A 47-Year-Old, HIV-Positive Man with Wrist Swelling
October 3, 2018
A 47-year-old, right-hand-dominant, male welder with human immunodeficiency virus (HIV) noted a 1-year history of left wrist pain and swelling that had begun shortly after he had begun highly active antiretroviral therapy (HAART). When the HAART had been initiated, the patient met the criteria for acquired immune deficiency syndrome (AIDS). He had seen several different physicians over the course of that year, including an orthopaedic surgeon who had performed an intra-articular wrist corticosteroid injection for presumed osteoarthritis.
When seen in the clinic, the patient had no fevers and no systemic signs of illness. The left wrist was diffusely edematous and erythematous. Wrist motion was limited and painful. There were no open skin wounds, and the hand was well perfused. The white blood-cell count was within normal limits (6.4 × 103/μL), but the erythrocyte sedimentation rate (ESR) and the C-reactive protein (CRP) level were elevated at 46 mm/hr and 2.9 mg/dL, respectively. Radiographs of the left wrist showed advanced destruction of the distal aspect of the radioulnar, radiocarpal, intercarpal, and midcarpal joints, with cystic osseous erosions throughout the wrist and the metacarpal bases, as well as volar subluxation of the carpus (Figs. 1-A and 1-B).
We performed an open biopsy through a dorsal approach. We encountered abundant mucinous material, hyperproliferative tenosynovium, and extensive destruction of the scaphoid and the lunate. We excised the proximal carpal row and performed an extensor tenosynovectomy. Osseous destruction extended through the articular surface of the radius, which was curetted back to normal-appearing bone. Initial Gram staining and acid-fast bacilli (AFB) staining results were negative, as were the results from routine anaerobic, aerobic, and fungal culture. The histologic examination of the excised tissue is shown in Fig. 2. The infectious disease service was consulted prior to surgery and comanaged the patient during the postoperative period, but could not recommend an antibiotic regimen immediately postoperatively because of the lack of an identifiable infectious organism.
On postoperative day 14, the patient returned to the clinic with a well-healed surgical wound, but the wrist pain was persistent. At 5 weeks after surgery, he presented with 3 draining sinuses over the volar aspect of the wrist.
Five weeks after surgery, a culture specimen on AFB culture medium had exhibited some growth, but the organism could not be speciated. Based on a worsening clinical picture and a strong suspicion of atypical mycobacterial infection, the patient received ethambutol, clarithromycin, and rifampin. The HAART was never discontinued. At 4 months after surgery and 3 months after the initiation of antibiotics, the draining sinuses had resolved. On postoperative day 67, the final culture results identified the organism as Mycobacterium avium-intracellulare (MAI).
At 5 years after surgery, the patient had returned to work as a pipe fitter with minimal wrist pain. Radiographs showed no progression of bone destruction (Figs. 3-A and 3-B). He demonstrated 30° of wrist flexion and 30° of wrist extension. The HAART and suppressive antimycobacterial therapy were continued indefinitely by recommendation of the infectious disease specialist.
Proceed to Discussion >>Reference: Ward C, Milam G. Atypical mycobacterial septic arthritis of the wrist: a report of two cases. JBJS Case Connect. 2018 Apr-Jun:8(2):e42.
Because of their rarity, delay in the diagnosis and subsequent treatment of atypical mycobacterial infections continue to compromise outcomes. In the largest case series of nontuberculous mycobacterial (NTM) infections of the upper extremity, Kozin and Bishop reported that delay in diagnosis averaged 1 year from the onset of symptoms in 33 patients. The delay in diagnosis of NTM (M. kansasii) osteomyelitis of the scaphoid in an immunocompetent slaughterhouse worker after a traumatic inoculation approached 3 years. Similarly, the diagnosis of M. marinum osteomyelitis had been delayed for over a year in a patient described by Clark et al. The delay in diagnosis in our patient was 1 year from the onset of symptoms.
Even when physicians suspect an NTM infection, growing the causative organism in culture can take months. Although molecular tests for NTM exist, a positive molecular test does not indicate that NTM is the causative organism of the joint infection because these organisms often are present in immunosuppressed patients. Unfortunately, waiting for culture growth and antibiotic sensitivities remains the best treatment path.
MAI infections often have affected patients with AIDS, and typically present as pneumonia, bacteremia, and disseminated infection. MAI infections typically occur in profoundly immunosuppressed patients with very low CD4 lymphocyte counts and high viral loads. Localized infection with MAI remained relatively rare until the advent of HAART in the 1990s. Immunocompromised patients are particularly susceptible to developing deep musculoskeletal infections after the initiation of HAART in a phenomenon known as immune reconstitution inflammatory syndrome (IRIS). In these cases, opportunistic infections in patients who are infected with HIV become symptomatic because of the enhancement of immune responses to these low-virulence organisms. IRIS has been reported in cases of vertebral osteomyelitis presenting >1 year after the initiation of HAART, as well as in a case of septic arthritis of the knee with osteomyelitis of the proximal aspect of the tibia that developed 11 months after the initiation of HAART. Patients with CD4 counts of <100 cells/μL, viral loads of >105 copies/mL, and a rapid response to HAART are more at risk for IRIS, especially in the early weeks to months after beginning treatment. Our patient developed symptoms shortly after beginning HAART, although he was not diagnosed with an MAI infection for a year.
Interestingly, this patient developed draining sinuses prior to treatment with antibiotics. Yano et al. reported 1 case of MAI septic arthritis of the wrist in an immunocompetent patient who also developed a fistula at a wrist puncture site. Although perhaps not unique to MAI infection, the development of a draining sinus should raise suspicion of an atypical infection.
The duration of antibiotic treatment that is necessary to completely resolve such an infection is not known. Although we debrided as much diseased tissue as possible in our patient, we believe that complete eradication of the infected tissue would likely require amputation because resection of the wrist and replacement or arthrodesis is not recommended in the setting of infection. In 2 previously reported cases of MAI septic arthritis of the wrist in immunocompetent patients, patients completed 1 year of antibiotic treatment.
In our opinion, any patient with HIV and a history of HAART who presents with new or chronic musculoskeletal symptoms warrants a workup for atypical infection. Diagnosis requires sufficient tissue, and organisms may take several months to grow on culture. Treatment may require aggressive debridement followed by long-term culture-specific antibacterial therapy. A multidisciplinary approach with an infectious disease specialist and a surgeon can help to minimize morbidity and achieve optimal outcomes.
Reference: Ward C, Milam G. Atypical mycobacterial septic arthritis of the wrist: a report of two cases. JBJS Case Connect. 2018 Apr-Jun:8(2):e42.
What is the diagnosis?
Bone resorption secondary to corticosteroid injection
Chronic recurrent multifocal osteomyelitis
Epithelioid sarcoma
Probable atypical mycobacterial infection
Synovial sarcoma



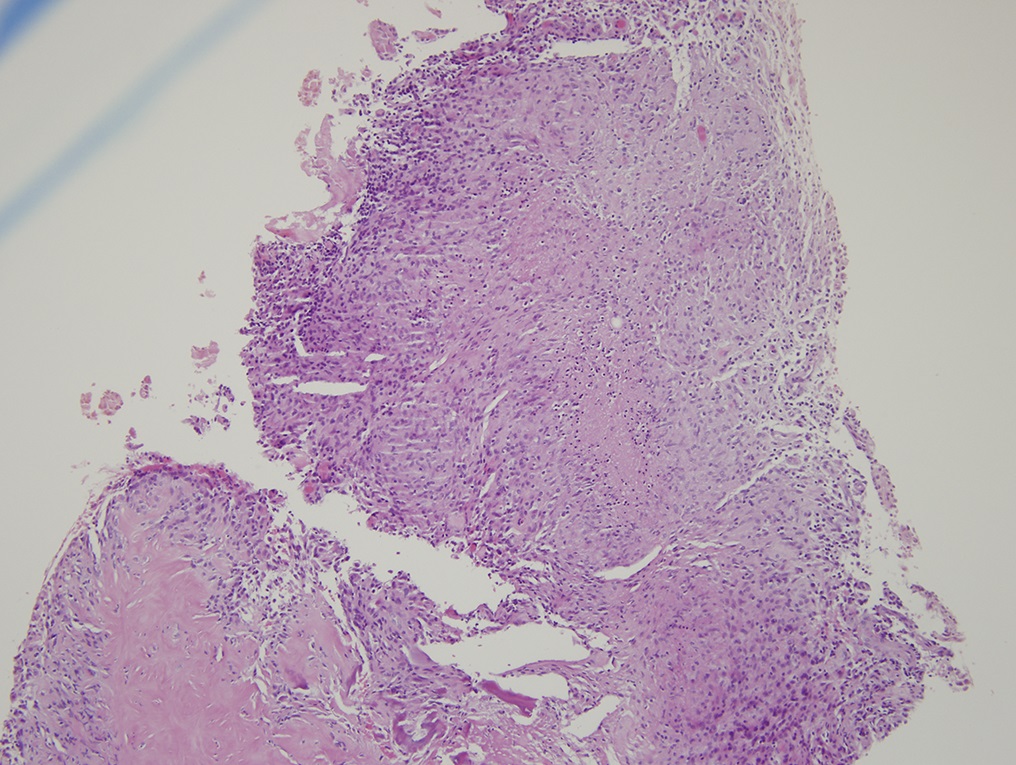
 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 2
Fig. 2 Fig. 3-A
Fig. 3-A Fig. 3-B
Fig. 3-B
