ganong showed a rate of 23% in patients with isolated fractures of the femur and tibia in a population of otherwise healthy young skiers, who typically required prolonged hospitalization. More recent studies have shown the rate to be lower, with most authors in agreement that the rate is between 0.9% and 11% for isolated femoral and tibial fractures. In Gurd’s original 1970 paper, he estimated that 67% of trauma patients have some degree of fat embolism without any clinical symptoms, and more recent work has raised that estimate to 100%. The difference in rate has been attributed to varying severity, concomitant chest and head injuries in patients with polytrauma, and the lack of a verifiable diagnostic test.
The temporal relationship of symptoms to injury also remains poorly defined. Animal studies in dogs have shown pulmonary hypertension to occur within hours of injury; however, the average time to symptom onset has been shown to be 48.5 hours, with most patients showing signs and symptoms within 72 hours. Our patient developed symptoms within 6 hours of the injury and prior to any operative intervention. However, the diagnosis was not made until he experienced postoperative pulmonary and neurologic deterioration, although, in retrospect, FES was present preoperatively at 6 hours postinjury.
Certain patients with various mechanisms of injury are at higher risk of FES than others. Younger patients with multiple closed long bone fractures after a crush injury and delayed stabilization are the group that is at highest risk for developing FES. It is hypothesized that crushing mechanisms increase the soft-tissue and osseous damage, resulting in more fat globules being released into the bloodstream. Our patient was at risk for the development of FES given his young age, the long bone fracture, and the crushing mechanism.
FES often is considered a subset of acute respiratory distress syndrome (ARDS). A definitive cause has not yet been established, and 2 leading theories have been proposed: the mechanical and biochemical theories. The mechanical theory is supported by the work of Aoki et al. and Pell et al., proposing that fat cells from bone marrow are seeded into the circulatory system at the time of injury, causing direct injury to the lungs and brain. The biochemical theory states that when these same fat globules enter the respiratory system, they are broken down into free fatty acids, leading to a microvascular inflammatory response and acute lung injury. This interferes with the oxygenation of the blood and leads to hypoxemia. Mental status changes result from inflammation from the deposition of these free fatty acids in neural tissue. This has most recently been supported by Prakash et al., who showed a higher level of proinflammatory cytokines, specifically interleukin-6, in patients with polytrauma and FES at 12 hours after injury compared with those without FES. Our case highlights the multifactorial nature of FES given the early-onset presentation, which likely occurred prior to the effect of the proinflammatory cytokine cascade, with sustained and worsening symptomatology occurring later in the clinical course. Thus, the underlying mechanism of FES is likely a combination of both the mechanical and biochemical theories.
Many treatment modalities have been utilized, including heparin and corticosteroid therapy, with little support in the literature. Current treatment includes pulmonary support, management of circulatory shock, and early long-bone-fracture fixation, as indicated. Talbot and Schemitsch were the first to theorize that early fracture stabilization could prevent FES. Later, Pinney et al. showed that early rather than late intramedullary nailing of femoral fractures decreased the rate of FES. Even with timely stabilization, our patient manifested early symptoms and, despite operative stabilization, experienced continued clinical progression. Some may suggest that these worsening clinical symptoms may, in part, be related to treatment with a reamed intramedullary nail. However, an increase in FES has not been demonstrated with reamed or unreamed nailing versus open reduction and internal fixation. Multiple recent studies have shown no increased risk of developing or worsening FES with reamed intramedullary nailing. While Aoki et al. and Pell et al. showed the presence of fat emboli in the cardiac chambers during reamed intramedullary nailing of long bone fractures through the use of transesophageal echocardiography, no relation was elicited between the presence of emboli and FES. Reamed intramedullary nailing was chosen for our patient given the lack of increased risk of FES and the decreased rate of nonunion. The postoperative respiratory and mental deterioration in our patient suggests that a delay in definitive stabilization might have been appropriate. However, the response to pulmonary support and the excellent recovery to full function support early definitive fixation.
FES is a well-known and often devastating complication of long bone fractures in patients with polytrauma. It is important for all clinicians to be aware of the triad of hypoxia, petechial rash, and neurologic derangement while treating this subset of patients. The clinical outcomes are wide, ranging from full function without sequelae to death, with an overall mortality rate of up to 10%. To our knowledge, this case report is the first published case of FES that occurred within 6 hours of an open isolated long bone fracture in a young, healthy man with no head or chest trauma. This case of FES, which presented as early as 6 hours after injury and prior to operative intervention, brings awareness of the possibility of early-onset FES. The temporal relationship between injury and symptoms should not be used as a diagnostic criterion. Recognition and treatment are important to obtain optimal short and long-term outcomes in patients with FES.
Reference: Cronin KJ, Hayes CB, Moghadamian ED. Early-onset fat embolism syndrome: a case report. JBJS Case Connect. 2018 Apr-Jun;8(2):e44.
What is the diagnosis?
Systemic inflammatory response syndrome
Disseminated intravascular coagulation
Pneumonia with septic emboli
Posttraumatic fat embolism syndrome
Congestive heart failure


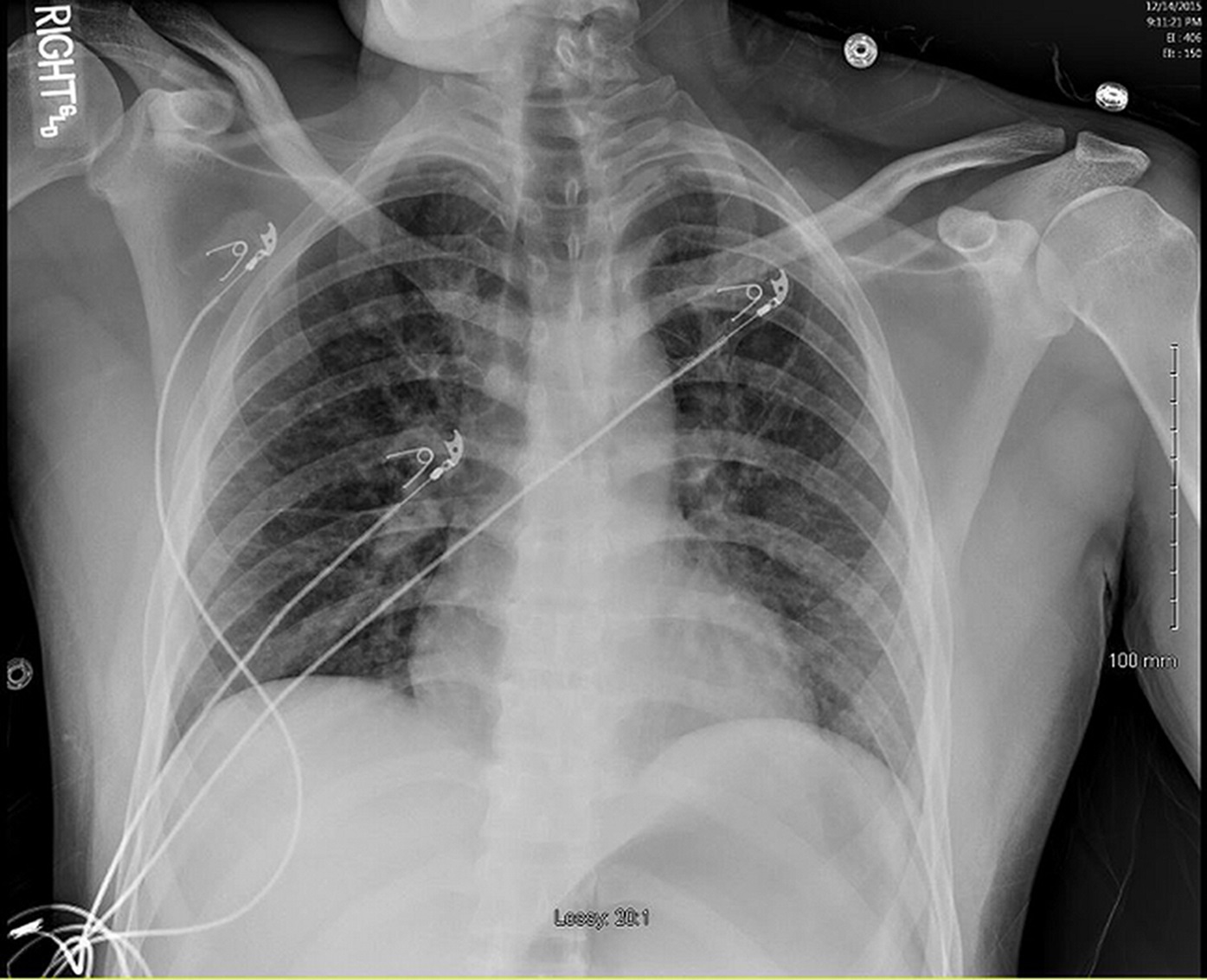
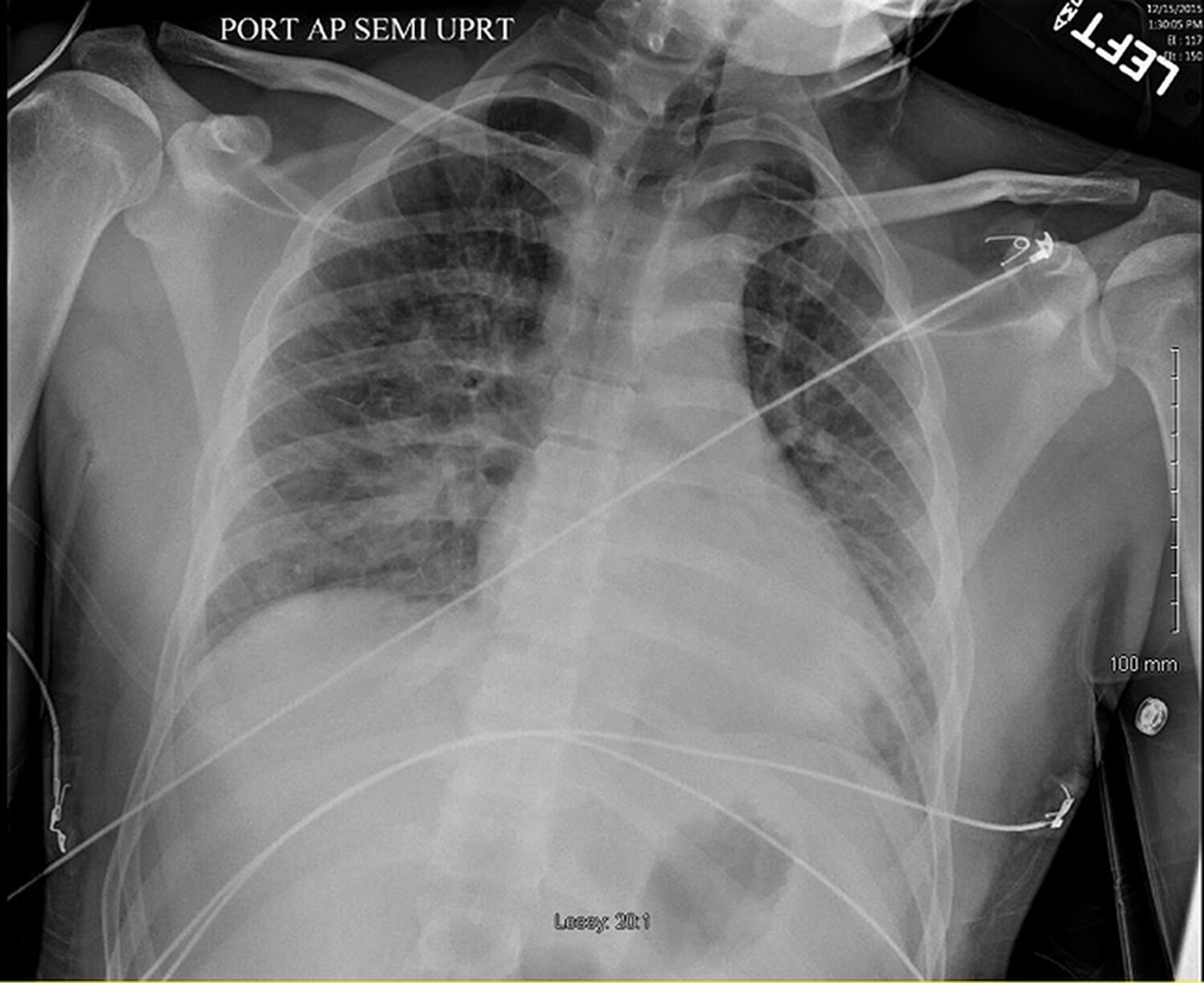

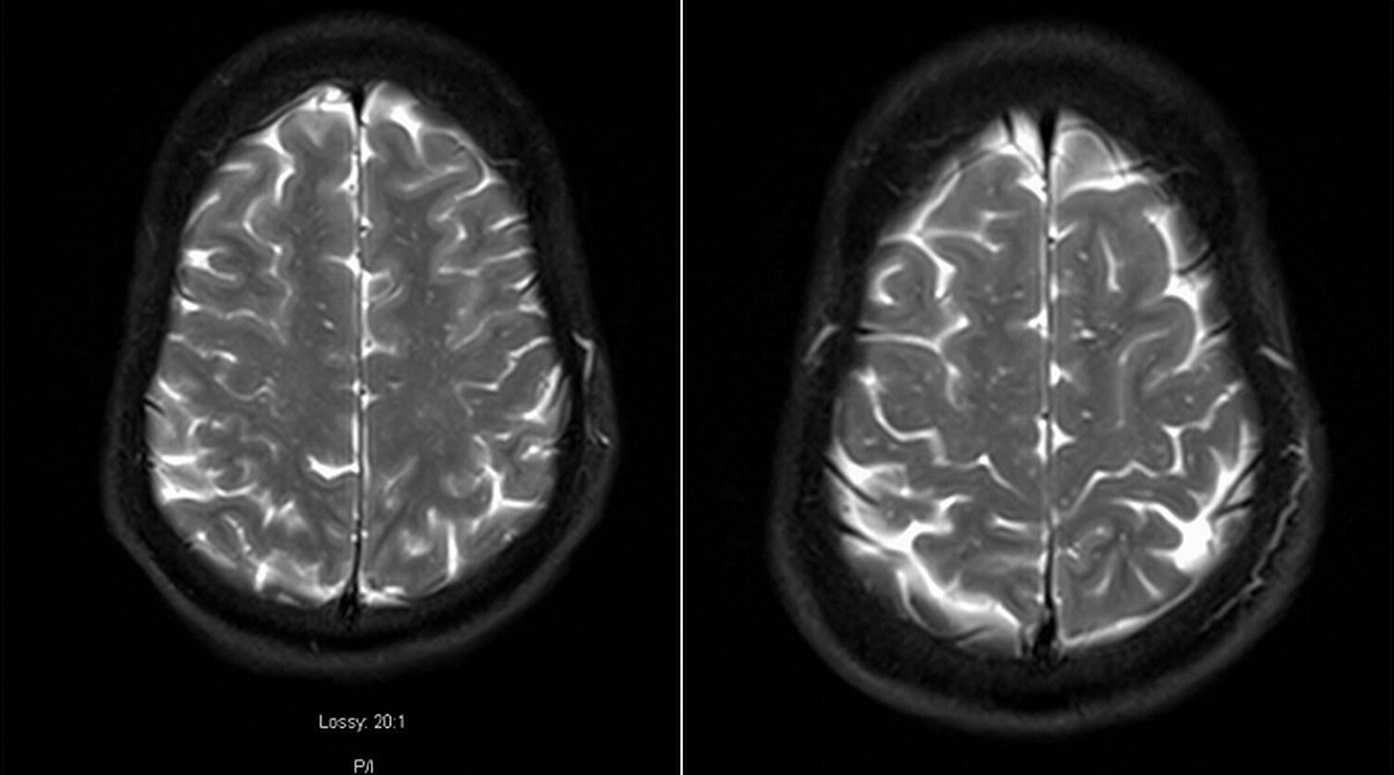
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3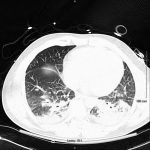 Fig. 4
Fig. 4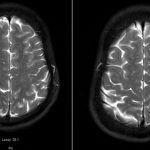 Fig. 5
Fig. 5