A 29-Year-Old Man with Pain and Swelling of the Elbows
November 7, 2018
A 29-year-old man who had been diagnosed with Ollier disease when he was a child previously had undergone surgery on the right calcaneus (Fig. 1). He presented with symptoms of new pain and increasing size of the elbows, the forearms, and the wrists over a 12 to 18-month period. Enlargement was most prominent bilaterally in the proximal third of the forearms (Fig. 2). He had been treated with factor VIII infusions for hemophilia A as a child, but had not received any additional treatment over the last 11 years. He did not note any recent trauma, but reported aggressive weightlifting, including biceps curls. Radiographs of both forearms revealed substantial osseous expansion and cystic changes, primarily in the radius, with secondary sclerotic changes in the ulna and the associated soft-tissue masses (Figs. 3 and 4).
The patient had a history of very minimal bleeding and no previous hemarthrosis. The basal factor VIII activity varied from 0.06 to 0.09 units/mL, in keeping with mild hemophilia A (factor VIII reference range, 0.47 to 1.7 units/mL). Laboratory studies demonstrated a normal factor IX plasma level, excluded von Willebrand disease, and were negative for a factor VIII inhibitor.
The patient had difficulty raising his arms due to the weight of the forearm masses, and reported a new onset of numbness in the right hand in the ulnar nerve distribution, with intact sensation along the median and radial nerve distributions. The decreased functional status and the neurologic symptoms in the right forearm required operative management with a planned sequentially staged approach (right forearm first). In collaboration with the hematology service, the patient was given a dose of factor VIII (50 units/kg of body weight) before the start of surgery. The factor VIII activity in the plasma measured 0.09 units/mL before the infusion and 1.23 units/mL 30 minutes later.
After the arm was elevated and a tourniquet was applied, a 29-cm incision was made over the fluctuant area of the mass. The skin was elevated with full-thickness flaps over the capsule of the mass. The capsule was incised, and approximately 1.5 L of fluid egressed under pressure from the mass, immediately decompressing the large cyst and leaving residual capsule and redundant tissue. Fibrinous tissue and a hematoma that were found at the base of the capsule were removed using a curet and a rongeur (Fig. 5). Tissue samples were sent for pathologic evaluation (Fig. 6).
The biopsy showed organizing hemorrhage with cholesterol clefts and hemosiderin-laden macrophages with calcification, and was interpreted as a pseudotumor related to the patient’s hemophilia.
The wound was irrigated, and 2 drains were placed within the capsule and brought out of the skin on the lateral aspect of the arm. Excess capsule (approximately 200 cm2 of capsule) was removed to allow for a tight closure over the defect. Despite the extensive debridement, the remaining ulna was found to be stable to flexion and extension; therefore, additional autologous bone-grafting was not needed. Once the tourniquet was deflated, the wound began to bleed copiously. A compression dressing was applied for 10 minutes. After careful inspection, no local bleeding vessels were identified. We applied 1 g of tranexamic acid locally. Factor VIII activity was monitored postoperatively for 10 days, and additional doses (25 to 50 units/kg of body weight) were given at 12-hour intervals to maintain the activity of factor VIII in the plasma at ≥0.06 units/mL.
At 2 weeks postoperatively, the patient presented for suture removal and wound evaluation (Fig. 7). At 6 weeks, the left forearm was treated with the same surgical procedure. At the 1-year follow-up, the patient had full active range of motion (AROM) of the shoulder and elbow flexion and extension (right forearm AROM from 30° to 130°, pronation to 60°, and supination to 70°; left forearm AROM from 20° to 130°, pronation to 65°, and supination to 80°), as well as AROM in all of the digits. He also reported decreased neurapraxia of the right forearm. Although radiographs demonstrated organizing heterotopic bone formation around the osseous debulking sites of the forearm (Fig. 8), the patient had returned to all activities of daily living; the residual pseudotumors will remain under observation.
Proceed to Discussion >>Reference: Gurbani B, Igbinigie M, Koutrouvelis A, Alperin JB, Lindsey RW. Bilateral forearm pseudotumors in an adult with hemophilia A and Ollier disease: a case report. JBJS Case Connect. 2018 Jul-Sep;8(3):e54.
Pseudotumors usually present as cystic masses within muscle or bone with an insidious history of growth. Panotopoulos et al. described 3 types of pseudotumor formation in relation to muscle and bone pathology: (1) bleeding within muscle, causing nerve and blood vessel compression, without radiographic evidence of bone involvement; (2) bleeding within muscle, with extensive periosteal attachment, leading to thinning of the cortical bone; and (3) subperiosteal hemorrhage, causing periosteal stripping and cortical destruction. Our patient presented with severe pseudotumors that had components of all of these types.
Pseudotumors are commonly located in the pelvis and the lower extremities because of greater muscle mass in these regions. Gilbert identified 2 types of hemophilic pseudotumors: (1) proximal, occurring in the pelvis and/or the femur, and (2) distal, occurring in the hand and the foot. Shaheen and Alasha described a hemophilic pseudotumor of the distal parts of the radius and the ulna in a 16-year-old boy. Ahlberg described 6 cases of hemophilic pseudotumors, with 1 case in the distal aspect of the radius. To our knowledge, no other reports of forearm hemophilic pseudotumors have been reported in the literature to date.
This case report is novel in that it describes a 29-year-old man who presented with increasing bilateral forearm pain and growth of masses over a period of 12 to 18 months without a history of trauma. This patient has mild hemophilia A and no history of hemarthrosis. In the absence of hemarthrosis, it is unusual for patients to present with bilateral pseudotumors, and we believe that the symmetric cartilage tumors due to Ollier disease made our patient vulnerable to bleeding within the bone and the development of the severe pseudotumors.
A recent search of the peer-reviewed literature revealed no modern references for surgical approaches or current standardized therapy for pseudotumor formation in hemophiliacs. Ahlberg advocated a conservative approach, while Magallón et al. and Rodriguez-Merchan advised primary surgical treatment rather than prolonged substitution therapy. Nonoperative treatment options include factor VIII replacement and immobilization with hopes of regression (although this is not a true cure). An acceptable level of regression is a reduction of >25% of the pseudotumor mass when patients are treated nonoperatively. When factor VIII substitution fails to control growth, especially if that threatens an impending rupture, surgical management consists of radical extirpation, percutaneous management, exeresis and filling in of the dead cavity, irradiation, and embolization, as previously recommended by Ahlberg in 1975. Complications of untreated pseudotumors are abscess formation, a mass effect, pathologic fractures, and, occasionally, amputation of the affected limb.
To our knowledge, we have described the first case of bilateral forearm pseudotumors in the setting of Ollier disease in an adult with mild hemophilia A. Surgical management of pseudotumors is substantially challenging and requires advanced technical skills, especially in patients with chronic conditions where surrounding tissue has accommodated the mass. In our patient, we did not irradiate the dead cavity or fill it with bone graft, and it is unknown if this could have reduced the chance of the radiographic recurrence that we observed at the most recent follow-up. Postoperative complications include permanent damage to surrounding structures and extensive bleeding to the point of hemorrhagic shock. Ultimately, a treatment decision, whether nonoperative or operative, must be made by the patient and the care team on a case-by-case basis, depending on the current symptoms and the patient’s constitution.
Reference: Gurbani B, Igbinigie M, Koutrouvelis A, Alperin JB, Lindsey RW. Bilateral forearm pseudotumors in an adult with hemophilia A and Ollier disease: a case report. JBJS Case Connect. 2018 Jul-Sep;8(3):e54.
What is the diagnosis?
Chondrosarcoma in a patient with Ollier disease
Angiosarcoma
Pleomorphic liposarcoma
Chondrosarcoma arising in an osteochondroma
Hemophilic pseudotumor

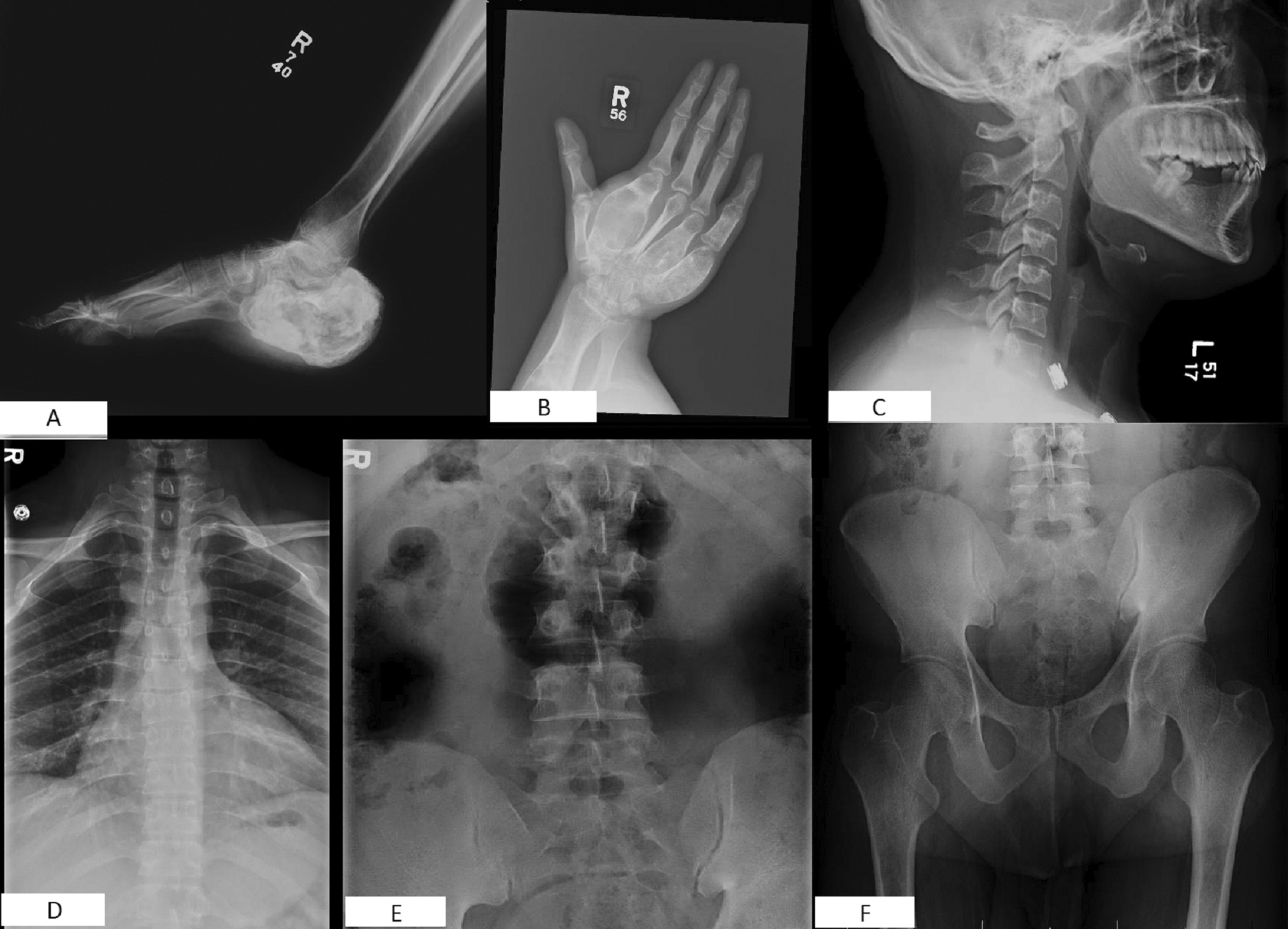


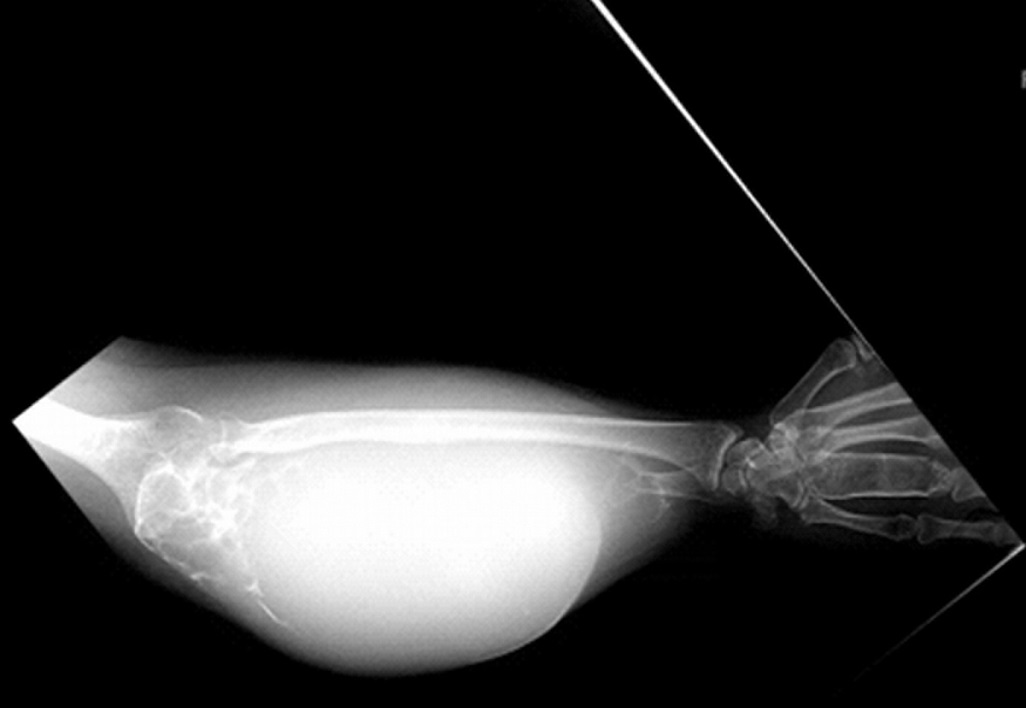
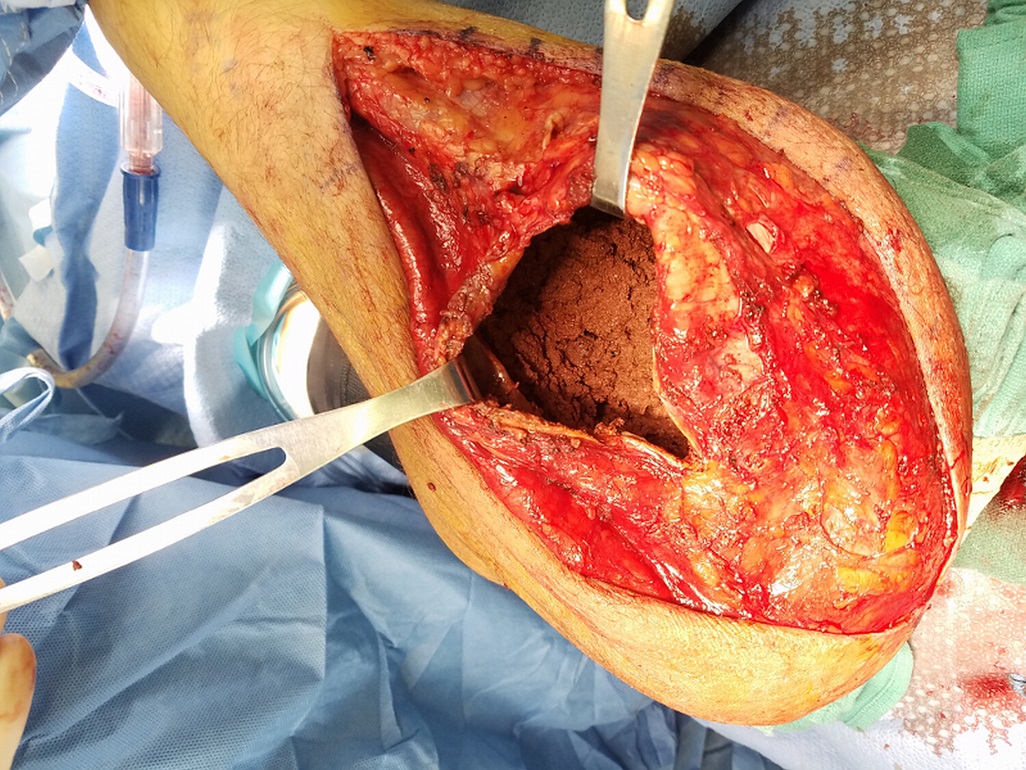
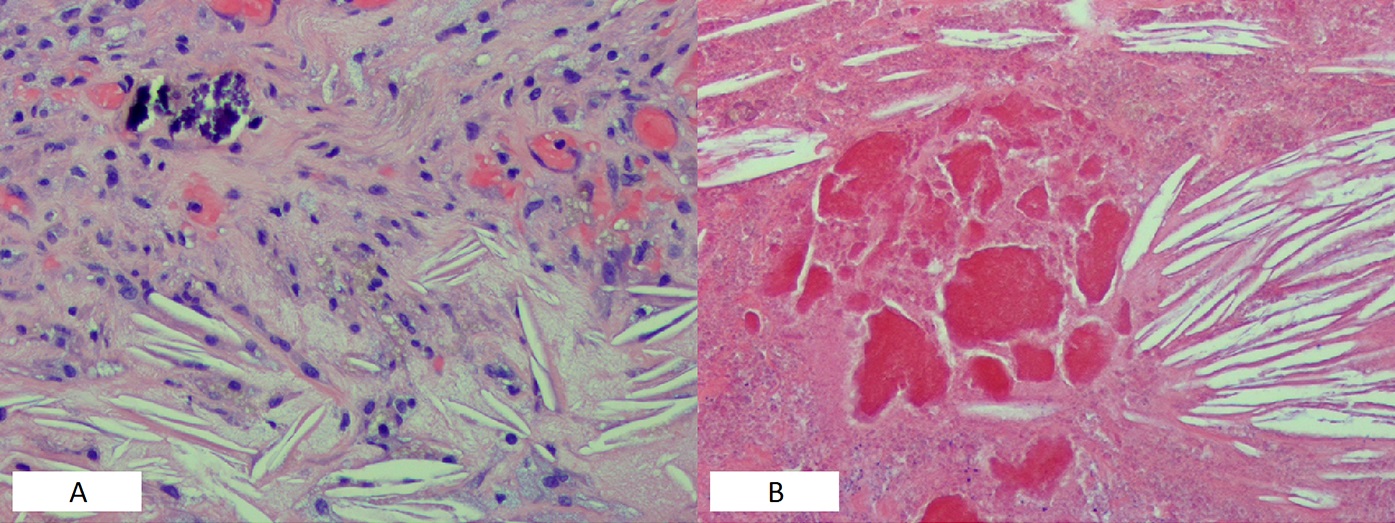
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5
Fig. 5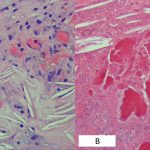 Fig. 6
Fig. 6 Fig. 7
Fig. 7 Fig. 8
Fig. 8
